More Evidence of Self-Rationing as Patients Morph into Healthcare Payors

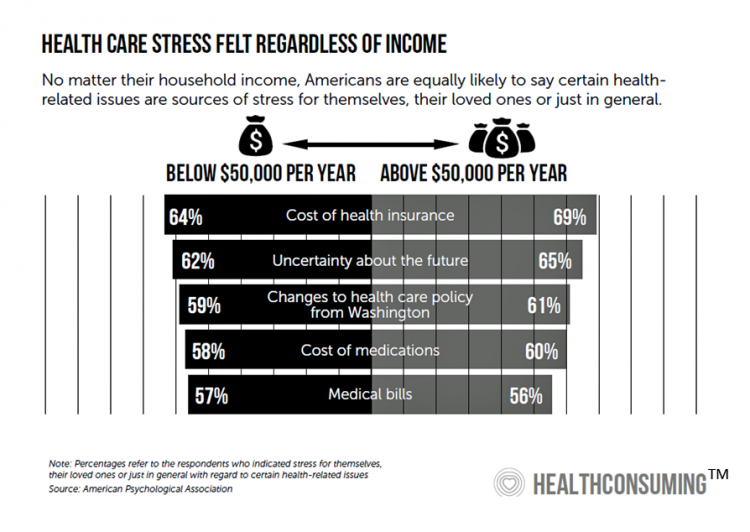
Several new studies reveal that more patients are feeling and living out their role as health care payors as medical spending vies with other household line items. This role of patient-as-the-payor crosses consumers’ ages and demographics, and is heating up health care as the top political issue for the 2020 elections at both Federal and State levels. In research from HealthPocket, 2 in 5 Americans said they needed to reduce other household expenses to be able to afford their monthly insurance premiums. Four in ten consumers said their monthly health insurance premiums were increasing. One in four people in the
A Tale of Two Americas as Told by the 2019 OECD Report on Health

It was the best of times, It was the worst of times, It was the age of wisdom, it was the age of foolishness, It was the epoch of belief, it was the epoch of incredulity, … starts Dickens’ Tale of Two Cities. That’s what came to my mind when reading the latest global health report from the OECD, Health at a Glance 2019, which compares the United States to other nations’ health care outcomes, risk factors, access metrics, and spending. Some trends are consistent across the wealthiest countries of the world, many sobering, such as: Life expectancy rates fell in 19 of the
Great Expectations for Health Care: Patients Look for Consumer Experience and Trust in Salesforce’s Latest Research

