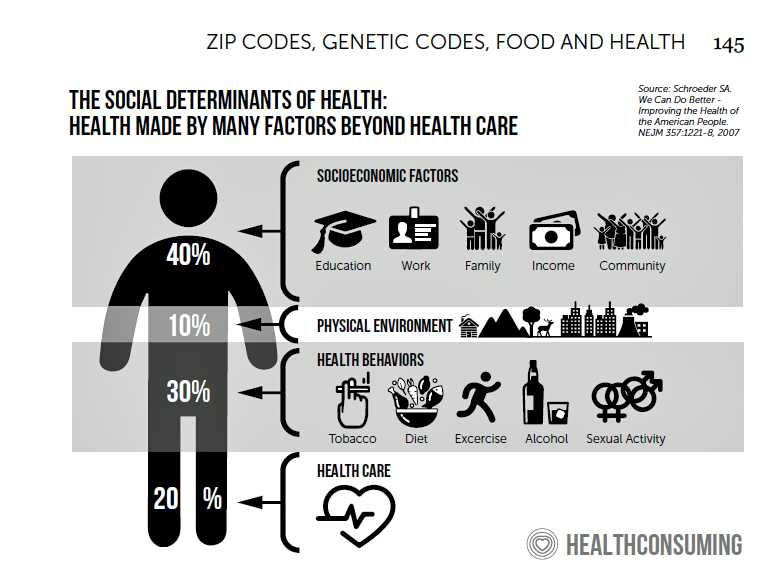
 Across the U.S., the health/care ecosystem warmly embraced social determinants of health as a concept in 2019. A few of the mainstreaming-of-SDoH signposts in 2019 were:
Across the U.S., the health/care ecosystem warmly embraced social determinants of health as a concept in 2019. A few of the mainstreaming-of-SDoH signposts in 2019 were:
- Cigna studying and focusing in on loneliness as a health and wellness risk factor
- Humana’s Bold Goal initiative targeting Medicare Advantage enrollees
- CVS building out an SDOH platform, collaborating with Unite US for the effort
- UPMC launching a social impact program focusing on SDoH, among other projects investing in social factors that bolster public health.
As I pointed out in my 2020 Health Populi trendcast, the private sector is taking on more public health initiatives as policy progress at the Federal level feels frozen. Even seemingly popular plan ideas like prescription drug pricing and coverage for pre-existing conditions can’t get traction in Congress or through the White House’s executive pen.
 Ironically, more social spending by the public sector could help address health outcomes for people, something for which we’ve had evidence for many years. This Health Affairs research published in 2015 made it clear that State spending on social health services builds citizens’ health beyond medical services. In peer OECD nations where social spending is a bigger piece of national GDP, health indicators tend to be much better than in the U.S., which is a key factor underpinning my argument for health citizenship in America in my book, HealthConsuming: From Health Consumer to Health Citizen.
Ironically, more social spending by the public sector could help address health outcomes for people, something for which we’ve had evidence for many years. This Health Affairs research published in 2015 made it clear that State spending on social health services builds citizens’ health beyond medical services. In peer OECD nations where social spending is a bigger piece of national GDP, health indicators tend to be much better than in the U.S., which is a key factor underpinning my argument for health citizenship in America in my book, HealthConsuming: From Health Consumer to Health Citizen.
In 2019, there was a major sentinel event for public health made by a huge private sector force in America: Walmart. When the company quit selling lethal bullets in its sporting goods department, this largest organization in the Fortune 100 made a huge public health impact in its own footprint and waving across Big Businesses.
 This was a sort of déjà vu moment for me, harkening back to my preceptorship conducted between grad school years at University of Michigan. I moved to Washington, DC, for a summer and took on a special project with the Department of Health and Human Services under Secretary Margaret Heckler. The goal of the research was to study the lifestyle behaviors of staff working in three federal agencies to create health-risk profiles of government employees in the Bureau of Printing, the Pension Benefit Guaranty Corporation, and the DHHS itself.
