Consumers Feel More Respect from Personal Care and Grocery Brands Than Pharma or Insurance
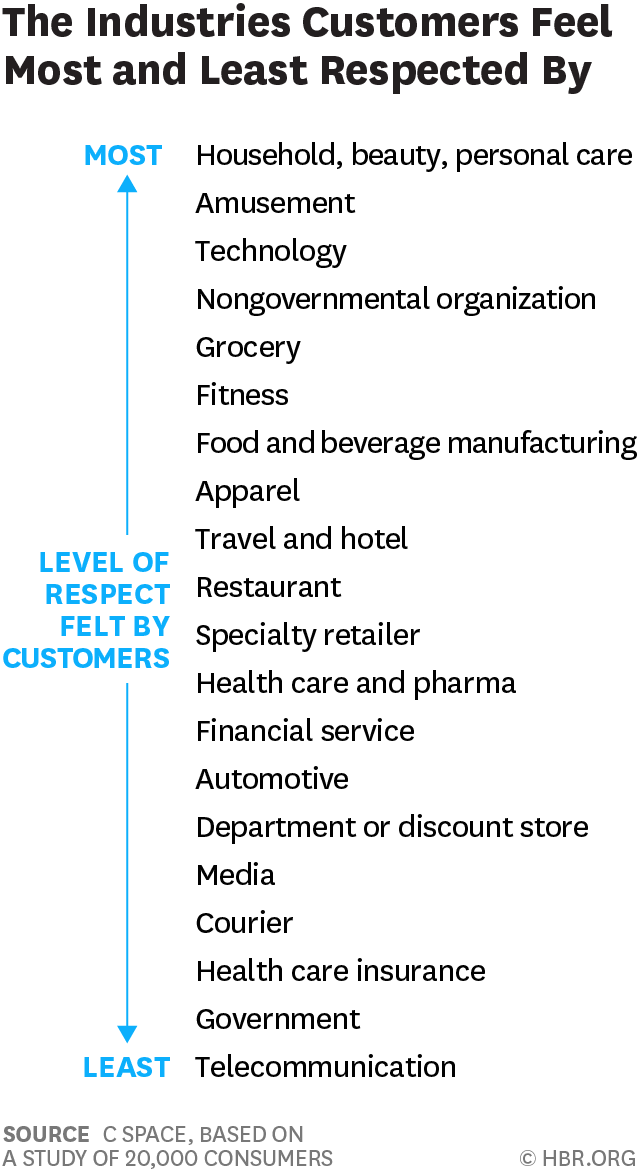
People feel like get-no-respect Rodney Dangerfield when they deal with health insurance, government agencies, or pharma companies. Consumers feel much more love from personal care and beauty companies, grocery and fitness, according to a brand equity study by a team from C Space, published in Harvard Businss Review. As consumer-directed health care (high deductibles, first-dollar payments out-of-pocket) continues to grow, bridging consumer trust and values will be a critical factor for building consumer market share in the expanding retail health landscape. Nine of the top 10 companies C Space identified with the greatest “customer quotient” are adjacent in some way to health:
Looking for Amazon in Healthcare
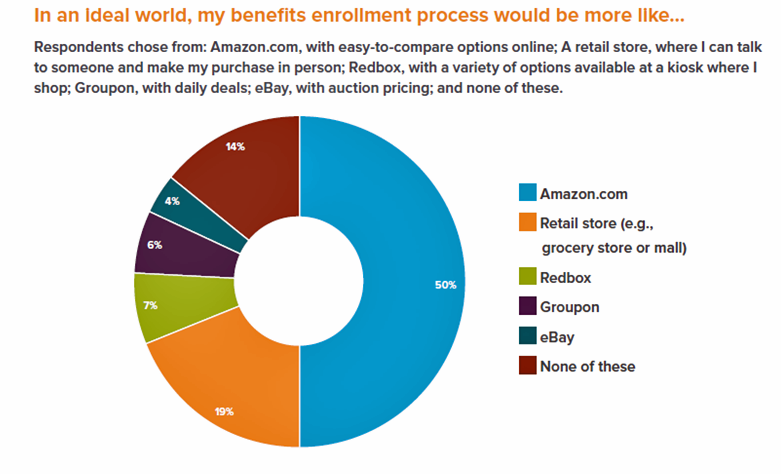
Consumers have grown accustomed to Amazon, and increasingly to the just-in-time convenience of Amazon Prime. Today, workers who sign onto employee benefit portals are looking for Amazon-style convenience, access, and streamlined experiences, found in the Aflac Workforces Report 2016. Aflac polled 1,900 U.S. adults employed full or part time in June and July 2016 to gauge consumers’ views on benefit selections through the workplace. Consumers have an overall angst and ennui about health benefits sign-ups: 72% of employees say reading about benefits is long, complicated, or stressful 48% of people would rather do something unpleasant like talking to their ex or
The Average Monthly Health Plan Premium in the U.S. Hit $885 in 2016
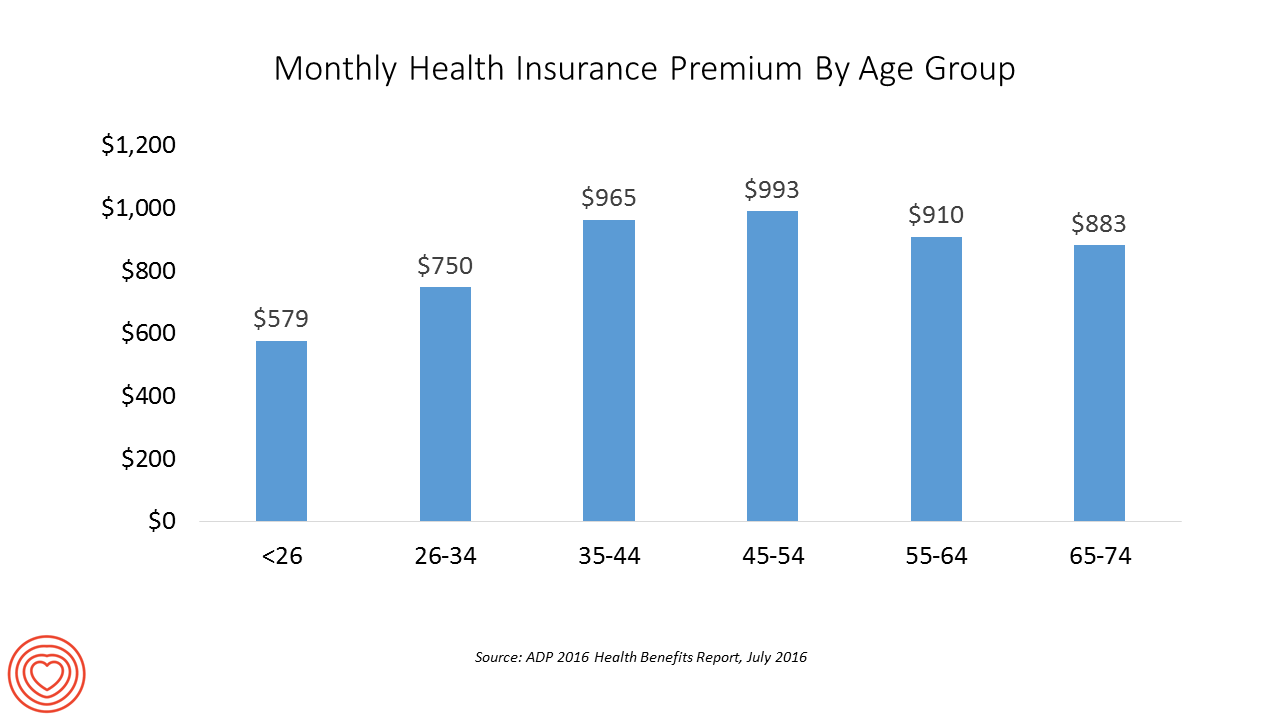
Three years after the launch of the Affordable Care Act (ACA), the big picture of employer-sponsored health benefits in the U.S. show stability, with modest changes in costs being kept in check by a growing younger workforce, according to the 2016 ADP Annual Health Benefits Report. Roughly 9 in 10 employees in large companies are eligible to participate in health insurance plans at the workplace, with two-thirds of people participating, shown in the chart. Younger people, under 26 years of age, have much lower participation rates than those over 26, with many staying on their parents’ plans (taking advantage of
In Healthcare, Pharmacists and Doctors Most Trusted. Insurance Execs and Congress? Not.