On the demand side of U.S. health care economics, patients are now payors as health consumers with more financial skin in paying medical bills. As consumers, people have great expectations from the organizations on the supply side of health care — providers (hospitals and doctors), health insurance plans, pharma and medical device companies. But as payors, health consumers face challenges in getting care, so great expectations are met with frustration and eroding trust with the system, according to the latest Connected Healthcare Consumer report from Salesforce published today as the company announced expansion of their health cloud capabilities. This is
Will Consumers Cross the Cost-and-Trust Chasm Between Prescription Drugs and Hospitals?
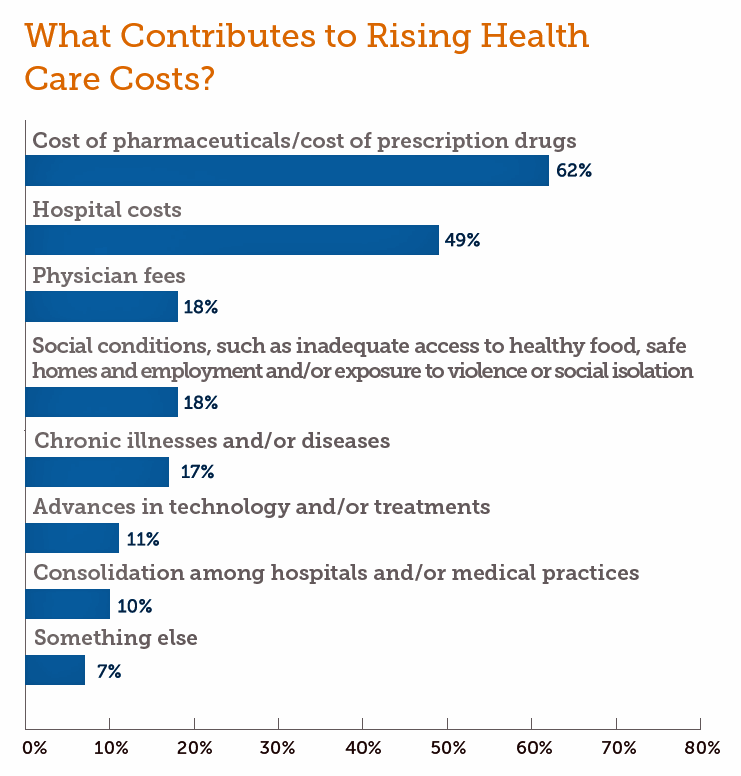
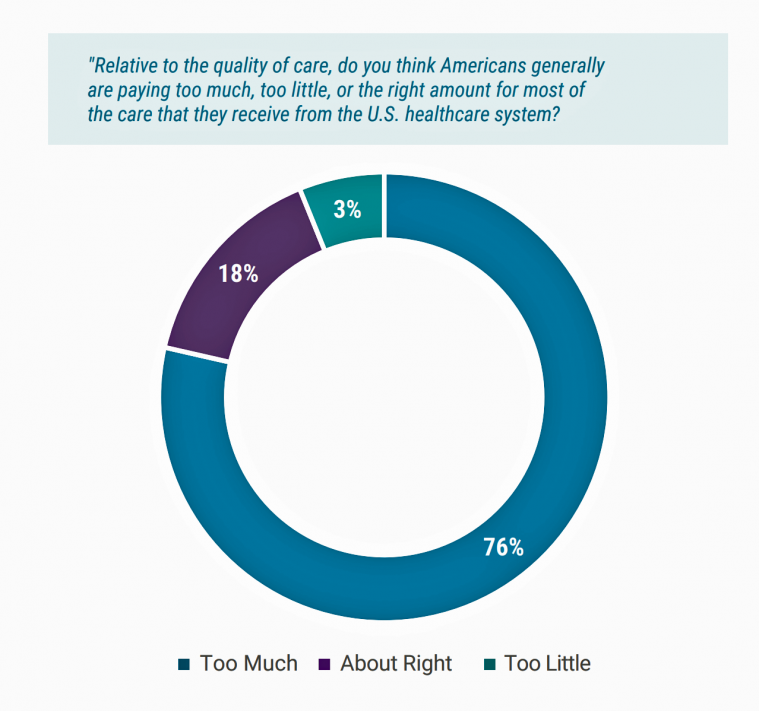
People in the U.S. rank prescription drugs, lab tests, emergency room visits, dental and vision care, preventive services, chronic disease management and mental health care as the “most essential” health care services, according to the 2019 Survey of America’s Patients conducted by The Physicians Foundation. When asked what factors contribute to rising health care costs in America, most consumers cite the cost of prescription drugs. Taken together, these two data points demonstrate the potent political import of prescription drug prices as the U.S. approaches the 2020 Presidential election. The Physicians Foundation surveyed 2,001 U.S. adults between 27 and 75 years
Learning from Dr. Eric Topol, Live from Medecision Liberation 2019

