In health care, one of the “gifts” inspired by the coronavirus pandemic was the industry’s fast-pivot and adoption of digital health tools — especially telehealth and more generally the so-called “digital front doors” enabling patients to access medical services and personal work-flows for their care.
Two years later, Experian provides a look into The State of Patient Access: 2023.
You may know the name Experian as one of the largest credit rating agencies for consumer finance in the U.S. You may not know that the company has a significant footprint in health care and financial technology. This results of the consumer and provider surveys combines those corporate interests, discussed in this report.
Start with the definition of patient access. In this study, Experian is speaking more to digital workflows for patients and providers — in particular, those tasks that occur before a care encounter, as shown in the first graphic: these include,
- Scheduling an appointment
- Pre-registering and registering
- Coverage verification and estimate of costs
- Pre-care payment services, and
- Patient communication.
So how do folks feel about progress for digital front doors in health care?
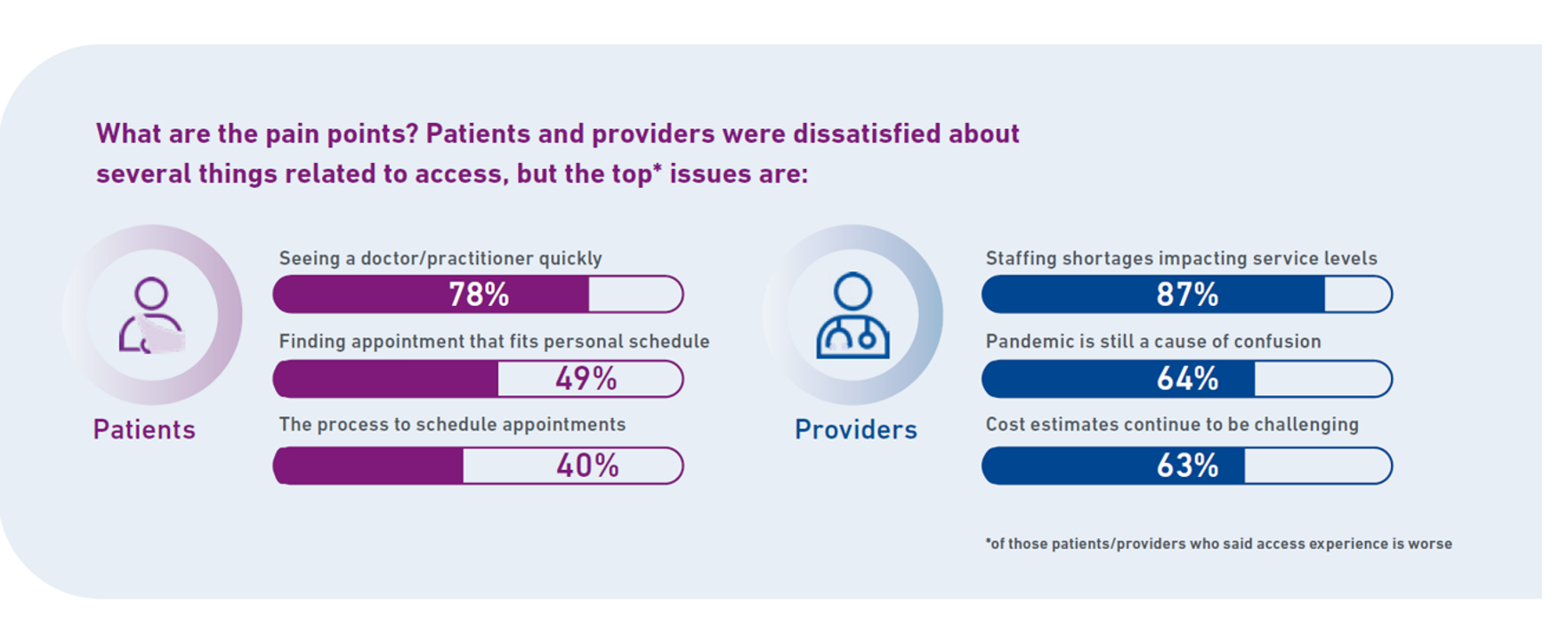
Check out the second chart of patients’ and providers’ pain points.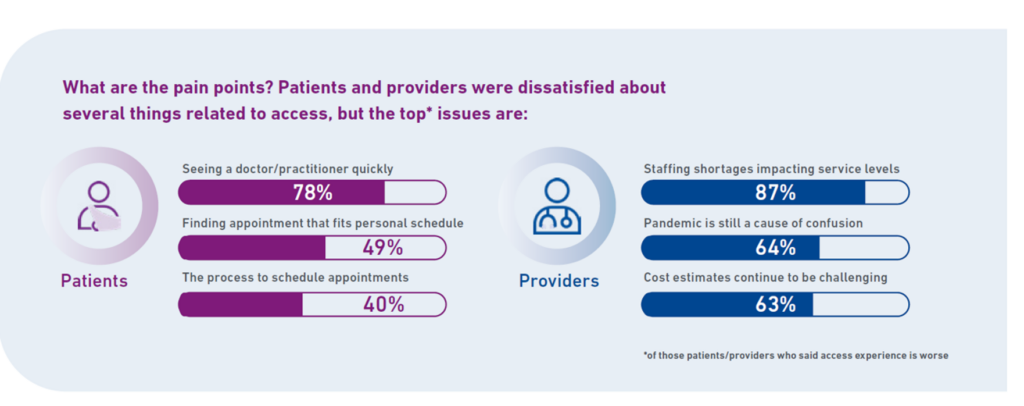
For patients, the most painful access issue for most is seeing a clinician quickly, which 4 in 5 health consumers point to. Then, 1 in 2 patients say finding an appointment that fits their schedule is a top pain issue, followed by appointment schedule processes.
