Expecting health care cost increases of 5% in 2015, employers in the U.S. will focus on several tactics to control costs: greater offerings of consumer-directed health plans, increasing employee cost-sharing, narrowing provider networks, and serving up wellness and disease management programs.
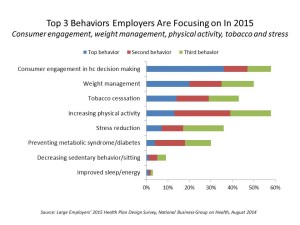
The National Business Group on Health’s Large Employers’ 2015 Health Plan Design Survey finds employers committed to health engagement in 2015 as a key strategy for health benefits. More granularly, addressing weight management, smoking cessation, physical activity, and stress reduction, will be top priorities, shown in the first chart.
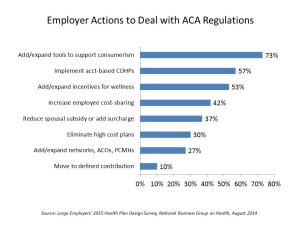
An underpinning of engagement is health care consumerism — which is the most common action cited by employers to minimize the impact of the excise tax that will hit more expensive health benefits (aka “Cadillac plans”) as part of the Affordable Care Act’s provisions. The second chart illustrates this point, along with more than half of employers looking to expand account-based health plans (CDHPs), as well as incentives to engage people in wellness programs. Both of these plans speak to the need to arm employees with tools and information that bolsters their ability to be health care consumers; these would include financial management portals that enable people to track their health spending, clinical decision making tools for prescription drugs (say, answering the patient’s question, “Is there a generic substitute for this drug and, if so, what’s the copayment?”), and for wellness, activity tracking devices, apps, and “nudging” help to stay on-course for behavior change.
Employers are experimenting with new ways to deliver health care based on quality and selectivity. Two-thirds of large employers use centers of excellence for transplants, and over 50% contract with centers for select conditions beyond transplants. About one-half of large companies offer second opinion and medical decision support services, and nearly one-half will offer telehealth services — a very fast-growth area for employer health benefits.
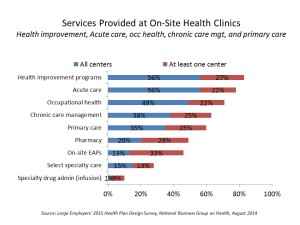 Another feature of employer-sponsored health is the growing prevalence of on-site health clinics: in 2010, 36% of large employers offered on-site clinics; in 2014, 40% offered clinics, and 14% are considering offering them. This, combined with the telehealth statistic cited in the previous paragraph, indicates that employers are looking for lower-cost settings to deliver health services that help bend cost-curves and provide convenience to workers and their dependents. These clinics go well beyond the traditional “occupational health” care of manufacturing workplaces; the new-new clinic involves biometric screenings as part of wellness programs, chronic care management (remember: weight management and smoking cessation are high priorities), and pharmacies on-site that can promote medication adherence programs for people managing chronic conditions.
Another feature of employer-sponsored health is the growing prevalence of on-site health clinics: in 2010, 36% of large employers offered on-site clinics; in 2014, 40% offered clinics, and 14% are considering offering them. This, combined with the telehealth statistic cited in the previous paragraph, indicates that employers are looking for lower-cost settings to deliver health services that help bend cost-curves and provide convenience to workers and their dependents. These clinics go well beyond the traditional “occupational health” care of manufacturing workplaces; the new-new clinic involves biometric screenings as part of wellness programs, chronic care management (remember: weight management and smoking cessation are high priorities), and pharmacies on-site that can promote medication adherence programs for people managing chronic conditions.
Health Populi’s Hot Points: While health costs continue to be top-of-mind for large employers, the 2015 outlook foresees companies getting more artful in designing health benefits. While consumer-directed health plans with medical spending accounts will become mainstream in large companies, benefits managers “get” the fact that people need support in becoming health plan literate: that is, learning to be savvy consumers of CDHPs and health savings accounts. The growth of on-site health clinics and telehealth can help people access care closer to work, and do more prevention and chronic care management in more convenient places than the doctor’s office of hospital ambulatory care center. In this respect, for (especially younger) workers in large companies, the workplace may become the de facto medical home.




 I was invited to be a Judge for the upcoming
I was invited to be a Judge for the upcoming  Thank you Team Roche for inviting me to brainstorm patients as health citizens, consumers, payers, and voters
Thank you Team Roche for inviting me to brainstorm patients as health citizens, consumers, payers, and voters  For the past 15 years,
For the past 15 years,