“Bold thinking is great. Bold doing is better,” Dr. Eric Topol introduced his talk yesterday at Medecision’s Liberation 2019 conference. I have the opportunity, for which I’m so grateful, of not only attending this meeting but playing a role as a speaker, a sometimes stage “emcee,” and a keynote speaker. And as an attendee, I learn so much from other speakers, fellow attendees, and Medecision staff all sharing perspectives during breakouts and networking breaks. In mode of attendee (and self-confessed collegial-groupie of Dr. Topol’s), I took in his remarks taking notes as fast as I could thanks to Mom teaching
Wasted: $1 of Every $4 Spent on Health Care In America
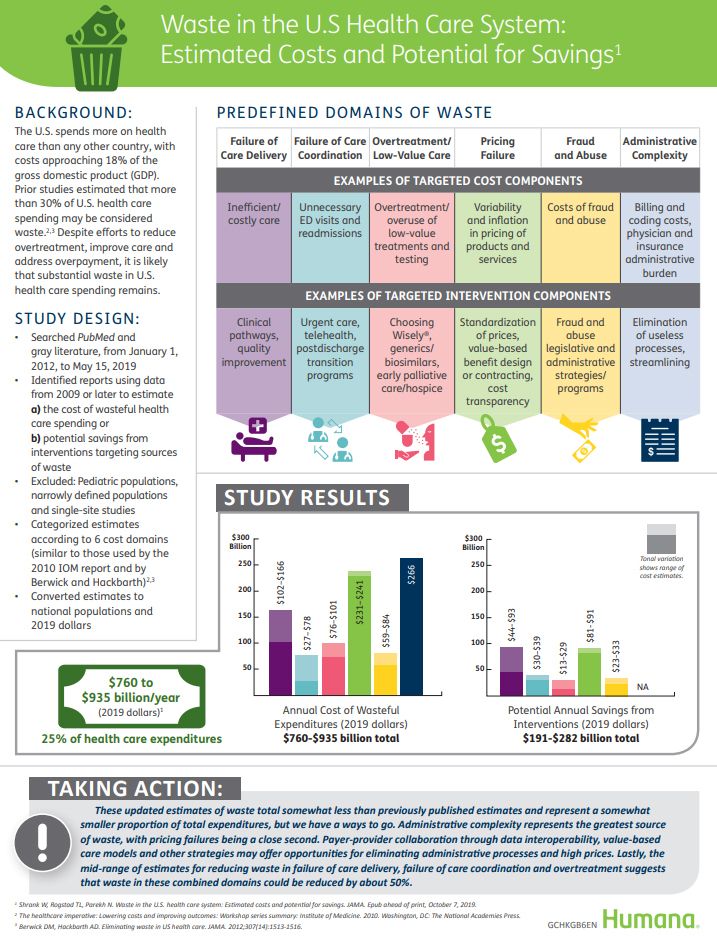
A study in JAMA published this week analyzed research reports that have measured waste in the U.S. health care system, calculating that 25% of medical spending in America is wasted. If spending is gauged at $3.8 trillion, waste amounts to nearly $1 trillion. If spending is 18% of the American gross domestic product (GDP), then some 4.5% of the U.S. economy is wasted spending by the health care system and its stakeholders. In “Waste in the US Health Care System,” a team from Humana and the Univrsity of Pittsburgh recalibrated the previous finding of 30% of wasted spending to the 25%,
The Hospital CFO in the Anxiety Economy – My Talk at Cerner’s Now/Next Conference
As patients have taken on more financial responsibility for first-dollar costs in high-deductible health plans and medical bills, hospitals and health care providers face growing fiscal pressures for late payments and bad debt. Those financial pressures are on both sides of the health care payment transaction, stressing patients-as-payors and health care financial managers alike. I’m speaking to health industry stakeholders on patients-as-payors at Cerner’s Now/Next conference today about the patient-as-payor, a person primed for engagement. That’s as in “Amazon-Primed,” which patients in their consumer lives now use as their retail experience benchmark. But consumers-as-patients don’t feel like health care today
Prelude to Health 2.0 2019: Thinking Consumers At the Center of Digital Health Transformation