For providers, staffing shortages, post-pandemic confusion, and challenges with estimating costs for patients continue to be pain points in the process of digital transformation.
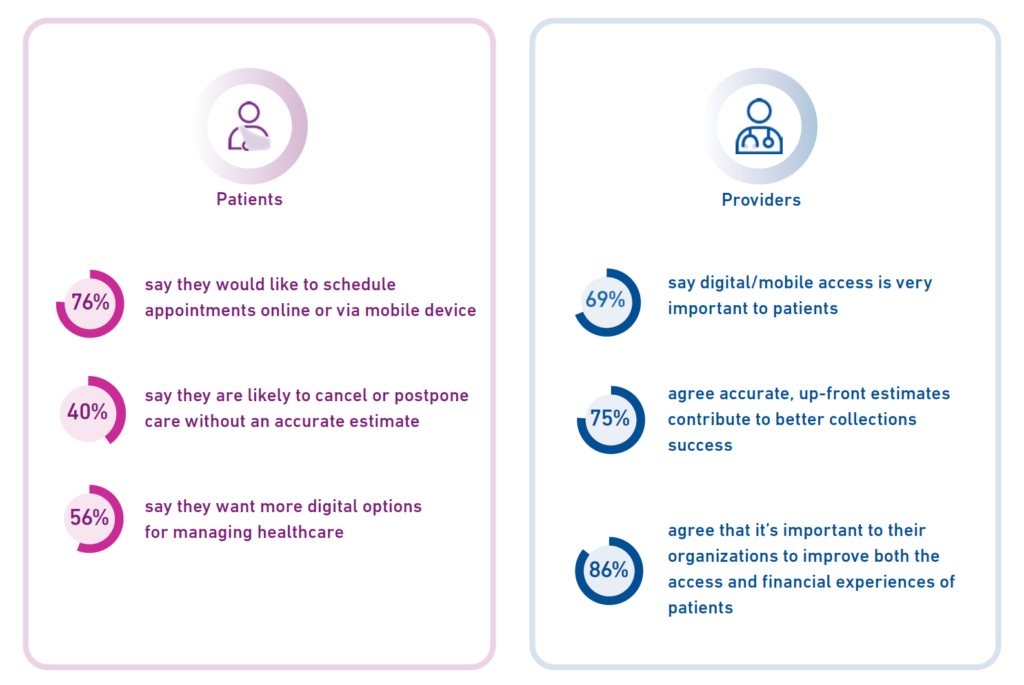
To better align, consumer-patients are looking to digital/mobile as a basic expectation for health care engagement with providers. Their personal preferences for digital front doors are first, phones, followed by portals, in-person mode, email, text, and finally snail mail.
Thus we see in this chart that three quarters of patients would like to schedule appointments online or via mobile devices. And, over one-half of patients want more digital options for managing their care.
What do people want from digital transformation for their health care experiences? pre-care cost estimates that are accurate (personalized based on their own health insurance plans), payment plans for paying medical bills over time, digital payment options (think: Venmo meets medical bills), a multi-purpose portal, and mobile access for both administrative tasks and care — that is, virtual care/telehealth.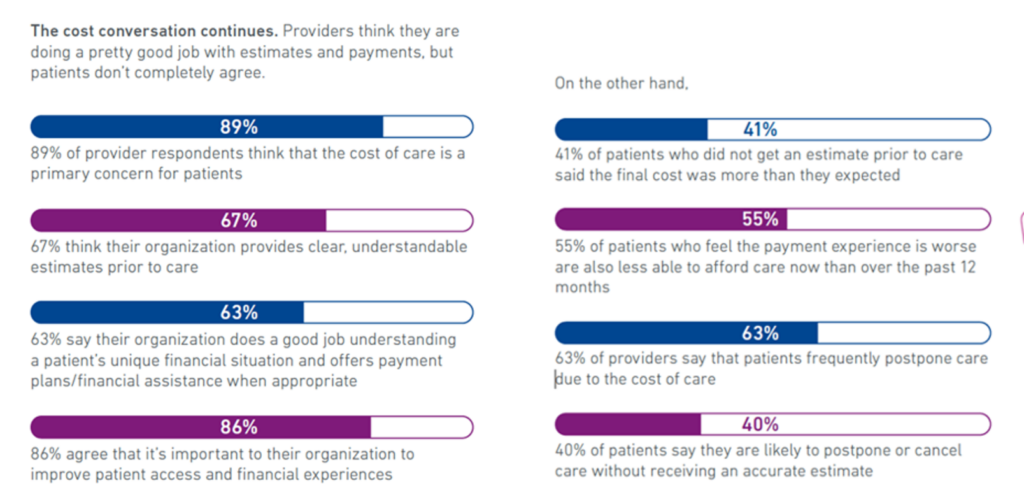
Health Populi’s Hot Points: As Experian puts the situation and experience-gap, “the cost conversation continues.” The gap is that most providers think they’re doing a “pretty good job” estimate patients’ costs, but a minority of patients didn’t get a very good estimate — resulting in surprise bills or higher costs than planned-for.