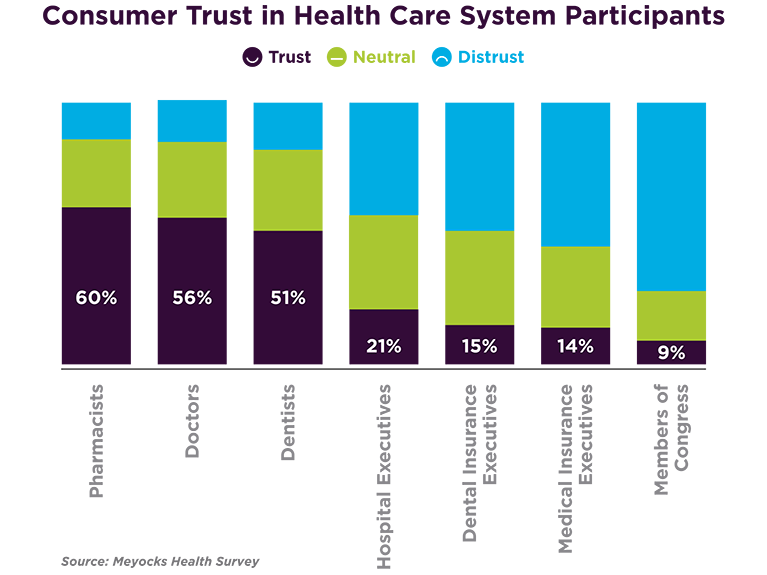
When consumers consider the many stakeholder organizations in healthcare, a majority trust pharmacists first, then doctors and dentists. Hospital and health insurance execs, and members of Congress? Hardly, according to a survey from Meyocks, a marketing consultancy. Meyocks conducted the survey via email among 1,170 US adults, 18 years of age and older. This survey correspondends well with the most recent Gallup Poll on most ethical professions, conducted in December 2015. In that study, pharmacists, nurses and doctors come out on top, with advertisers (“Mad Men”), car salespeople, and members of Congress at the bottom, as shown in the second
The State of Health Benefits in 2016: Reallocating the Components
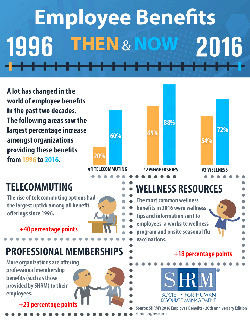
Virtually all employers who offer health coverage to workers extend health benefits to all full-time employees. 94% offer health care coverage to opposite-sex spouses, and 83% to same-sex spouses. One-half off health benefits to both opposite-sex and same-sex domestic partners (unmarried). Dental insurance, prescription drug coverage, vision insurance, mail order prescription programs, and mental health coverage are also offered by a vast majority (85% and over) of employers. Welcome to the detailed profile of workplace benefits for the year, published in 2016 Employee Benefits, Looking Back at 20 Years of Employee Benefits Offerings in the U.S., from the Society for Human
PwC’s “Behind the Numbers” – Where the Patient Stands
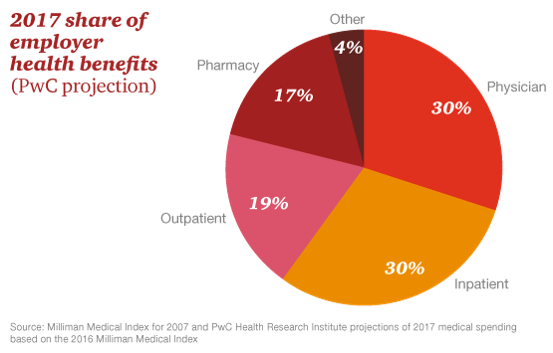
The growth of health care costs in the U.S. is expected to be a relatively moderate 6.5% in 2017, the same percentage increase as between 2015 and 2016, according to Medical Cost Trend: Behind the Numbers 2017, an annual forecast from PwC. As the line chart illustrates, the rate of increase of health care costs has been declining since 2007, when costs were in double-digit growth mode. Since 2014, health care cost growth has hovered around the mid-six percent’s, considered “low growth” in the PwC report. What’s driving overall cost increases is price, not use of services: in fact, health care
Most Americans Favor A Federally-Funded Health System
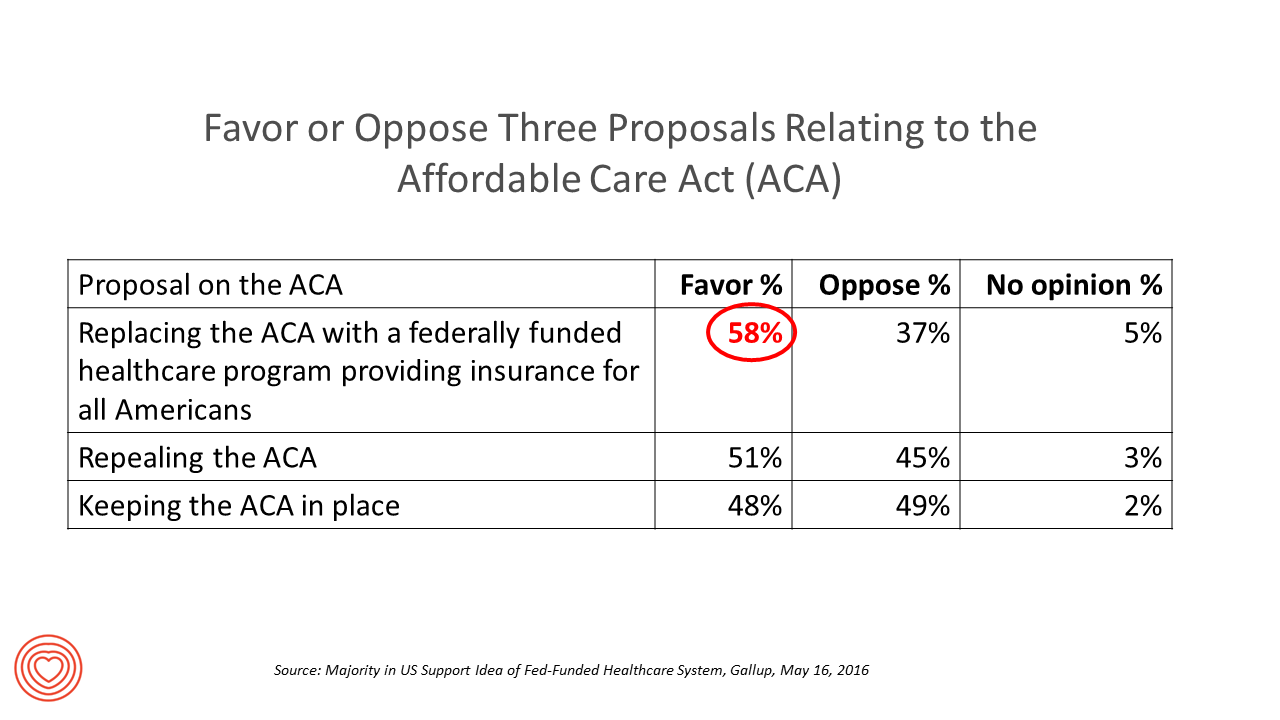
6 in 10 people in the US would like to replace the Affordable Care Act with a national health insurance program for all Americans, according to a Gallup Poll conducted on the phone in May 2016 among 1,549 U.S. adults. By political party, RE: Launch a Federal/national health insurance plan (“healthcare a la Bernie Sanders”): Among Democrats, 73% favor the Federal/national health insurance plan, and only 22% oppose it; 41% of Republicans favor it and 55% oppose it. RE: Repeal the ACA (“healthcare a la Donald Trump”): Among Democrats, 25% say scrap the ACA, and 80% of Republicans say to do
Costs and Connection At the Core of Consumers’ Health-Value Equations
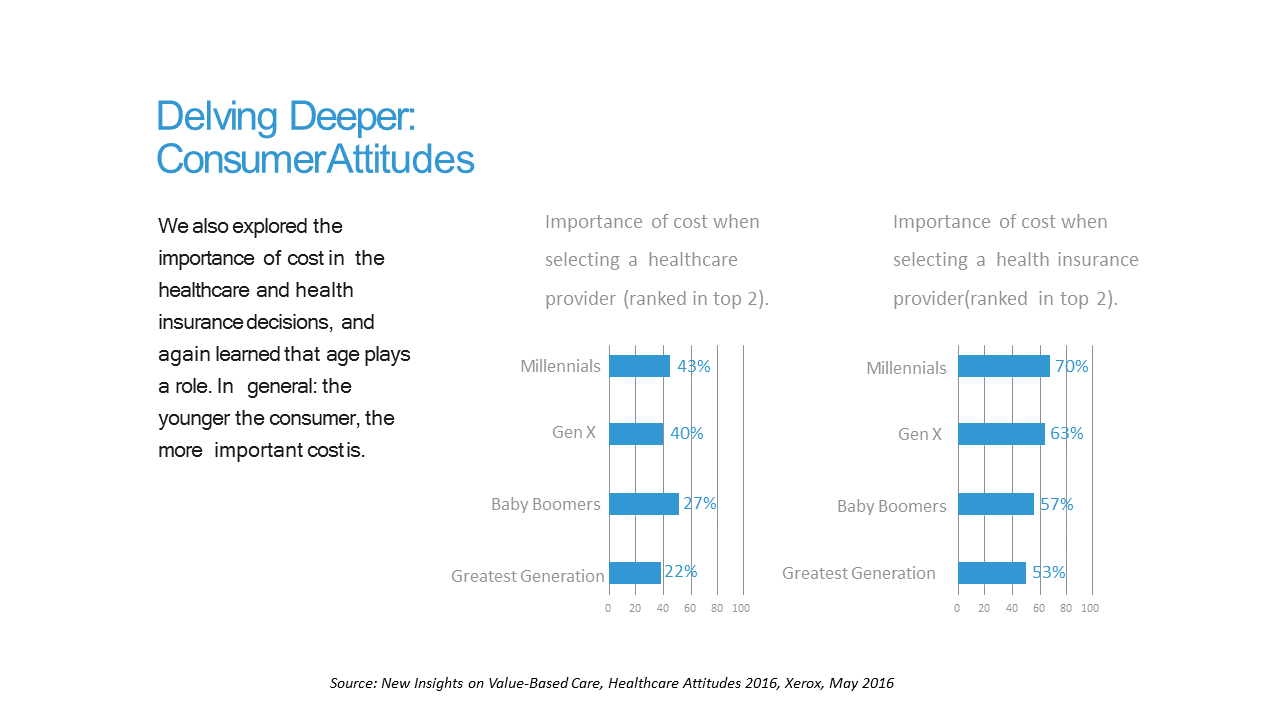
Cost ranks first among the factors of selecting health insurance for most Americans across the generations. As a result, most consumers are likely to shop around for both health providers and health plans, learned through a 2016 Xerox survey detailed in New Insights on Value-Based Care, Healthcare Attitudes 2016. The younger the consumer, the more important costs are, Xerox’s poll found, shown in the first chart. Thus, “shopping around” is more pronounced among younger health consumers — although a majority people who belong to Boomer and Greatest Generation cohorts do shop around for both health providers and health insurance plans —
Generation Gaps in Health Benefit Engagement
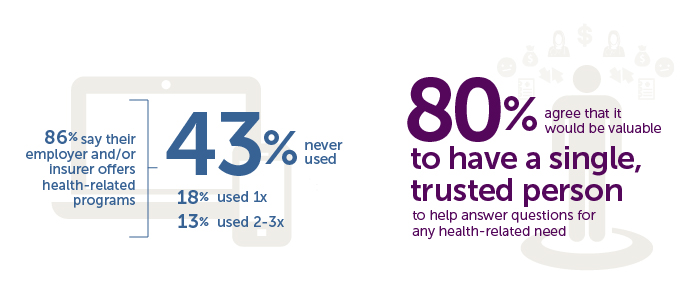
Older workers and retirees in the U.S. are most pleased with their healthcare experiences and have the fewest problems accessing services and benefits. But, “younger workers [are] least comfortable navigating U.S. healthcare system,” which is the title of a press release summarizing results of a survey conducted among 1,536 U.S. adults by the Harris Poll for Accolade in September 2015. Results of this Accolade Consumer Healthcare Experience Index poll were published on April 12, 2016. Accolade, a healthcare concierge company serving employers, insurers and health systems, studied the experiences of people covered by health insurance to learn about the differences across age
Behavioral Economics in Motion: UnitedHealthcare and Qualcomm

What do you get when one of the largest health insurance companies supports the development of a medical-grade activity tracker, enables data to flow through a HIPAA-compliant cloud, and nudges consumers to use the app by baking behavioral economics into the program? You get Motion from UnitedHealthcare, working with Qualcomm Life’s 2net cloud platform, a program announced today during the 2016 HIMSS conference. What’s most salient about this announcement in the context of HIMSS — a technology convention — is that these partners recognize the critical reality that for consumers and their healthcare, it’s not about the technology. It’s about
Tying Health IT to Consumers’ Financial Health and Wellness

