 1 in 5 among all U.S. employers (22%) would likely drop health insurance coverage and let workers buy a plan through a health insurance exchange. However, most employers would expand wellness programs driven by incentives in health reform.
1 in 5 among all U.S. employers (22%) would likely drop health insurance coverage and let workers buy a plan through a health insurance exchange. However, most employers would expand wellness programs driven by incentives in health reform.
Employers’ perspectives on the Affordable Care Act/health reform are mixed, according to a survey conducted by the Midwest Business Group on Health, co-sponsored by the National Business Coalition on Health, Business Insurance and Workforce Management. Not surprisingly, these views vary by whether the firm is large (>500 employees) or small. More large employers support the creation of Health Insurance Exchanges and would expand wellness services; smaller employers aren’t as concerned about falling into the Cadillac plan segment which would be levied an excise tax.
Employers are generally supportive of changes in the law to improve quality and cost, such as creating accountable care organizations, creating patient-centered medical homes, retaining quality and performance-based payments, and using value-based designs to motivate health behavior changes.
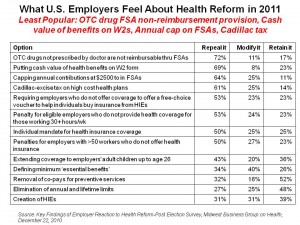
Over one-half of employers would seek to repeal several provisions, including:
- Not reimbursing OTC drugs not prescribed by a doctor through flexible spending accounts
- Putting the cash value of health benefits on the employee’s W-2 form
- Capping annual contributions at $2,500 in flexible spending accounts
- Levying Cadillac-excise tax on high-cost health plans.
Employers’ views on these and other provisions are shown in the chart based on survey data.
The survey was conducted in November and December 2010 among about 430 employer-respondents.
Health Populi’s Hot Points: The key takeaway from this survey is that health care costs continue to be top-of-mind among employers, large and small. Their embrace of value-based benefit designs and growing awareness of the role of behavioral economics and incentives to motivate positive health behaviors underlie this finding. Nearly 60% of all employers would also expand wellness programs based on incentives in the ACA — however, this is skewed by large employers, as only 32% of small employers plan to increase wellness programs. Interestingly, more large employers (67%) support the removal of co-pays for preventive services than overall employers (52%).
An intriguing mixed-result is the question of how to define “minimum essential benefits:” while 34% of employers would repeal that provision, 40% would modify it and 26% would repeal it. There’s clearly no consensus among firms on what an essential health benefit package would look like. This data point is a symbol of how, still, the U.S. continues to struggle for consensus about the role and import of health care for the nation’s health citizens.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.