“Digital transformation” is the corporate strategy flavor of the moment across industries, and the health are sector isn’t immune from the trend. As this 13th year of the annual Health 2.0 Conference kicks off this week, I’m focused on finding digital health innovations that engage people — consumers, caregivers, patients, health citizens all. This year’s conference will convene thought leaders across a range of themes, and as is the Health 2.0 modus operandi, live demo’s of new-new things. As Health 2.0 kicks off today in pre-conference sessions, there is useful context described in a new report from the American Hospital
Health Care Providers Grow Consumer-Facing Muscles Driven by Retail & Tech-Health Competition
As patients continue to morph into health care payers, they’re increasingly expecting value-for-money, transparency, and customer experiences that show respect, bolster trust, and deliver quality services. Is that so much to ask from health care providers? Sure is, as it turns out, based on this year’s annual report from Kaufman Hall, the 2019 State of Consumerism in Healthcare: The Bar is Rising. For several years, Kaufman Hall have developed an Index of healthcare consumerism based on several pillars that, together, gauge health care providers’ performance on consumer health engagement. Providers fall into one of four tiers, ranging from Tier 1
Milliman Finds PPO for Family of 4 in 2019 Will Cost $28,386
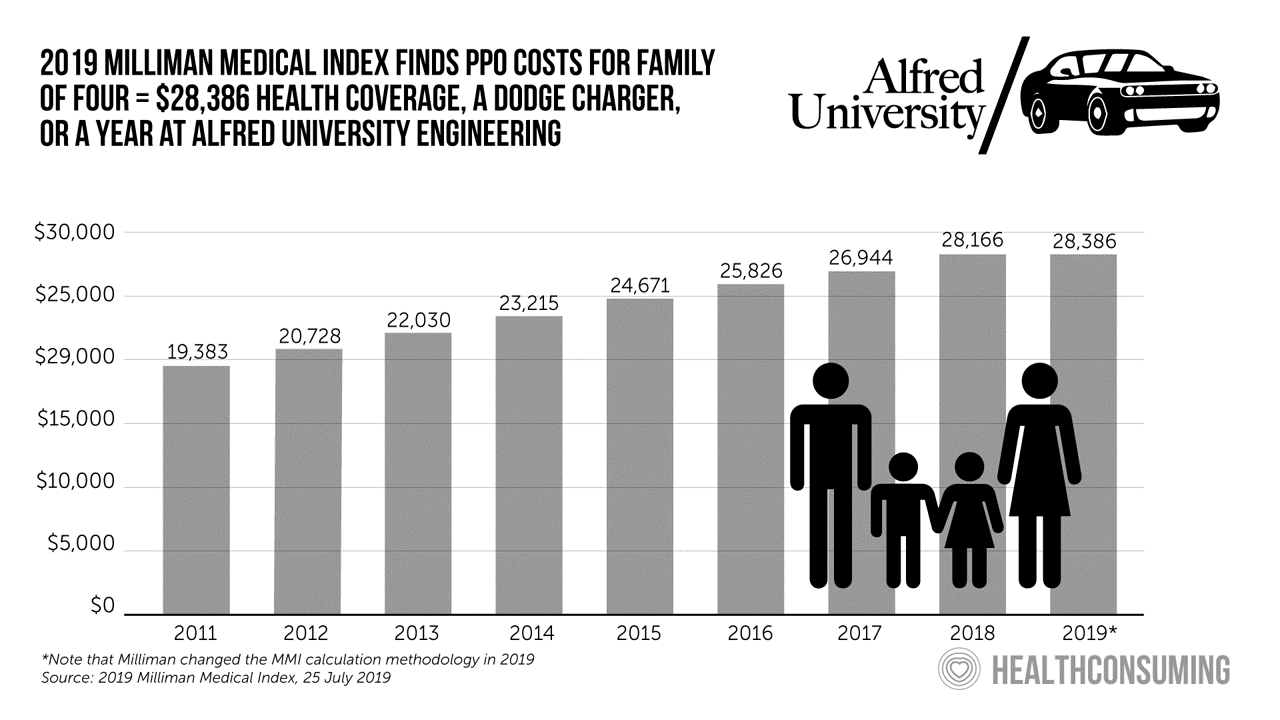
This year, an employer-sponsored PPO for a family of four in the U.S. will cost $28,386, a 3.6% increase over 2018, according to the 2019 Milliman Medical Index (MMI). Based on my annual read of this year’s Index, the PPO costs roughly the same as a new Dodge Charger or a year attending the engineering school at Alfred University. The Milliman MMI team has updated the methodology for the Index; the chart shown here is my own, recognizing that the calculations and assumptions beneath the 2019 data point differ from previous years. The key points of the report are that:
Health Care and the Democratic Debates – Round 2 – Battle Royale for M4All vs Medicare for All Who Want It – What It Means for Industry

Looking at this photo of the 2020 Democratic Party Presidential candidate debater line-up might give you a déjà vu feeling, a repeat of the night-before debate. But this was Round 2 of the debate, with ten more White House aspirants sharing views — sometimes sparring — on issues of immigration, economic justice, climate change, and once again health care playing a starring role from the start of the two-hour event. The line-up from left to write included: Marianne Williamson. author and spiritual advisor John Hickenlooper, former Governor of Colorado Andrew Yang. tech company executive Pete Buttigieg, Mayor of South Bend,
Health Care and the Democratic Debates – Part 1 – Medicare For All, Rx Prices, Guns and Mental Health

Twenty Democratic Presidential candidates each have a handful of minutes to make their case for scoring the 2020 nomination, “debating” last night and tonight on major issues facing the United States. I watched every minute, iPad at the ready, taking detailed notes during the 120 minutes of political discourse conducted at breakneck speed. Lester Holt, Savannah Guthrie, and Jose Diaz-Balart asked the ten candidates questions covering guns, butter (the economy), immigration, climate change, and of course, health care — what I’m focusing on in this post, the first of two-debate-days-in-a-row. The first ten of twenty candidates in this debate were,
Two-Thirds of Americans Say Healthcare Doesn’t Work Well, in RealClear Politics Poll

Health care is the top issue facing the U.S. today, one in three Americans says, with another one-fourth pointing to the economy. Together, health care + the economy rank the top issues for 62% of Americans. Health care and the economy are, in fact, intimately tied in every American’s personal household economy I assert in my book, HealthConsuming: From Health Consumer to Health Citizen. This poll from RealClear Politics, conducted in late April/early May 2019, makes my point that the patient is the consumer and, facing deductibles and more financial exposure to footing the medical bill, the payor. Fully
When Will Self-Service Come to Health Care?