As HIMSS 2016, the annual conference of health information technology community, convenes in Vegas, an underlying market driver is fast-reshaping consumers’ needs that go beyond personal health records: that’s personal health-financial information and tools to help people manage their growing burden of healthcare financial management. There’s a financial risk-shift happening in American health care, from payers and health insurance plan sponsors (namely, employers and government agencies) to patients – pushing them further into their role as health care consumers. The burden of health care costs weighs heavier on younger U.S. health citizens, based on a survey from the Xerox Healthcare
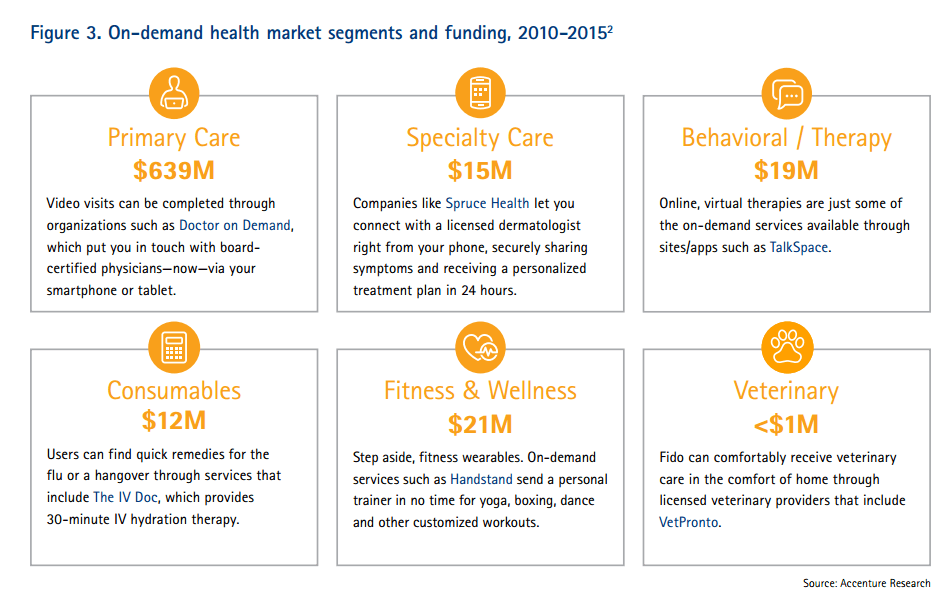
Telehealth Comes of Age at HIMSS 2016
Telehealth will be in the spotlight at HIMSS 2016, the biggest annual conference on health information technology (HIT) that kicks off on 29th February 2016 in Las Vegas – one of the few convention cities that can handle the anticipated crowd of over 50,000 attendees. Some major pre-HIMSS announcements relate to telehealth: American Well, one of the most mature telehealth vendors, is launching a software development kit (SDK) which will enable The new videoconferencing option can simultaneously connect patients with multiple physicians and specialists, and the SDK is designed to enable users to incorporate telemedicine consults into patient portals and
U.S. National Health Spending Up Due to More People Covered and Higher Drug Costs
National health spending in American grew by 5.3% in 2014, hitting the $3 trillion mark. This represented an up-tick nearly twice the growth rate of 2.9% in 2013, the slowest rate of growth in 55 years, according to the latest analysis of the U.S. health economy published by Health Affairs. The first chart illustrates the factors that contribute to that 5.3% growth in health spending. The two largest factors were medical prices and so-called “residual use and intensity.” The medical price increase portion was 1.8% in 2014, up from 1.3% in 2013. The use and intensity component was attributable to
51% of Americans Say It’s Government’s Responsibility To Provide Health Insurance
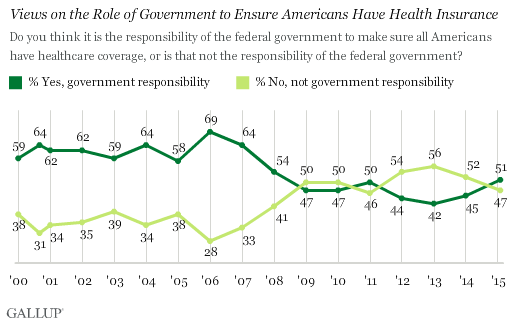
For the first time since 2008, a majority of Americans say government is responsible for ensuring that people have health insurance. The first chart shows the crossing lines between those who see government-assured health insurance in the rising dark green line in 2015, and people who see it as a private sector responsibility. The demographics and sentiments underneath the 51% are important to parse out: people who approve of the Affordable Care Act are over 3x more likely to believe in government sponsoring health insurance versus those who disapprove, 80% compared with 26%. The demographic differences are also striking, detailed
In 2016 Prescription Drugs Will Be The Fastest-Growing Component of Healthcare Costs
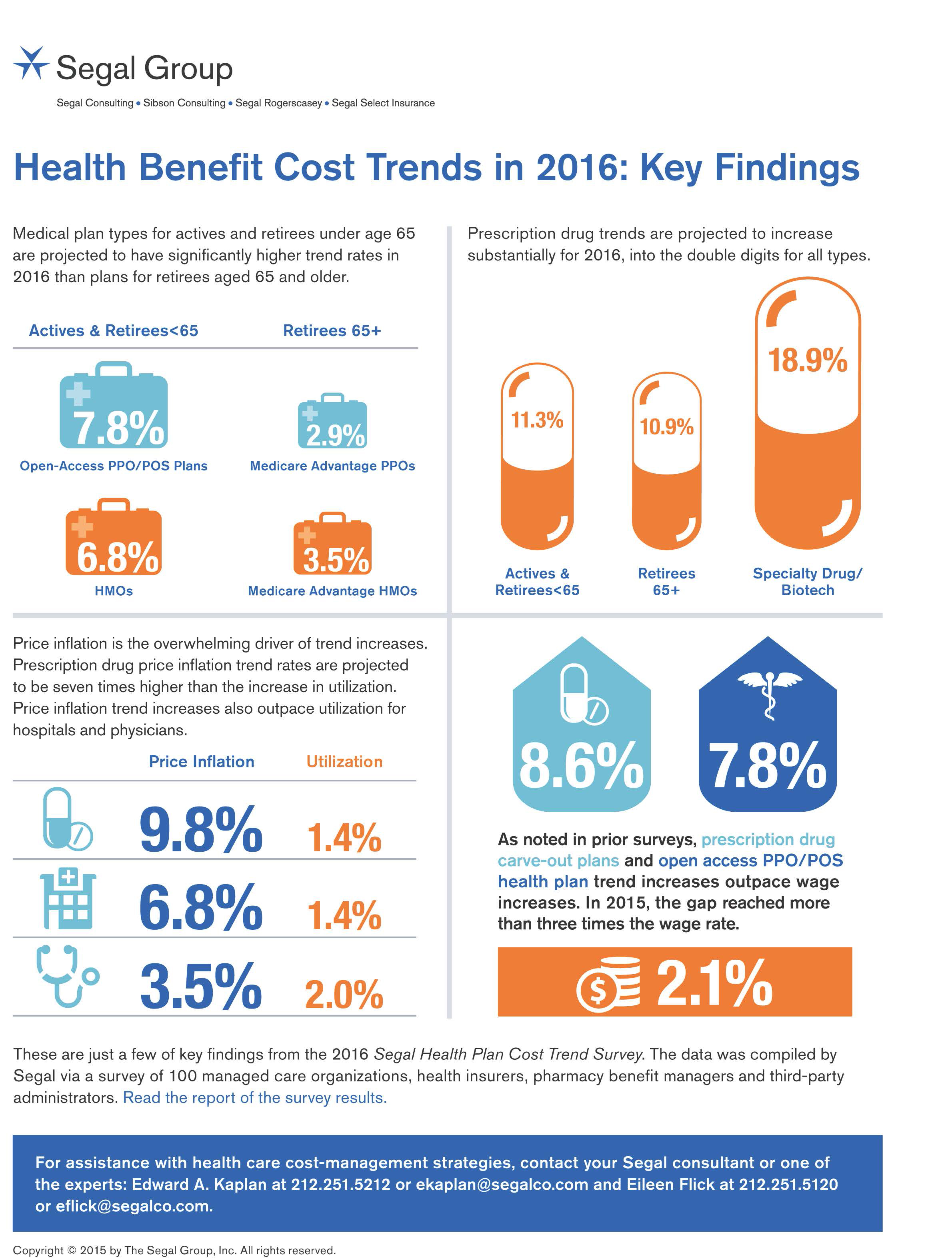
In 2016, prescription drug trend will rise over 11%. In contrast, medical trend growth for high-deductible health plans is expected to be 8%, hospital services 8.2%, and physician services 5.5%, according to the 2016 Segal Health Plan Cost Trend Survey released in September 2015. By definition, “trend” is the forecast of per capita health insurance claims cost increases that incorporate many factors include price inflation, utilization, government-mandated benefits, and new therapies and technologies. Consider the upper right portion of the infographic which illustrates Segal’s data: the 3 “capsule” diagrams show that specialty drug trend is anticipated to be 18.9% in
From Pedometers to Premiums in Swiss Health Insurance
A Switzerland-based health insurance company is piloting how members’ activity tracking could play a role in setting premiums. The insurer, CSS, is one of the largest health insurance companies in the country and received a “most trusted general health insurance” brand award in 2015 from Reader’s Digest in Switzerland. The company is conducting the pilot, called the MyStep project, with volunteers from the Federal Institute of Technology in Zurich and the Unviersity of St. Gallen. According to an article on the program published in the Swiss newspaper The Local, “the pilot aims to discover to what extend insured people are
A Company’s Healthy Bottom Line Requires Healthy Employees
“What is the meaning of health to our businesses?” asked Dr. Thomas Parry of the Integrated Benefits Institute (IBI) at a dinner last night, convened by the Pittsburgh Business Group on Health on the eve of the organization’s annual meeting being held today in Steel City. I was fortunate to attend the dinner and hear Dr. Parry speak; I will be addressing the meeting today on the topic, “Building a Better Health Consumer.” The IBI is researching the direct link between the top line of a healthy employee base and healthy workers’ impacts on the bottom line. A report will be
Employers pushing consumerism for health benefits in 2016
This is the dawning of the Age of Consumer-Driven Health, the tipping point of which has been passed. The data point for this assertion comes from the National Business Group on Health‘s annual 2016 Large Employers’ Health Plan Design Survey. The tagline, “reducing costs while looking to the future,” suggests some of the underlying tactics employers will use to manage their financial burden of providing health insurance to workers. That burden will continue to shift to employees and their dependents in the form of greater cost-sharing: for premiums, co-pays and co-insurance, and the hallmark of consumer-driven health plans (CDHPs): high(er) deductibles.