This was a sort of déjà vu moment for me, harkening back to my preceptorship conducted between grad school years at University of Michigan. I moved to Washington, DC, for a summer and took on a special project with the Department of Health and Human Services under Secretary Margaret Heckler. The goal of the research was to study the lifestyle behaviors of staff working in three federal agencies to create health-risk profiles of government employees in the Bureau of Printing, the Pension Benefit Guaranty Corporation, and the DHHS itself.
We gathered data through health risk appraisals and physical exams in government clinics for selected employees who opted into the research from the three agencies. I then analyzed the anonymized data to create health risk profiles for workers in the agencies, which had distinctively different profiles.
In one group there was an outlying statistic of gun ownership in the home.
Flash forward to Walmart, and their 2019 moment of business-and-community responsibility. See this recent essay in PLOS by Daniel Kim of Northeastern University on SDoH related to firearm-related homicides in America. Kim identified statistically significant factors related to mortality due to firearms in the U.S.: the growing gap between rich and poor in the U.S., eroding citizens’ trust in institutions, and lower economic opportunity.
We enter 2020 with companies making decisions like Walmart’s and Dick’s Sporting Goods, CVS quitting tobacco, and dozens of companies signing the Business Roundtable manifesto re-stating the group’s commitment to stakeholders beyond financial investor-shareholders – to larger communities of both local citizens and consumers.
 In this new year and decade, social determinants will be embraced beyond food, transportation and housing. One on which I focus in my book is connectivity. For several years, I’ve called out telecom connections as a social determinant: for example, in this Huffington Post column written in July 2016, I asserted that broadband is a social determinant of health. In May 2017, AMIA called for the same, and the issue is getting the traction it merits.
In this new year and decade, social determinants will be embraced beyond food, transportation and housing. One on which I focus in my book is connectivity. For several years, I’ve called out telecom connections as a social determinant: for example, in this Huffington Post column written in July 2016, I asserted that broadband is a social determinant of health. In May 2017, AMIA called for the same, and the issue is getting the traction it merits.
Connectivity can happen in other ways and bolster wellness: consider art-as-medicine. Art occasions are getting more attention in other countries outside of the U.S., such as in the U.K. where this research found Britons’ mental health improved through socializing via creative activities of all sorts. I covered this in depth in this Health Populi post earlier this year. This coverage asked and answered: “Want to live longer? Visit an art gallery.”
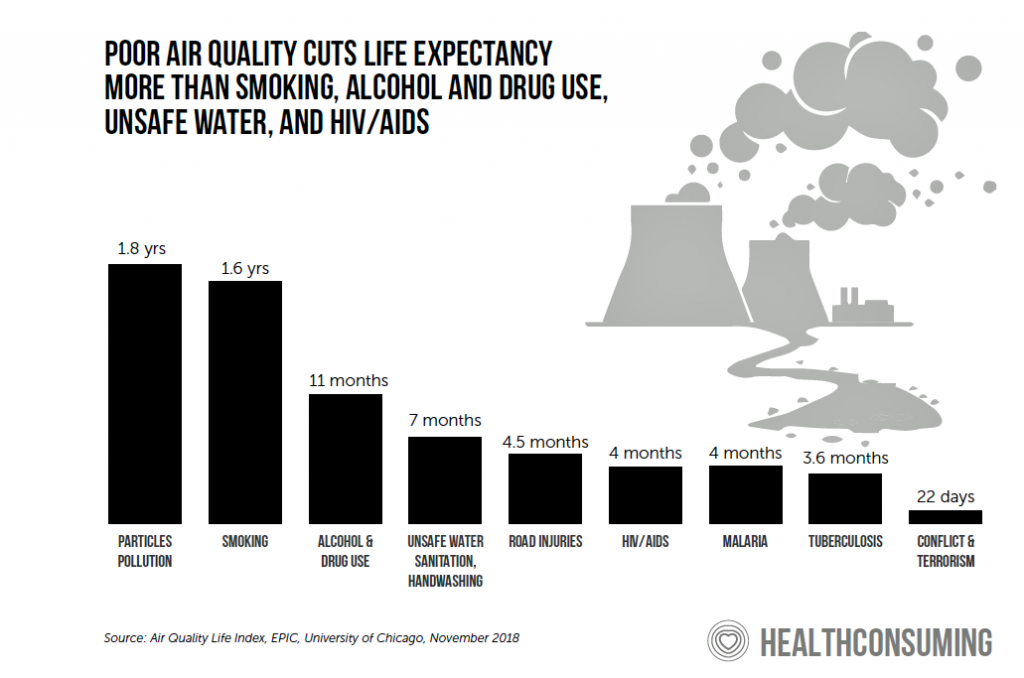
The SDoH of clean environment, and especially air quality, gained traction this past year with renewed interest in climate change and the message of the TIME person of the year, Greta Thunberg. The World Health Organization called for “prescribing” clean air for the world’s children, 90% of whom were breathing toxic air in 2018. This study, published in November 2019 by a team from Harvard, looked at admissions to hospital among Medicare enrollees exposed to higher levels of air particulates. The good news is that within a short period of time, respiratory health can improve once air quality is addressed, this study found. In Utah, Intermountain Healthcare sets a national example for health care providers to address air pollution for the benefit of the larger community beyond the hospital’s patient base.