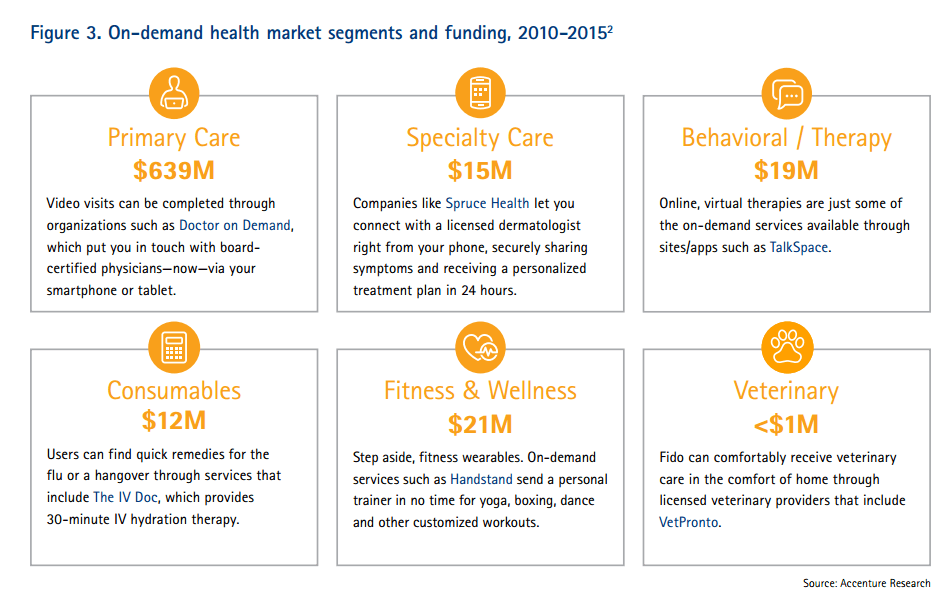
At least one in three people who have tried out virtual health care have done so because they use technology in all aspects of life and want to do the same with their healthcare. This data point has informed my vision for self-care and the home as our health hub, bolstered in part through the research of Accenture from which this first graphic comes. A common theme at health care meetings these days is how and when health care will meet its Amazon, Apple, or Uber moment? Lately, one of my speaking topics is the “Amazon Prime-ing” of health consumers,
Scaling the Social Determinants of Health – McKinsey and Kaiser’s Bold Move

People who are in poor health or use more health care services are more likely to report multiple unmet social needs, such as food insecurity, unsafe neighborhoods, lack of good housing, social isolation, and poor transportation access, found through a survey conducted by McKinsey. The results are summarized in Addressing the Social Determinants of Health. The growing recognition of the influence of social determinants reached a tipping point last week with the news that Kaiser-Permanente would work with Unite US to scale services to people who need them. The mainstreaming of SDoH speaks to the awareness that health is made
Assessing the GAO’s Report on Single-Payer Healthcare in America: Let’s Re-Imagine Workflow

Calls for universal health care, some under the banner of Medicare for All,” are growing among some policy makers and presidential candidates looking to run in 2020. As a response, the Chairman of the House Budget Committee in the U.S. Congress, Rep. John Yarmuth (D-Ky.), asked the Congressional Budget Office (CBO) to develop a report outlining definitions and concepts for a single-payer health care system in the U.S. The result of this ask is the report, Key Design Components and Considerations for Establishing a Single-Payer Health Care System, published on 1st May by the CBO. The report provides
The Convergence of Health/Care and Real Estate