Coverage and price before brand for health plan shoppers
When Americans shop for health insurance (and they do – more, later in the post), they look most for covering major medical expenses, prescription drugs, preventive care, and price. Less important is the brand of the plan, or its high ratings. Valence Health surveyed 524 U.S. consumers in June 2015 to learn how healthcare shoppers feel about health insurance and health reform. The results are published in the report, U.S. Attitudes Toward Health Insurance and Healthcare Reform in August 2015. Key findings in the study were that: Price and coverage come before all other factors in evaluating health plans 73%
Telehealth goes retail
In the past couple of weeks, a grocery store launched a telemedicine pilot, a pharmacy chain expanded telehealth to patients in 25 states, and several new virtual healthcare entrants received $millions in investments. On a parallel track, the AMA postponed dealing with medical ethics issues regarding telemedicine, the Texas Medical Association got stopped in its tracks in a case versus Teladoc, and the Centers for Medicare and Medicaid Services (CMS) issued a final rule for the Medicare Shared Savings Program that falls short of allowing Accountable Care Organizations (ACOs) to take full advantage of telehealth services. These events beg the
It’s still the prices, stupid – health care costs drive consumerism
“It’s the prices, stupid,” wrote Uwe Reinhardt, Gerald F. Anderson and colleagues in the May 2003 issue of Health Affairs. Exactly twelve years later, three reports out in the first week of June 2015 illustrate that salient observation that is central to the U.S. healthcare macroeconomy. Avalere reports that spending on prescription drugs increased over 13% in 2014, with half of the growth attributable to new product launches over the past two years. Spending on pharmaceuticals has grown to 13% of overall health spending, and the growth of that spending between 2013-14 was the fastest since 2001. In light of
Purchase of wearable fitness trackers expected to grow in 2015, but one-half of Americans would “never” buy one
Headphones and smartphones are the top two electronics products U.S. consumers intend to purchase in 2015. But the emerging consumer electronics categories of wearable fitness trackers, smart watches, and smarthome devices (especially “smart” thermostats) are positioned to grow, too, in 2015, according to the 17th Annual CE Ownership and Market Potential Study from the Consumer Electronics Association (CEA). Wearable trackers have an installed base of about 17 million devices in the U.S., with 11% of U.S. households intending to purchase a tracker in 2015 — 6 percentage points up from 2014 (about a 50% increase over 2014). There are about 6 million smart
Supersize Rx: the impact of specialty drug spending and Hep C in 2014
The number of people in the U.S. spending over $100,000 a year on prescription drugs tripled in 2014, according to Super Spending: U.S. Trends in High-Cost Medication Use, from The Express Scripts Lab. Express Scripts is a pharmacy benefits management company that manages over one billion prescriptions a year. The company analyzed prescription drug claims for 31.5 million health plan members for this study, in commercially insured, Medicare, and Medicaid plans. The big-dollar story in 2014 was Hepatitis C, with a relatively small patient population but a super-sized drug spend as the first chart shows: a very tall blue bar (Rx
Consumers seek retail convenience in healthcare financing and payment
Health care consumers face a fragmented and complicated payment landscape after receiving services from hospitals and doctors, and paying for insurance coverage. People want to “view their bills, make a few clicks, pay…and be done,” according to Jamie Kresberg, product manager at Citi Retail Services, a unit of Citibank. He’s quoted in Money Matters: Billing and payment for a New Health Economy from PwC’s Health Research Institute. The healthcare service segment most consumers are satisfied with when it comes to billing and payment is pharmacies, who score well on convenience, affordability, reliability, and seamless transactions – with only transparency being
#OwnYourHealth: Health is everywhere, even underground
Living my mantra of Health is Everywhere, where we live, work, play, pray, and shop, I am always on the lookout for signs of health in my daily life. Today I’m in Washington, DC, speaking on a webinar led by the National Council on Patient Information and Education (NCPIE), discussing the findings in a survey of U.S. adults on self-care health care – my shorthand for healthcareDIY. And the hashtag for the webinar also speaks volumes: #OwnYourHealth. Here’s the link to the survey resources. On my walk from Farragut North Metro station to a nearby office where the meeting will take place,
Health = love. Care = love. Healthcare? Meh
Bruce Broussard, CEO of Humana, forgot the charger for his smartwatch on a business trip. Stopping into a consumer electronics store, he was struck by the options he faced of various wearable technologies. He ended up buying a new watch, which he uses for exercise tracking. “Technology is such an important part of the direction of health care,” Broussard told the HIMSS 2015 audience in his keynote address on 14 April 2015. But Broussard was quick to point out to the thousands of technology geeks that comprise HIMSS’s membership that improving the health/care system isn’t just about technology: “we have
John Hancock flips the life insurance policy with wellness and data
When you think about life insurance, images of actuaries churning numbers to construct mortality tables may come to mind. Mortality tables show peoples’ life expectancy based on various demographic characteristics. John Hancock is flipping the idea life insurance to shift it a bit in favor of “life” itself. The company is teaming with Vitality, a long-time provider of wellness tools programs, to create insurance products that incorporate discounts for healthy living. The programs also require people to share their data with the companies to quality for the discounts, which the project’s press release says could amount to $25,000 over the
Workers at work for the health benefits but absent when it comes to talking costs
As much as the Affordable Care Act is bolstering health insurance rolls for the uninsured, people who have enjoyed health insurance at work continue to highly value that benefit, according to a survey from Benz Communications and Quantum Workplace published April 2015. Based on a national sample of over 2,000 employees surveyed in October 2014 about workplace benefits. The research re-confirms the long-term reality of workers working in America for the health benefit. Benz/Quantum note that 89% of workers say health benefits play a part in remaining on-the-job, and half say the health benefit is a “major” part of remaining
Consumers trust retailers to manage health as much as health providers
40% of U.S. consumers trust Big Retail to manage their health; 39% of U.S. consumers trust healthcare providers to manage their health. What’s wrong with this picture? The first chart shows the neck-and-neck tie in the horse race for consumer trust in personal health management. The Walmart primary care clinic vs. your doctor. The grocery pharmacy vis-a-vis the hospital or chain pharmacy. Costco compared to the chiropractor. Or Apple, Google, Microsoft, Samsung or UnderArmour, because “digitally-enabled companies” are virtually tied with health providers and large retailers as responsible health care managers. Welcome to The Birth of the Healthcare Consumer according
Transparency in health care: not all consumers want to look
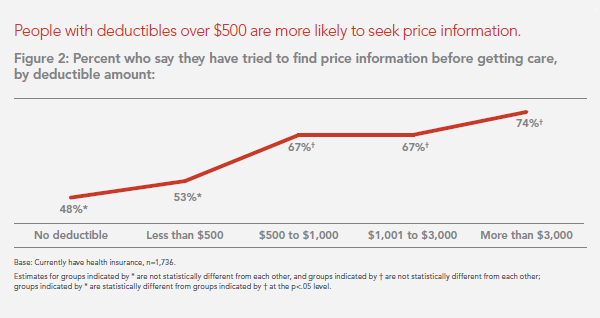
Financial wellness is integral to overall health. And the proliferation of high-deductible health plans for people covered by both public insurance exchanges as well as employer-sponsored commercial (private sector) plans, personal financial angst is a growing fact-of-life, -health, and -healthcare. Ask any hospital Chief Financial Officer or physician practice manager, and s/he will tell you that “revenue cycle management” and patient financial medical literacy are top challenges to the business. For pharma and biotech companies launching new-new specialty drugs (read: “high-cost”), communicating the value of those products to users — clinician prescribers and patients — is Job #1 (or #2,
The Affordable Care Act As New-Business Creator
While there’s little evidence that the short-term impact of the Affordable Care Act has limited job growth or driven most employers to drop health insurance plans, the ACA has spawned a “cottage industry” of health companies since 2010, according to PwC. As the ACA turned five years of age, the PwC Health Research Institute led by Ceci Connolly identified at least 90 newcos addressing opportunities inspired by the ACA: Supporting telehealth platforms between patients and providers, such as Vivre Health Educating consumers, such as the transparency provider HealthSparq does Streamlining operations to enhance efficiency, the business of Cureate among others
Value is in the eye of the shopper for health insurance
While shopping is a life sport, and even therapeutic for some, there’s one product that’s not universally attracting shoppers: health insurance. McKinsey’s Center for U.S. Health System Reform studied people who were qualified to go health insurance shopping for plans in 2015, covered by the Affordable Care Act. McKinsey’s consumer research identified six segments of health insurance plan shoppers — and non-shoppers — including 4 cohorts of insured and 2 of uninsured people. The insureds include: Newly-insured people, who didn’t enroll in health plans in 2014 but did so in 2015 Renewers, who purchased health insurance in both 2014 and
Humana and Weight Watchers Partner in Weight Loss for Employers
More employers are recognizing the link between workers who may be overweight or obese on one hand, and health care costs, employee engagement and productivity on the other. As a result, some companies are adopting wellness programs that focus on weight loss as part of an overall culture of health at the workplace. Humana and Weight Watchers are the latest example of two health brands coming together to address what is one of the toughest behavior changes known to humans: losing weight. Humana will extend access to Weight Watchers for the health plan’s enrollees in an integrated wellness program. The program
Health care costs still top financial problems for Americans
“Health care spending grows at lowest-ever rate,” USA Today celebrated in their December 3, 2014 headline. The announcement was drawn from national health spending data gleaned from an annual report from the Centers for Medicare and Medicare Services (CMS), which tallied U.S. health spending at $2.9 trillion. From the bird’s-eye view, slowing healthcare cost growth is indeed good news. But from the point-of-view of consumers’ own pockets, health care costs are rising. And, a survey published today by Gallup points to this reality: that people in American say the most important financial problem they face is healthcare costs, tied for first place
People in consumer-directed health plans are — surprise! — getting more consumer-directed
People with more financial skin in the health care game are more likely to act more cost-consciously, according to the latest Employee Benefits Research Institute (EBRI) poll on health engagement, Findings from the 2014 EBRI/Greenwald & Associates Consumer Engagement in Health Care Survey published in December 2014. Health benefit consultants introduced consumer-directed health plans, assuming that health plan members would instantly morph in to health care consumers, seeking out information about health services and self-advocating for right-priced and right-sized health services. However, this wasn’t the case in the early era of CDHPs. Information about the cost and quality of health care services was scant,
