 When the phrase “health care innovation” is considered, most people think about technologies like digital imaging, breakthroughs in cancer treatment, and robotic surgery.
When the phrase “health care innovation” is considered, most people think about technologies like digital imaging, breakthroughs in cancer treatment, and robotic surgery.
But before clinicians order or prescribe the use of any of those choices, there’s a cognitive process that gets them to that decision. It’s a cerebral mash-up of information, learned knowledge, and that special art of medicine embodied in the provider’s experience with patients, well-honed over time.
How can innovation improve this process? “Healthcare innovation can be defined as the introduction of a new concept, idea, service, process, or product aimed at improving treatment, diagnosis, education, outreach, prevention and research, and with the long term goals of improving quality, safety, outcomes, efficiency and costs,” according to the seminal paper, Innovation in Healthcare Delivery Systems: A Conceptual Framework, from Omachonu and Einspruch of the University of Miami. By this definition, for health providers, process innovations focus on improving health providers’ internal capabilities and improving quality of care for patients.
The Garfield Center of Healthcare Innovation, a program of Kaiser Permanente, takes a three-pronged view on innovation, shown in the diagram. The three legs of the innovation stool according to the Garfield Center are to improve, solving a problem; to transform, delivering better care; and, to spread the diffusion of the innovation.
But Donald Berwick, former head of the Centers for Medicare and Medicaid Services (CMS) and driver of health reform, reminded us that innovation for health providers is difficult — especially because although the field has rich evidence-based innovations, they disseminate slowly, “if at all,” Berwick wrote in JAMA in 1993. That was nearly a decade ago.
What slows down diffusion of innovation in health care? In her treatise on Why Innovation in Healthcare is So Hard, Regina Herzlinger, Harvard professor whom Money magazine calls “the godmother of consumer-driven health care,” has identified six areas that can make or break innovation in health care:
- Policy, especially government regulation (THINK: FDA), legislation (THINK: Affordable Care Act), and government programs (THINK: Medicaid)
- Players, who are the stakeholders in the health system who can support or block an innovation’s chance of success
- Funding, which comprises the processes for generating revenue and acquiring capita
- Technology, which encompasses advances in treatment and in making health care more efficiency and convenient
- Customers, whom Herzlinger says are increasingly engaged in health care
- Accountability, which is the “demand from vigilant consumers and cost-pressured payers” forcing safety, effectiveness, and cost-effectiveness.
 These factors are converging to force innovation in health care. Clinicians as players in the system must cope with doing more, with less resources. Funding in terms of reimbursement and insurance payment is getting squeezed. Technology in the form of electronic health records and mobile platforms has disseminated, empowering physicians with the ability to making better informed clinical decisions on-the-fly. Customers — patients — are getting more demanding and involved in both financial and clinical decisions. And, accountability, in the form of paying-for-performance, bundled payments and Accountable Care Organizations (ACOs), are diffusing in health care financing models in the U.S.
These factors are converging to force innovation in health care. Clinicians as players in the system must cope with doing more, with less resources. Funding in terms of reimbursement and insurance payment is getting squeezed. Technology in the form of electronic health records and mobile platforms has disseminated, empowering physicians with the ability to making better informed clinical decisions on-the-fly. Customers — patients — are getting more demanding and involved in both financial and clinical decisions. And, accountability, in the form of paying-for-performance, bundled payments and Accountable Care Organizations (ACOs), are diffusing in health care financing models in the U.S.
Health Populi’s Hot Points: Innovation in health care is hard. Health care’s long and winding value chain offers many opportunities to introduce innovation along that chain. A crucial link in that chain is the provider-patient relationship, and the physician’s access to just-in-time, evidence-based information that’s highly relevant to that particular patient at the point-of-care.
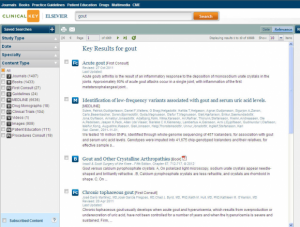 Elsevier’s ClinicalKey is one such tool that physicians can use to access that kind of information. ClinicalKey offers a straightforward, simple user interface to link clinicians, medical librarians, and researchers to the tool’s Smart Content platform that Elsevier’s team developed using semantic meaning for each and every clinical abstract. “SmartContent” is indeed an apt name for the brain in this tool, because the content includes semantically-tagged research from over 400 medical journals, 700+ books, multimedia, MEDLINE abstracts and other third-party sources. Elsevier’s innovation of the ClinicalKey reference system was developed to add value to the clinician’s cognitive process – with the objectives of driving better clinical decisions before and at the point-of-care, and indeed, throughout the patient journey.
Elsevier’s ClinicalKey is one such tool that physicians can use to access that kind of information. ClinicalKey offers a straightforward, simple user interface to link clinicians, medical librarians, and researchers to the tool’s Smart Content platform that Elsevier’s team developed using semantic meaning for each and every clinical abstract. “SmartContent” is indeed an apt name for the brain in this tool, because the content includes semantically-tagged research from over 400 medical journals, 700+ books, multimedia, MEDLINE abstracts and other third-party sources. Elsevier’s innovation of the ClinicalKey reference system was developed to add value to the clinician’s cognitive process – with the objectives of driving better clinical decisions before and at the point-of-care, and indeed, throughout the patient journey.
Faculty and medical students participating in recent ClincalKey tours at the University of Tennessee in Memphis, Case Western, and AT Still University, who had been using PubMed and other available clinical search engines appreciated ClinicalKey’s streamlined process and applications such as the Presentation Maker function which isn’t offered by existing tools in the search space.
With the growth of consumer-directed health care and accountable care for both public payers (Medicare, Medicaid) and private/commercial plans, Herzlinger’s barriers to innovation in health care are poised to fall. This will be particularly true for clinicians, who face an increasingly demanding customer base that is more info-mated and interested in collaborating as participatory patients. The last graphic illustrates how CMS envisions performance measurement for ACOs. Physicians will be charged to deliver on patient experiences, care coordination, patient safety, and population health management. Innovation of the medical practice will be the lifeblood for those practices that can survive in the accountable care era. Fast access to the highest-quality clinical information at the point-of-care is a crucial component of innovating healthcare processes in a more cost-effective, evidence-based payment environment.
Stay tuned to future Health Populi posts on ClinicalKey in November and December. Elsevier is a paid sponsor of this blog post. Stay tuned later in November for more on the ClinicalKey Experience tour and driving physician engagement.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.