There’s no denying the growth of telehealth, virtual visits, remote health monitoring and mHealth apps in the healthcare landscape. But these growing technologies don’t replace the role of real estate in health, wellness and medical care. Health care is a growing force in retail real estate, according to the ICSC, the acronym for the International Council of Shopping Centers, which has been spending time analyzing, in their words, “what landlords should know in eyeing tenants from a $3.5 trillion industry.” Beyond the obvious retail clinic segment, the ICSC points out a key driving growth lever for its stakeholders, recognizing that,
Americans’ Trust in U.S. Healthcare Lags Tech — and Women Are Particularly Cynical
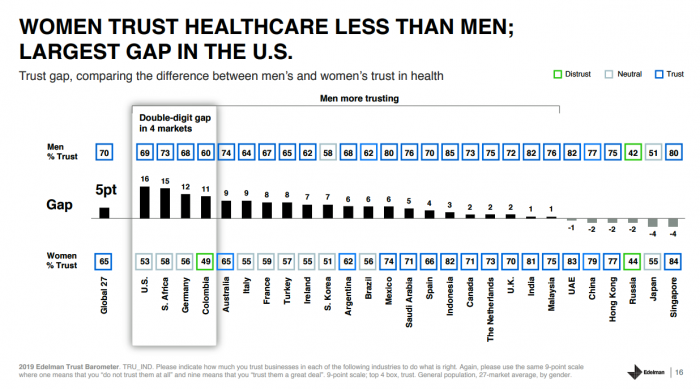
The 2019 Edelman Trust Barometer measured the biggest gap in trust for the healthcare industry between the U.S. “informed public” and the mass population. Fewer American women, too, trust the healthcare industry than men do. “This inequality of trust may be reflective of the mass population continuing to feel left behind as compared to others, even as they recognize the advances that are being made that could benefit them. Given tone and tenor of the day, and particularly among mass population, healthcare may continue to see increasing demands for change and regulation,” Susan Isenberg, Edelman’s head of healthcare, notes in
Health/Care Everywhere – Re-Imagining Healthcare at ATA 2019

“ATA” is the new three-letter acronym for the American Telemedicine Association, meeting today through Tuesday at the Convention Center in New Orleans. Ann Mond Johnson assumed the helm of CEO of ATA in 2018, and she’s issued a call-to-action across the health/care ecosystem for a delivery system upgrade. Her interview here in HealthLeaders speaks to her vision, recognizing, “It’s just stunning that there’s such a lag between what is possible in telehealth and what is actually happening.” I’m so keen on telehealth, I’m personally participating in three sessions at #ATA19. On Monday 15th April (US Tax Day, which is relevant
Medical Costs Are Consuming Americans’ Financial Health
Spending on medical care costs crowded out other household spending for millions of Americans in 2018, based on The U.S. Healthcare Cost Crisis, a survey from West Health and Gallup. Gallup polled 3,537 U.S. adults 18 and over in January and February 2019. One in three Americans overall are concerned they won’t be able to pay for health care services or prescription drugs: that includes 35% of people who are insured, and 63% of those who do not have insurance. Americans borrowed $88 billion in 2018 to pay for health care spending, West Health and Gallup estimated. 27 million Americans
Most Americans Blame Drug Companies, Insurers, and Hospitals for High Health Care Costs