Health IT Forecast for 2015 – Consumers Pushing for Healthcare Transformation
Doctors and hospitals live and work in a parallel universe than the consumers, patients and caregivers they serve, a prominent Chief Medical Information Officer told me last week. In one world, clinicians and health care providers continue to implement the electronic health records systems they’ve adopted over the past several years, respond to financial incentives for Meaningful Use, and re-engineering workflows to manage the business of healthcare under constrained reimbursement (read: lower payments from payors). In the other world, illustrated here by the graphic artist Sean Kane for the American Academy of Family Practice, people — patients, healthy consumers, newly insured folks,
Self-care is the new black in health care
Consumers’ growing health care cost burden is competing with other household spending: basic costs for Americans are eroding what’s left of the traditionally-defined Middle Class. At the front end of health costs is the health insurance premium, the largest single line item for a family. It looks like a big number because it is: Milliman gauged the cost for an employer to cover a family of four in a PPO in the U.S. at around $23K, with the employee bearing an increasing percent of the premium, copays, coinsurance, and a larger deductible this year than last, on average. There are
Health insurance companies rank low on consumer experience
The corporate reputation, brand equity, of the health insurance continues to be low relative to other financial service industry benchmarks, found in the ACSI Finance and Insurance Report 2014. Customer satisfaction with health insurance companies fell between 2013 and 2014, especially attributed to higher costs hitting consumers in group (employer-based) policies. The 2014 American Customer Satisfaction Index (ACSI) is informed by interviews with 6,819 consumers interviewed via phone and email between July and September 2014. Customers of financial services companies (banks, credit unions, health insurance, life insurance, property & casualty, and internet brokerages) were asked to provide their opinions about named-firms
Health care costs, access and Ebola – what’s on health care consumers’ minds
The top 3 urgent health problems facing the U.S. are closely tied for first place: affordable health care/health costs, access to health care, and the Ebola virus. While the first two issues ranked #1 and #2 one year ago, Ebola didn’t even register on the list of healthcare stresses in November 2013. Gallup polled U.S. adults on the biggest health issues facing Americans in early November 2014, and 1 in 6 people named Ebola as the nation’s top health problem, ahead of obesity, cancer, as well as health costs and insurance coverage. Gallup points out that at the time of
Rationing health care, driven by high deductibles
Concerns about Death Panels and government restricting health services for people that have been key arguments used against the Affordable Care Act’s (ACA) detractors and, even before the advent of the ACA, proposed health reforms under President Clinton. But it’s peoples’ self-rationing in the U.S. health system that’s causing true rationing — driven by high deductible health plans (HDHPs) that are fast-growing in the health insurance market, and by the high cost of specialty drugs and prescriptions. There are plenty of data demonstrating the consumer health rationing trend being collected and reviewed by think tanks like RAND here, and by The
Health and financial well-being are strongly linked, CIGNA asks and answers
The modern view on wellness is “having it all” in terms of driving physical, emotional, mental and financial health across one’s life, according to CIGNA’s survey report, Health & Financial Well-Being: How Strong Is the Link? The key elements of whole health, as people define them are: – Absence of sickness, 37% – Feeling of happiness, 32% – Stable mental health, 32% – Management of chronic disease, 15% – Financial health, 14% – Living my dreams, 9%. 1 in 2 people (49%) agree that health and wellness comprise “all of these” elements, listed above. This holistic view of health is
Employers engaging in health engagement
Expecting health care cost increases of 5% in 2015, employers in the U.S. will focus on several tactics to control costs: greater offerings of consumer-directed health plans, increasing employee cost-sharing, narrowing provider networks, and serving up wellness and disease management programs. The National Business Group on Health’s Large Employers’ 2015 Health Plan Design Survey finds employers committed to health engagement in 2015 as a key strategy for health benefits. More granularly, addressing weight management, smoking cessation, physical activity, and stress reduction, will be top priorities, shown in the first chart. An underpinning of engagement is health care consumerism — which
Novel concept: people + health pricing information = market competition
In the post-Recession American economy, people shop for value in all things. And that includes health care services like MRIs — when patients are informed of pricing differences among imaging facilities and given free rein to pick-and-choose among them. In addition to lowering imaging costs in a community, price transparency also generated competition between providers. Health Affairs published this research detailed in Price Transparency for MRIs Increased Use of Less Costly Providers And Triggered Provider Competition in August 2014. An Economics 101 course teaches us that a well-oiled (perfect) market depends on lots of sellers of a product and lots of
We are all self-insured until we get sick – especially if we are women
During my conversation with a prominent pharma industry analyst yesterday, he observed, “As a consumer, you are self-insured until you get sick.” My brain then flashed back to a graph from the 2013 Employer Health Benefits Survey conducted annually by the Kaiser Family Foundation (KFF). The chart is shown here. It illustrates the upward line indicating that in 2013, 4 in 5 workers were enrolled in a health plan that included an annual deductible. That’s the “self-insurance” part of the observation my astute conversationalist noted. Simply put, when you are enrolled in a high-deductible health plan, You, The Consumer, are responsible for
The Season of Healthcare Transparency – Consumer Payments and Tools, Part 4
“The surge in HDHP enrollment is causing patients to become consumers of healthcare,” begins a report documenting the rise of patients making more payments to health providers. Patients’ payments to providers have increased 72% since 2011. And, 78% of providers mail paper statements to patients to collect what they’re owed. “HDHPs” are high-deductible health plans, the growing thing in health insurance for consumers now faced with paying for health care first out-of-pocket before their health plan coverage kicks in. And those health consumers’ expectations for convenience in payment methods is causing dissatisfaction, negatively affecting these individuals and their health providers’
The Season of Healthcare Transparency – Will Your Health Plan Be Your Transparency Partner? – Part 3
Three U.S. health plans cover about 100 million people. Today, those three market-dominant health plans — Aetna, Humana and UnitedHealthcare — announced that they will post health care prices on a website in early 2015. Could this be the tipping point for health care transparency so long overdue? These 3 plans are ranked #1, #4 and #5 in terms of market shares in U.S. health insurance. Together, they will share price data with the Health Care Cost Institute (HCCI), a not-for-profit organization dedicated to research on U.S. health spending. An important part of the backstory is that the HCCI was
The Season of Healthcare Transparency – Shopping in a World of High Cost and High Variability – Part 2
Yesterday kicked off this week in Health Populi, focusing on the growing role of transparency in health care in America. Today’s post discusses the results from Change Healthcare’s latest Healthcare Transparency Index report, based on data from the fourth quarter of 2013, published in May 2014. Charges for health services — dental, medical and pharmacy – varied by more than 300% in Q42013 — even within a single health network. Change Healthcare found this, based on their national data on 7 million health-covered lives. The company analyzed over 180 million medical claims. The company built the Healthcare Transparency Index (HCTI)
Wearable tech + the workplace: driving employee health
Employer wellness programs are growing in the U.S., bundled with consumer-directed plans and health savings accounts. A wellness company’s work with employee groups is demonstrating that workers who adopt mobile health technologies — especially “wearables” coupled with smartphone apps — helps change behavior and drive health outcomes. Results of one such program are summarized in Wearables at Work, a technical brief from Vitality, a joint venture of Humana and Discovery Ltd., published April 23, 2014. Vitality has been working in workplace wellness since 2005, first using pedometers to track workers’ workouts. In 2008, Vitality adopted the Polar heart rate monitor for
Consumers’ spending on medicine grows – the retailization of health care
People are spending more out of their own pockets on health care, and particularly for medications. There are two sides to the medicine-spending coin: there’s the low-end which are generic drugs, most of which carry a co-pay of $10 or less. Then there’s the high end of specialty pharmaceuticals, a fast-growing category of very expensive products for which many consumers dearly pay — if and when they choose to take their doctors’ recommendations. In Medicine use and shifting costs of healthcare, IMS Institute for Healthcare Informatics reports that while (inexpensive) generic drugs comprise 86% of prescriptions in the U.S., it’s high
The four futures of health care: simple, guru, ecosystem, self-care
In the not-too-distant future, will our health care be universally available to all, standardized with limited choices? Or, will we be in self-care mode, able to “buy up” if we can afford it like luxury goods? Will health care delivery be totally tech- and information-driven? Or, will care be driven by insurers’ health plans with artful designs that (almost) predetermine our choices? Welcome to four futures of health care, brought to us by PA Consulting whose report, How Can We Stop Healthcare From Bankrupting Our Children? speaks to scenarios based on 2 uncertainties, whether: Health care will be a personal
Risk-shift: employers continue to push more risk to employees and families for health costs
With health costs increase increasing at 4.4% in 2014, a slightly higher rate of growth than the 4.1% seen in 2013. While this is lower than the double-digit increases U.S. employers faced in 2001-2004, it’s still twice the rate of general consumer price inflation. That’s what the first graph shows, based on the The 19th Annual Towers Watson/National Business Group on Health Employer Survey on Purchasing Value in Health Care. Employers generally want to continue to provide health insurance…for the time being. 92% of companies expect to make changes in health plan provisions in 2014, with 1 in 2 anticipating “significant
The new retail health: Bertolini of Aetna connects dots between the economy and health consumers
