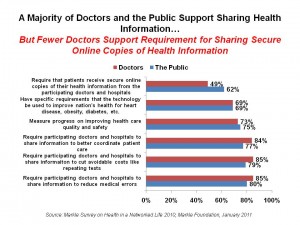
 The majority of both doctors and people in the U.S. support sharing information to improve health care in the U.S. by reducing medical errors, cutting avoidable costs, better coordinating patient care, measuring progress on improving quality and safety, and improving public health priorities such as heart disease and obesity.
The majority of both doctors and people in the U.S. support sharing information to improve health care in the U.S. by reducing medical errors, cutting avoidable costs, better coordinating patient care, measuring progress on improving quality and safety, and improving public health priorities such as heart disease and obesity.
What’s also clear is that both the public isn’t very familiar with the details of the HITECH Act which provides incentives for their doctors to adopt electronic health records. While 64% of doctors are familiar with the incentive program, only 14% of the public is.
The Markle Foundation conducted parallel surveys to measure the public’s and doctors’ views on health information technology’s (HIT) roles for improving quality, safety and cost-efficient health care in the U.S. Results of these polls are summarized in the Foundation’s report, Markle Survey on Health in a Networked Life 2010, published January 2011.
At the heart of this challenge is the central fact that 94% of doctors say patients forget or lose track of potentially important things they are told. Patients, ironically, give doctors higher marks than doctors give themselves for keeping track of the important things patients tell their doctors, Markle says.
Currently, only 5% of doctors share patient records via electronic means with patients. About one-half of doctors would prefer to share records through electronic means such as a secure web site, by email or secure messaging, or downloading to a flash drive.
Markle surveyed U.S. adults 18 and up and physicians for this project. A general population sample of 1,582 respondents to an online survey in August 2010. A total of 779 physicians completed the physician survey in August 2010; the physician sample may under-represent younger physicians and hospital-based physicians, according to the methodology discussion in Markle’s report.
Health Populi’s Hot Points: As certain members of Congress seek to weaken the overall Affordable Care Act, along with the HITECH HIT incentives to foster the adoption of electronic health records, this Markle survey firmly establishes the fact that a vast majority of both doctors and U.S. health citizens support the use of health IT to improve health care in the U.S.
There’s a potential disconnect that bears calling out in this survey: look at the top bars in the chart which shows data for the requirement that patients receive secure online copies of their health information from health providers. While 62% of the public likes this idea, 49% of doctors do. A related finding in the survey was that up to 70% of the public said patients should get a written or online summary after each doctor visit, while only 36% of doctors agreed.
There may be at least two reasons for this finding: the first is that physicians may be concerned that sharing this information could disrupt workflow and add to work load that’s not reimbursed. The right financial model for health financing could address this — such as the patient-centered medical home model (which may be why Kaiser has the largest embedded users of PHRs in the nation, along with the Veterans’ Administration). The second reason may have to do with survey methodology: Markle notes that younger physicians may be under-represented in this survey sample. Younger physicians may have a higher propensity for information sharing, especially via electronic means.
This aspect embodies patient engagement, which is part of meaningful use Stage 1 for achieving approval for receiving the incentive in the first year. When people have access to their personal health information via a personal health record, California HealthCare Foundation learned in their PHR survey that patients can become more health-engaged in their own care and treatment. Greater health engagement fosters better health outcomes. There’s wisdom in this aspect of meaningful use that leads to better individual health, better public health, and more rational use of health resources (e.g., more primary care than visits to the emergency department).




 Thank you, Trey Rawles of @Optum, for including me on
Thank you, Trey Rawles of @Optum, for including me on  I was invited to be a Judge for the upcoming
I was invited to be a Judge for the upcoming  For the past 15 years,
For the past 15 years,