There’s little agreement between Democrats and Republicans on a plethora of issues in American public life. But one issue that brings U.S. citizens together is agreement that the cost of health care is too high in the country, and that pharma, health plans, and providers are to blame. Welcome to health politics in America as of March 2019, according to The Public and High U.S. Health Care Costs, a poll conducted by POLITICO and the Harvard T.H. Chan School of Public Health. The first chart illustrates the common ground shared by Americans by party affiliation, with vast majorities across parties playing
How Genomics Can Battle Killer Bacterial Infections in the Hospital – Talking With Philips at HIMSS19
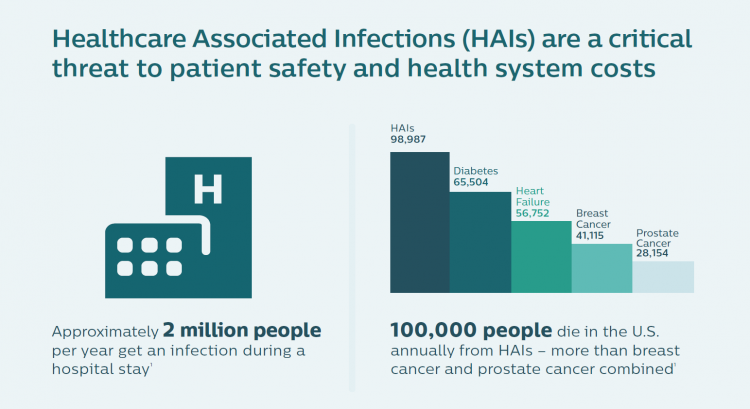
When you think “genomics,” your mind probably pictures a human DNA strand. Well, my mind did, prior to meeting with Dr. Joseph Frassica and Dr. Felix Baader at HIMSS19 to discuss Philips’ approach to the tragic problem of healthcare-acquired infections that kill patients. Ever since that conversation, my mind’s eye is filled with images of MRSA cells like those shown here. At HIMSS19, Philips launched a solution that couples clinical informatics with genomic sequencing of bacteria to quickly identify and treat patients that are affected with tough-to-treat infections that, so often, result in death. Healthcare-acquired infections (HAIs) are a worldwide
National Health Spending Will Reach Nearly 20% of U.S. GDP By 2027
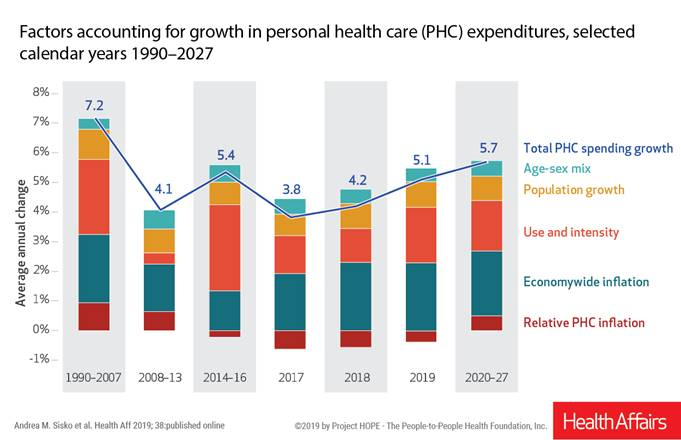
National health spending in the U.S. is expected to grow by 5.7% every year from 2020 to 2027, the actuaries at the Centers for Medicare and Medicaid Services forecast in their report, National Health Expenditure Projections, 2018-2927: Economic And Demographic Trends Drive Spending And Enrollment Growth, published yesterday by Health Affairs. For context, note that general price inflation in the U.S. was 1.6% for the 12 months ending January 2019 according to the U.S. Bureau of Labor Statistics. This growth rate for health care costs exceeds every period measured since the high of 7.2% recorded in 1990-2007. The bar chart illustrates the
“Telehealth is a digital distribution channel for health care” – catching up with Roy Schoenberg, President and CEO of American Well

Ten years ago, two brothers, physicians both, started up a telemedicine company called American Well. They launched their service first in Hawaii, where long distances and remote island living challenged the supply and demand sides of health care providers and patients alike. A decade later, I sat down for a “what’s new?” chat with Roy Schoenberg, American Well President and CEO. In full transparency, I enjoy and appreciate the opportunity to meet with Roy (or very occasionally Ido, the co-founding brother-other-half) every year at HIMSS and sometimes at CES. In our face-to-face brainstorm this week, we covered a wide range
The Expectation Gap Between What Patients Want Vs What They Get
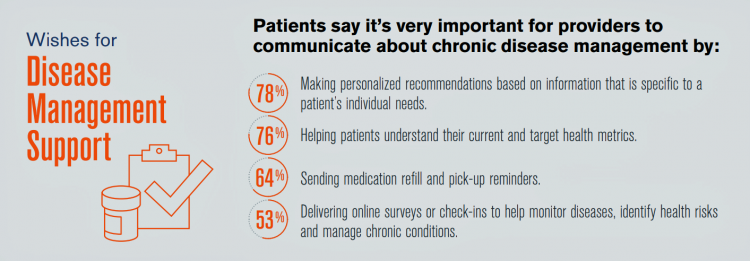
Talk to me, patients are demanding in unison. Most health consumers expect providers to communicate about routine health care and prevention; this is especially true among those patients trying to manage chronic conditions we learn from 10 Ways to Fulfill Patients’ Communication Wish List, a report based on a consumer survey from West, the communications and network infrastructure company. Four in five patients say that talking to “me” means they want personalized recommendations to their unique needs – but only one-third of patients say they’re getting that level of service from their healthcare providers. Most health consumers expect providers to communicate about
Consumers’ and Physicians’ Growing Embrace of Digital Health via PwC
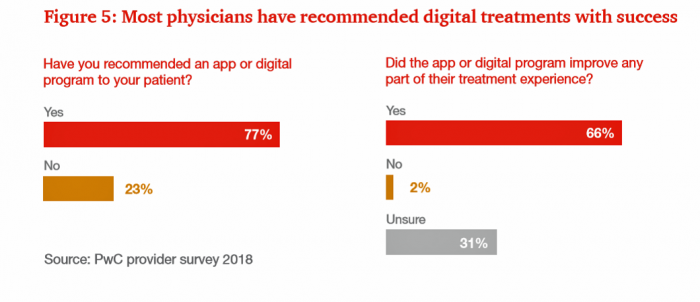
Most consumers would be willing to try an FDA-approved app or online to treat a medical condition, as well as receiving hospital care at home if would be less costly. We’ve reached an inflection point on the demand side among consumers for digital health options, PwC suggests in their report on the New Health Economy coming of age. The report outlines health/care industry issues for 2019, with a strong focus on digital health. Whether a menu of care options including virtual health to access specialists across the U.S., post-hospital virtual visits, or hospital care at-home, a majority of Americans supports
A Smarter Home for Healthy Living at CES 2019….and a nod to Microsoft
Health begins at home. I found evidence for that, beyond my own N of 1 understanding, in a research article published in the UK in 2000 by Lyn Harrison and Frances Heywood. Lyn and Frances tested three assumptions that they believed linked housing and health: that housing contributes to health; that housing is not routinely included in health or social planning;’ and that the potential contribution of primary care is wasted. Their conclusion: that the housing-health link was not receiving the recognition that connection needs. Nearly two decades later, that housing-health link still isn’t universally embraced by health care stakeholders. But
Costs, Consumerism, Cyber and Care, Everywhere – The 2019 Health Populi TrendCast