3 in 4 people in America will buy health care at retail with a subsidy within just a few years, according to Mark Bertolini, CEO of Aetna. Bertolini was the first keynote speaker this week at the 2014 HIMSS conference convened in Orlando. Bertolini’s message was grounded in health economics 101 (about which frequent readers of Health Populi are accustomed to hearing). A healthy community drives a healthy local economy, and healthier people are more economically satisfied, Bertolini explained. The message: health care can move from being a cost driver to being an economic engine. But getting to a healthy
Patients play a starring role at #HIMSS14 – Best In Show
Even before stepping into the Orlando Convention Center on Sunday 23 February 2014, my clairvoyant powers know the forecast of the Best in Show: the growing role of patients in health care, reflected in both the education session at the annual 2014 meeting of HIMSS as well as the product/service mix being proffered on the convention show floor. As a member of HIMSS Connected Patient Committee, I know first-hand the conscious effort and energy that the organization has committed to getting real about patients’-peoples’-caregivers’ central role in health care. The organization was built on providers and technology. When I first
Where’s TripAdvisor for health care? JAMA on physician ratings sites
As more U.S. health citizens enroll in high-deductible health plans – now representing about 30% of health-insured people in America – health plan members are being called on to play the role of consumer. Among the most important choices the health consumer makes is for a physician. Ratings sites and health care report cards ranking doctors by various characteristics have been in the market for over a decade. However, little has been known on the public’s knowledge about the availability of these information sources, nor of peoples’ use of physician rating sites. This question is addressed in Public Awareness, Perception, and
A CT for $300 or $2,781 – why health price transparency matters
Charges for medical, pharmacy and dental services can vary by more than 300%. This means that in one place, a procedure that costs $100 can cost $300 for the same treatment in another location or practice, discovered by Change Healthcare in their latest Healthcare Transparency Index 2013 Q3 Report, published in January 2014. The 300% is the average overall across dozens of health services used by the 67,000 plan members Change Healthcare analyzed based on health plan enrollees’ health care utilization in the third quarter of 2013. These health care services include office visits (behavioral health, physical therapy and
What, We Worry? Thinking About Healthcare (Costs) Is Stressing Us Out
Three-quarters of us are concerned about health care, a fraction fewer than those of us worried about the economy. Underneath stress about healthcare, people are worried about costs and the impact of the Affordable Care Act (ACA). Say hello to the Healthcare Worry Scale, developed by Chase Communications, a firm focused on marketing and media, largely in the health industry. Chase found that: – 93% believe that their health care costs will continue to increase – 49% say the ACA’s impact is a “major” worry – 43% say getting a disease, medical condition, or injury that health insurance doesn’t fully
Health Care Everywhere at the 2014 Consumer Electronics Show
When the head of the Consumer Electronics Association gives a shout-out to the growth of health products in his annual mega-show, attention must be paid. The #2014CES featured over 300 companies devoted to “digital health” as the CEA defines the term. But if you believe that health is where we live, work, play, and pray, then you can see health is almost everywhere at the CES, from connected home tech and smart refrigerators to autos that sense ‘sick’ air and headphones that amplify phone messages for people with hearing aids, along with pet activity tracking devices like the Petbit. If
mHealth will join the health ecosystem – prelude to the 2014 Consumer Electronics Show
The rise of digital health at the 2014 Consumer Electronics Show signals the hockey-stick growth of consumer-facing health devices for fitness and, increasingly, more medical applications in the hands of people, patients, and caregivers. This year at #CES2014, while the 40% growth of the CES digital health footprint will get the headlines, the underlying story will go beyond wristbands and step-tracking generating data from an N of 1 to tools that generate data to bolster shared-decision making between people and the health system, and eventually support population health. For example: – Aetna is partnering with J&J to deploy their Care4Today
A certain forecast: health consumers will be more cost-squeezed in 2014 for Rx and insurance
Gird your wallets, U.S. consumers: watch the dollars flow out-of-pocket for prescription drugs in 2014, as predicted by the 2013-2014 Prescription Drug Benefit Cost and Plan Design Report published by the Pharmacy Benefit Management Institute (PBMI) this week. Constraints covering most plan members are: Step therapy Prior authorization (to get approvals to fill high-cost drugs, notably growth hormones, injectables, controlled substances, Retin-A, and medications for sleep disorders, and Compulsory 90 day refills at retail (90-day dispensing for chronic meds). This Report, sponsored by Takeda, is the gold standard of drug benefit trends, having been published since 1995. Average 30-day copayments
Employers will strongly focus on costs in health benefit plans for 2014; so must consumers
Employers who sponsor health insurance in America are at a fork on a cloudy road: they know that they’re in the midst of changes happening in the U.S. health system. Except for one certainty: that health care costs too much. So employers’ plans for health benefits in 2014 strongly focus on getting a return-on-investment from health spending in an uncertain climate, according to Deloitte’s 2013 Survey of U.S. Employers. Key findings are that: Employers will grow their use of workers’ cost-sharing, continuing to shift more financial responsibility onto employees They will expand other tactics they believe will help address cost
Bundles in health care are the prix fixe menu
Ordering up and financing health care in the U.S. looks like the proverbial Chinese food menu, picking and paying for “one from column A, and one from column C.” But that’s no way to operate a well-oiled machine for delivering quality health care, according to Healthcare Shifts from á la Carte to Prix Fixe from Strategy&, an analysis of the fragmented, high-cost and only fair quality American health system. One solution to this challenge is bundled payment. “No one has an overarching view of the entire process,” the report opines, “with an eye toward improving customer service, quality, or costs.” Further exacerbating the sub-optimal
Health care and costs on front-burner for people in America (again)
This week in America, the concept of “health care consumer” is in a tug-of-war, and those of us trying to behave as such feel bloodied in the skirmish. One side of the tug-of-war is the obvious, post October 1st reality of the sad state of the Health Insurance Exchanges. This has been well covered in mass media, right, left and center. And Americans polled by Gallup last week express their knowledge of that fact — even if they didn’t know what Healthcare.gov was on the 1st of October. The first chart shows that health care is now a front-burner issue
America’s health care is better due to Todd Park – detractors, be careful what you wish for
In the aftermath of the snafu that was/is the failed launch of the Affordable Care Act’s Health Insurance Exchange comes, today via Reuters, an article called Obama’s tech expert becomes target over healthcare website woes. The piece, by Roberta Rampton and Sarah McBride, states that Todd Park, Chief Technology Officer at The White House, “now finds himself among a handful of officials with targets on their backs as Republicans try to root out who is responsible for this month’s glitch-ridden rollout of Healthcare.gov,” going on to say that “The White House trotted him out in July to talk up the new version”
Innovating and thriving in value-based health – collaboration required
In health care, when money is tight, labor inputs like nurses and doctors stretched, and patients wanting to be treated like beloved Amazon consumers, what do you do? Why, innovate and thrive. This audacious Holy Grail was the topic for a panel II moderated today at the Connected Health Symposium, sponsored by Partners Heathcare, the Boston health system that includes Harvard’s hospitals and other blue chip health providers around the region. My panelists were 3 health ecosystem players who were not your typical discussants at this sort of meeting: none wore bow ties, and all were very entrepreneurial: Jeremy Delinsky
Consumers trust and welcome health and insurance providers to go DTC with communications
Consumers embrace ongoing dialog with the companies they do business with, Varolii Corporation toplines in a survey report, What Do Customers Want? A Growing Appetite for Customer Communications. Across all vertical industries consumers trust for this dialogue, health care organizations – specifically doctors, pharmacists, and insurance companies – are the most trusted. Examples of “welcome-comms” would be reminders about upcoming appointments or vaccinations (among 69% of people), notices to reorder or pick up a prescription (57%), and messages encouraging scheduling an appointment (39%). In banking, notices about fraudulent activity on one’s account is the most welcomed message beating out appointment
The new era of consumer health risk management: employers “migrate” risk
The current role of health insurance at work is that it’s the “benefits” part of “compensation and benefits.” Soon, benefits will simply be integrated into “compensation and compensation.” That is, employers will be transferring risk to employees for health care. This will translate into growing defined contribution and cost-shifting to employees. Health care sponsorship by employers is changing quite quickly, according to the 2013 Aon Hewitt Health Care Survey published in October 2013. Aon found that companies are shifting to individualized consumer-focused approaches that emphasize wellness and “health ownership” by workers to bolster behavior change and, ultimately, outcomes. The most
Whither price transparency in health care? The supply side may be growing faster than consumer demand
Online shopping for health care can drive costs down, according to research conducted by HealthSparq, a company that works with health insurance companies to channel health cost information to plan members (that is, consumers). Healthsparq partnered with one of the company’s health insurance company clients to conduct this study, which demonstrated that, over two years, consumers who used an online treatment cost estimator saved money on care for hernia conditions, digestive conditions, and women’s health issues. It’s early days for health care price transparency in health care, but HealthSparq’s findings demonstrate positive evidence that when consumers are offered a tool
U.S. Health Citizens Needed a Dummies Guide to the ACA
The Affordable Care Act (ACA) was signed in March 2010; that month, 57% of U.S. adults did something to self-ration health care, such as splitting prescription pills, postponing necessary health care, and putting off recommended medical tests, according to the Kaiser Family Foundation (KFF) Health Tracking Poll of March 2010. 57% of U.S. adults are still self-rationing health care in September 2013, according to KFF’s latest Health Tracking Poll, completed among 1,503 U.S. adults just two weeks before the launch of the Health Insurance Marketplaces on October 1, 2013. As of September 2013, only 19% of U.S. adults said they had heard
The slow economy is driving slower health spending; but what will employers do?