And, 63% of providers said patients frequently postpone care due to cost.
A just-breaking report from the CDC explores the demographics of patients between 18 and 64 years of age (that is, not children and not folks of Medicare-age) who avoid prescription drugs due to cost, in Characteristics of Adults Age 18-64 Who Did Not Take Medication as Prescribed to Reduce Costs: United States, 2021.
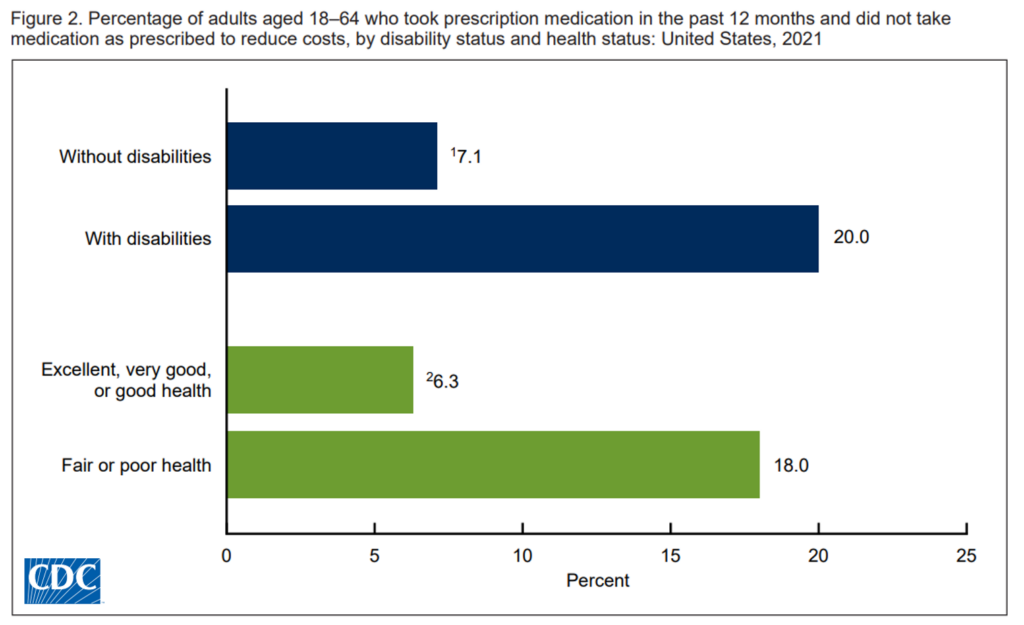
The CDC asserts that high costs of prescription drugs can limit health consumers’ access to medications and lead to people not taking meds as prescribed — presenting risks for further illness and adverse events.
Patients as health consumers trying to save medical costs try to save money by skipping doses, taking less medication (dose) than prescribed, or delaying filling an Rx.
The proportion of U.S. adults who avoid meds due to cost varies by different patient characteristics including:
- Gender, with more women avoiding medicines due to cost than men
- Age, with adults 30-44 years of age at greater risk of medicines-avoidance due to cost
- Race/ethnicity, where 10.4% of Black Americans did not take meds according to the prescription due to cost compared with 7.4% of White Americans and 9.7% of Hispanic Americans, and,
- People with disabilities nearly three times as likely to avoid medications due to cost — as well as 18% of those in fair or poor health in this situation versus 6.3% of people in excellent, very good, or good health.
So as we continue to ideate, design, and build out digital front doors, we should remember that not all patients access doors the same way, nor do they uniformly face the same cost calculus — which profoundly shapes how, when, and where they might access that digital on-ramp.




 I was invited to be a Judge for the upcoming
I was invited to be a Judge for the upcoming  Thank you Team Roche for inviting me to brainstorm patients as health citizens, consumers, payers, and voters
Thank you Team Roche for inviting me to brainstorm patients as health citizens, consumers, payers, and voters  For the past 15 years,
For the past 15 years,