 Intermountain is but one health care provider that will commit to social determinants beyond food and lifts for medical transport in 2020. There are new ICD-10 Z codes for social determinants that will enable billing and reimbursement for social care tied to diagnoses. Establishing a code is a good precursor to getting adoption for new-new things in U.S. health care delivery.
Intermountain is but one health care provider that will commit to social determinants beyond food and lifts for medical transport in 2020. There are new ICD-10 Z codes for social determinants that will enable billing and reimbursement for social care tied to diagnoses. Establishing a code is a good precursor to getting adoption for new-new things in U.S. health care delivery.
But let’s make sure we’re not irrationally exuberant about the private sector solving social care issues for health. Public policy trumps private projects in terms of the social, political and economic framework that determines the household economy, jobs, and income security — which is the #1 shaper of health and mortality.
 If 2020 isn’t the end all-be all year of SDoH, one thing is certain — that November 2020 will feature a Presidential election. To that point, Presidential candidate Mayor Pete Buttigieg has proposed a National Health Equity Strategy featuring “Health Equity Zones,” part of his Douglass Plan to address health disparities. Named after the Marshall Plan that rebuilt Europe after World War II, the Douglass Plan’s goal in the words of Mayor Pete’s website is to, “dismantle old systems and structures that inhibit prosperity and build new ones that will unlock the collective potential of Black America.”
If 2020 isn’t the end all-be all year of SDoH, one thing is certain — that November 2020 will feature a Presidential election. To that point, Presidential candidate Mayor Pete Buttigieg has proposed a National Health Equity Strategy featuring “Health Equity Zones,” part of his Douglass Plan to address health disparities. Named after the Marshall Plan that rebuilt Europe after World War II, the Douglass Plan’s goal in the words of Mayor Pete’s website is to, “dismantle old systems and structures that inhibit prosperity and build new ones that will unlock the collective potential of Black America.”
I conclude this last Health Populi post of 2019 with a link to Harold Paz’s CNN Opinion column highlighting Heisman Trophy winner Joe Burrow’s speech on food security as a social determinant of health in his home state of Ohio. “Coming from southeast Ohio, it’s a very impoverished area and the poverty rate is almost two times the national average. There’s so many people there that don’t have a lot, and I’m up here for all those kids in Athens and Athens County that go home to not a lot of food on the table, hungry after school. You guys can be up here, too.” Connecting with fans and aficionados, Joe raised $300,000 for his local food pantry.
Indeed, we can be “up here, too,” doing our part for our communities’ health.
I wish you health, joy, peace, food on your table and love in your heart in the new year. Love is, after all, the ultimate social determinant of health.




 I was invited to be a Judge for the upcoming
I was invited to be a Judge for the upcoming  Thank you Team Roche for inviting me to brainstorm patients as health citizens, consumers, payers, and voters
Thank you Team Roche for inviting me to brainstorm patients as health citizens, consumers, payers, and voters  For the past 15 years,
For the past 15 years,