By 2022, $1 in every $5 worth of spending in the U.S. will go to health care in some way, amounting to nearly $15,000 for each and every person in America. From biggest line item on down, health spending will go to payments to: Hospitals, representing about 32% of all spending Physicians and clinical costs, 20% of spending Prescription drugs, 9% of spending Nursing, continuing care, and home health care, together accounting for over 8% of health spending (added together for purposes of this analysis) Among other categories like personal care, durable medical equipment, and the cost of health insurance.
Food and the household health budget: one pocket, shrinking access
Over 1 in 5 people in the U.S. have not had enough money to buy food for themselves or their families in the past year, according to the August 2013 Gallup Healthways Index. This is as many consumers as those who couldn’t afford food during the deepest months of the last recession. Lack of access to food is a challenge for a cadre of Americans who lack access to other basic needs such as shelter and health care. Gallup’s Basic Access Index looks at this market basket, and has found that Americans’ access to basic needs at 81.4 in August
Consumers don’t get as much satisfaction with high-deductible health plans
Since the advent of the so-called consumer-directed health care era in the mid-2000s, there’s been a love-gap between health plan members of traditional plans, living in Health Plan World 1.0, and people enrolled in newer consumer-driven plans – high-deductible health plans (HDHPs) and consumer-directed health plans (CDHPs). That gap in plan satisfaction continues, according to the Employee Benefits Research Institute (EBRI)’s poll of Americans’ consumer engagement in health care. The survey was conducted with the Commonwealth Fund. As the bar chart illustrates, some 62% of members in traditional plans were satisfied (very or extremely) with their health insurance in 2012.
Criticizing health reform has jumped the shark for mainstream Americans
You might see potato and I might see po-tah-to when looking at the Affordable Care Act – health reform — but it’s clear we don’t want to call the whole thing off. (Go to 1:44 seconds in this video to get my drift, thanks to the Gershwin’s). I’m talking about the latest August 2013 Kaiser Health Tracking Poll from Kaiser Family Foundation finds a health citizenry suffering ennui or a form of split personality about health reform: while many Americans don’t believe the Affordable Care Act (ACA) will help them, most don’t want Congress to de-fund it, either. Several graphs from
HSAs for Dummies: improving health insurance literacy
Most Americans don’t understand what a health savings account (HSA) is – including people who are enrolled in the plans. While health literacy is generally acknowledged to be a public health challenge in America, health insurance literacy is not well recognized. Yet in the emerging consumer-directed health plan era of U.S. health care, peoples’ lack of understanding of health financial accounts will get in the way of people who really need care seeking care at the right time. This leads to greater health spending later when the consumer-patient can develop a health condition that could have been prevented (say, pre-diabetes
Chief Health Officers, Women, Are In Pain
Women are the Chief Health Officers of their families and in their communities. But stress is on the rise for women. Taking an inventory on several health risks for American women in 2013 paints a picture of pain: of overdosing, caregiver burnout, health disparities, financial stress, and over-drinking. Overdosing on opioids. Opioids are strong drugs prescribed for pain management such as hydrocodone, morphine, and oxycodone. The number of opioid prescriptions grew in the U.S. by over 300% between 1999 and 2010. Deaths from prescription painkiller overdoses among women have increased more than 400% since 1999, compared to 265% among men.
Working for health care in 2013: workers’ health insurance cost burden still grows faster than wages
Insurance premium costs grew 4% for families between 2012 and 2013, with workers now bearing 39% of health premiums in 2013 compared with only 26% ten years ago, in 2003. That’s a 50% increase in health plan premium “burden” for working families, by my calculation. This snapshot of health insurance in 2013 comes to us from the 2013 Employer Health Benefits Survey, provided by the Kaiser Family Foundation (KFF) and the Health Research & Educational Trust (HRET). This research is one of the most important annual reports to hit the health care industry every year, and this year’s analysis provides strategic context
Americans’ health insurance illiteracy epidemic – simpler is better
Consumers misunderstand health insurance, according to new research published in the Journal of Health Economics this week. The study was done by a multidisciplinary, diverse team of researchers led by one of my favorite health economists, George Loewenstein from Carnegie Mellon, complemented by colleagues from Humana, University of Pennsylvania, Stanford, and Yale, among other research institutions. Most people do not understand how traditional health plans work: the kind that have been available on the market for over a decade. See the chart, which summarizes top-line findings: nearly all consumers believe they understand what maximum out-of-pocket costs are, but only one-half do.
The health care automat – Help Yourself to healthcare via online marketplaces
Imagine walking into a storefront where you can shop for an arthroscopy procedure, mammogram, or appointment with a primary care doctor based on price, availability, quality, and other consumers’ opinions? Welcome to the “health care automat,” the online healthcare marketplace. This is a separate concept from the new Health Insurance Marketplace, or Exchange. This emerging way to shop for and access health care services is explored in my latest paper for the California HealthCare Foundation (CHCF), Help Yourself: The Rise of Online Healthcare Marketplaces. What’s driving this new wrinkle in retail health care are: U.S. health citizens morphing into consumers,
10 Reasons Why ObamaCare is Good for US
When Secretary Sebelius calls, I listen. It’s a sort of “Help Wanted” ad from the Secretary of Health and Human Services Kathleen Sebelius that prompted me to write this post. The Secretary called for female bloggers to talk about the benefits of The Affordable Care Act last week when she spoke in Chicago at the BlogHer conference. Secretary Sebelius’s request was discussed in this story from the Associated Press published July 25, 2013. “I bet you more people could tell you the name of the new prince of England than could tell you that the health market opens October 1st,” the
In the US health care cost game, doctors have seen the enemy – and it’s not them
When it comes to who’s most responsible for reducing the cost of health care in America, most doctors put the onus on trial lawyers, health insurance companies, pharma and medical device manufacturers, hospitals, and even patients. But physicians themselves ? Not so much responsibility – only 36% of doctors polled said doctors should assume major responsibility in reducing health care costs. And, in particular, most U.S. physicians have no enthusiasm for reducing health care costs by changing payment models, like penalizing providers for hospital re-admissions or paying a group of doctors a fixed, bundled price for managing population health. Limiting
Urgent care centers: if we build them, will all patients come?
Urgent care centers are growing across the United States in response to emergency rooms that are standing-room-only for many patients trying to access them. But can urgent care centers play a cost-effective, high quality part in stemming health care costs and inappropriate use of ERs for primary care. That’s a question asked and answered by The Surge in Urgent Care Centers: Emergency Department Alternative or Costly Convenience? from the Center for Studying Health System Change by Tracy Yee et. al. The Research Brief defines urgent care centers (UCCs) as sites that provide care on a walk-in basis, typically during regular
What to expect from health care between now and 2018
Employers who provide health insurance are getting much more aggressive in 2013 and beyond in terms of increasing employees’ responsibilities for staying well and taking our meds, shopping for services based on cost and value, and paying doctors based on their success with patients’ health outcomes and quality of care. Furthermore, nearly one-half expect that technologies like telemedicine, mobile health apps, and health kiosks in the back of grocery stores and pharmacies are expected to change the way people regularly receive health care. What’s behind this? Increasing health care costs, to be sure, explains the 18th annual survey from the National
They call it “primary” care because it comes first — and it should
It’s called “primary” care for a reason: it’s first and foremost important in the health care services a person can use. In its report, Primary care: our first line of defense, The Commonwealth Fund explains why primary care is crucial to one’s individual health, and how primary care is morphing into medical teams and patient-centered medical homes. And that’s a good thing for you and me, the Fund says. That’s because people in the U.S. who have a primary care doctor have 33% lower health costs and 19% lower risk of dying than people who see only a specialist (Source:
Health consumers, meet the medical bank
Health consumers, meet a new player in your health care world: the bank. Financial services companies will play a growing role in U.S. health care as patients morph into health care consumers responsible for making more money-based decisions about their health care. This shift could make paying for health care just like paying other bills in the consumer retail market. And that’s a new role for health providers – doctors and hospitals – to fill. The Impact of Growing Patient Financial Responsibility on Healthcare Providers, prepared for Citi Enterprise Payments by Boundary Information Group, discusses what the impact of consumers’ payments in
As Account-Based Health Plans Grow, Will Americans Save More in Health Accounts?
The only type of health plan whose membership grew in 2012 was the consumer-directed health plan (CDHP), according to a survey from Mercer, the benefits advisors. Two-thirds of large employers expect to offer CDHPs by 2018, five years from now. 40% of all employers (small and large) anticipate offering a CDHP in five years. The growth in CDHPs going forward will be increasingly motivated by the impending “Cadillac tax” that will be levied on companies that currently offer relatively rich health benefits. Furthermore, Mercer foresees that employers will also expand wellness and health management programs with the goal of reducing health
The emerging economy for consumer health and wellness
The notion of consumers’ greater skin in the game of U.S. health care — and the underlying theory of rational economic men and women that would drive people to greater self-care — permeated the agenda of the 2nd annual Consumer Health & Wellness Innovation Summit, chaired by Lisa Suennen of Psilos Ventures. Lisa kicked off the meeting providing a wellness market landscape, describing the opportunity that is the ‘real’ consumer-driven health care: people getting and staying well, and increasing participation in self-management of chronic conditions. The U.S. health system is transforming, she explained, with payors beginning to look like computer
Consumer-directed health isn’t always so healthy
Giving health consumers more skin in the game doesn’t always lead to them making sound health decisions. Over four years in consumer-directed health plans, enrollees used one-quarter fewer visits to doctors every year and filled one fewer prescription drugs. CDHP members also received fewer recommended cancer screenings, and visited the emergency room more often. These rational health consumer theory-busting findings were published in the June 2013 issue of the Health Affairs article, Consumer-Directed Health Plans Reduce The Long-Term Use of Outpatient Physician Visits And Prescription Drugs by Paul Fronstin of the Employee Benefit Research Institute and colleagues from IBM and RxEconomics,
Health care costs for a family of 4 in 2013: a college education, a diamond or a 4-door sedan
If you have $22,030 in your wallet, you can buy: A princess-cut diamond A Ford Focus 4-door A year’s tuition at James Madison University (in-state, 2013-14) A health plan for a family of four. The 2013 Milliman Medical Index gauges the annual health care costs for a typical American family at $22,030, up $1,302 from 2012 — a 6.3% increase, nearly 6x the all-items increase of 1.1% for the U.S. Consumer Price Index from April 2012-April 2013. That 1.1% includes the costs of food and energy, along with cars, tobacco, shelter, and other consumer goods. In 2013, the average family will
Most employers will provide health insurance benefits in 2014…with more costs for employees
Nearly 100% of employers are likely to continue to provide health insurance benefits to workers in 2014, moving beyond a “wait and see” approach to the Affordable Care Act (ACA). As firms strategize tactics for a post-ACA world, nearly 40% will increase emphasis on high-deductible health plans with a health savings account, 43% will increase participants’ share of premium costs, and 33% will increase in-network deductibles for plan members. Two-thirds of U.S. companies have analyzed the ACA’s cost impact on their businesses but need to know more, according to the 2013 survey from the International Foundation of Employee Benefit Plans (IFEBP).
The health/wealth disconnect in America
Two in 3 Americans are uncomfortable with their financial situation. And most are totally oblivious to how much money they will need to spend on health care in the future. Seven in 10 people expect to spend less than 10% of their monthly retirement income on medical and dental expenses; but the real number is 30% of income needed for health care in retirement, according to The Urban Institute. The Wellness for Life survey, conducted for Aviva, the life and disability company, collaborating with the Mayo Clinic, finds an American health citizen out of touch with their personal health economics.
Americans feeling more financially insecure
One in three workers does not feel financially secure. The proportion of Americans who feel “not at all secure” grew to 16% from 12% between 2011 and 2012, based on the question, “When it comes to paying your bills and keeping up with living expenses, how financially secure do you feel these days?” Women are much more likely than men to feel financially insecure, representing a 33% growth rate in financial insecurity. These sobering financial statistics come to us from the UNUM study, 2012 Employee Education and Enrollment Survey: Employee Perspectives on Financial Security, published May 8, 2013. Based on the question asked – paying
Un-directed Americans in a consumer-directed healthcare world
U.S. employers have been implementing various flavors of consumer-directed health plans for the better part of a decade. But consumers feel neither “directed” nor especially competent in managing their way through these plans. It appears that employers also have their own sort of health plan illiteracy when it comes to understanding health reform — the Affordable Care Act — according to the 2013 Aflac WorkForces Report (AWR) based on a survey of 1,900 benefits managers and over 5,200 U.S. workers conducted in January 2013. While you might know the Aflac Duck, you may not be aware that Aflac is the
Bending the cost-curve: a proposal from some Old School bipartisans
Strange political bedfellows have come together to draft a formula for dealing with spiraling health care costs in the U.S. iin A Bipartisan Rx for Patient-Centered Care and System-Wide Cost Containment from the Bipartisan Policy Center (BPC). The BPC was founded by Senate Majority Leaders Howard Baker, Tom Daschle, Bob Dole, and George Mitchell. This report also involved Bill Frist, Pete Domenici, and former White House and Congressional Budget Office Director Dr. Alice Rivlin who together work with the Health Care Cost Containment Initiative at the BPC. The essence of the 132-page report is that the U.S. health system is
Food = Health for employers, hospitals, health plans and consumers
Food is inextricably bound up with health whether we are well or not. Several key area of the Food=Health ecosystem made the news this week which, together, will impact public and personal health. On the employer health benefits front, more media are covering the story on CVS strongly incentivizing employees to drop body mass index (BMI) through behavioral economics-inspired health plan design of a $50 peer month penalty. Michelin, whose bulky advertising icon Bibendum has more than one “spare tire,” introduced a program to combat health issues, including but not limited to BMI and high blood pressure, according to the
US Health Executives Predict the ACA Will Increase Health Insurance Premiums
As a result of implementing the Affordable Care Act (health reform), most U.S. health executives crystal balls foresee health care insurance premiums will increase over 10% in the next three years. 4 in 10 predict premiums will grow over 25% over the next 3 years. This sobering forecast comes out of a Munich RE Health survey conducted among 326 health industry executives in March 2013. Those polled included representatives from health plans, managed care, disease management firms, and health insurance brokers and agents. How do health execs expect employers would deal with such fast-rising health premium costs? Why shift more
The need for a Zagat and TripAdvisor in health care
Patient satisfaction survey scores have begun to directly impact Medicare payment for health providers. Health plan members are morphing into health consumers spending “real money” in high-deductible health plans. Newly-diagnosed patients with chronic conditions look online for information to sort out whether a generic drug is equivalent to a branded Rx that costs five-times the out-of-pocket cost of the cheaper substitute. While health care report cards have been around for many years, consumers’ need to get their arms around relevant and accessible information on quality and value is driving a new market for a Yelp, Travelocity, or Zagat in
The value of big data in health care = $450 billion
Exploiting Big Data in industry is Big News these days, and nowhere is the potential for leveraging the concept greater than in health care. McKinsey & Company estimates that harnessing big data across five dimensions of health care could yield nearly one-half trillion dollars’ worth of value in The ‘big data’ revolution in healthcare. The chart summarizes McKinsey’s calculations on the value of Big Data in health care at its maximum. Before digging into the value potential, just what is Big Data in health care? Statistics and information are generated in the health care system about patients: say, during visits
U.S. Health Costs vs. The World: Is It Still The Prices, and Are We Still Stupid?
Comparing health care prices in the U.S. with those in other developed countries is an exercise in sticker shock. The cost of a hospital day in the U.S. was, on average, $4,287 in 2012. It was $853 in France, a nation often lauded for its excellent health system and patient outcomes but with a health system that’s financially strapped. A routine office visit to a doctor cost an average of $95 in the U.S. in 2012. The same visit was priced at $30 in Canada and $30 in France, as well. A hip replacement cost $40,364 on average in the
The Not-So-Affordable Care Act? Cost-squeezed Americans still confused and need to know more
While health care cost growth has slowed nationally, most Americans feel they’re going up faster than usual. 1 in 3 people believe their own health costs have gone up faster than usual, and 1 in 4 feel they’re going out about “the same amount” as usual. For only one-third, health costs feel like they’re staying even. As the second quarter of 2013 begins and the implementation of the Affordable Care Act (ACA, aka “health reform” and “Obamacare”) looms nearer, most Americans still don’t understand how the ACA will impact them. Most Americans (57%) believe the law will create a government-run health plan,
The Rationale for CVS “Sticking” (vs. “Carroting”) It To Employees for Wellness
The Boston Herald was one of the first newspapers talking about CVS requiring workers to disclose personal health information…”or pay a $600 a year fine,” as the LA Times succinctly put the situation. The story is that CVS Caremark, the pharmacy and Rx benefits management company, is implementing a health screening program to measure height, weight, body fat, and blood pressure. These metrics are commonly collected in the process known as health risk appraisals (HRAs), which most large employers have begun to implement to help employees prevent the onset of chronic disease (think: “metabolic syndrome,” diabetes combined with overweight, for
Most consumers will look to health insurance exchanges to buy individual plans in 2013
As the Affordable Care Act, health reform, aka Obamacare, rolls out in 2013, American health insurance shoppers will look for sources of information they can trust on health plan quality and customer service satisfaction — as they do for automobiles, mobile phone plans, and washing machines. For many years, one of a handful of trusted sources for such insights has been J.D. Power and Associates. J.D. Power released its 2013 Member Health Plan Study (the seventh annual survey) and found that most consumers currently enrolled in a health plan have had a choice of only “one” at the time





 Thank you, Jared Johnson, for including me on the list of the
Thank you, Jared Johnson, for including me on the list of the  I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a