Today is Boxing Day and St. Stephens Day for people who celebrate Christmas, so I share this post as a holiday gift with well-wishes for you and those you love. The tea leaves have been brewing here at THINK-Health as we prepared our 2019 forecast at the convergence of consumers, health, and technology. Here’s our trend-weaving of 4 C’s for 2019: costs, consumerism, cyber and care, everywhere… Health care costs will continue to be a mainstream pocketbook issue for patients and caregivers, with consequences for payors, suppliers and ultimately, policymakers. Legislators inside the DC Beltway will be challenged by the
Koen Kas, the Gardener of Health Tech Delights
The future of healthcare is not about being sick, Prof. Dr. Koen Kas believes. Having spent many years in life sciences in both research and as an entrepreneur, Koen now knows that getting and staying healthy isn’t about just developing medicines and med-tech: optimally, health requires a tincture of delight, Koen advises in his breakthrough, innovative book, Your Guide to Delight. Healthcare must go beyond traditional user-centered design, Koen’s experience has shown, and aspire toward design-to-delight. The concept of “delight” in healthcare, such as we experience in hospitality, grocery stores, and entertainment, is elusive. I’ve observed this, too, in my
How MedModular Fits Into the New Lower-Cost, High-Quality, Consumer-Enchanted Healthcare World

In American health economics, there’s a demand side and a supply side. On the demand side, we’ve done a poor job trying to nudge patients and consumers toward rational economic decision making, lacking transparency, information symmetry, and basic health literacy. On the supply side, we’ve engaged in a medical arms race allocating capital resources to shinier and shinier new things, often without cost-benefit rationale or clinical evidence. On that supply side, though, I met up with an innovation that can help to bend the capital cost curve of how we envision and build new hospitals and clinics. This week, I
Sicker Consumers Are More Willing to Share Health Data

People dealing with chronic conditions are keener to share personally-generated data than people that don’t have a chronic disease, Deloitte’s 2018 Survey of U.S> Health Care Consumers learned. This and other insights about the patient journey are published in Inside the patient journey, a report from Deloitte that assesses three key touch points for consumer health engagement. These three patient journey milestones are searching for care, using new channels of care, and tracking and sharing health data, Deloitte maps. What drives people to engage on their patient journeys has a lot more to do with practical matters of care like convenience,
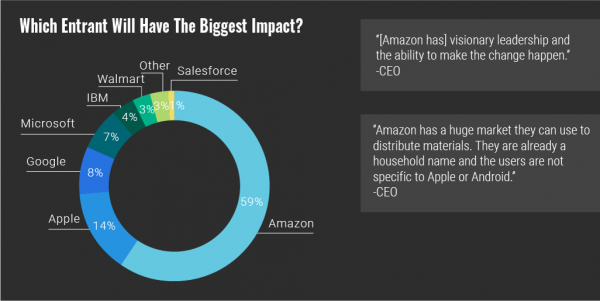
Prescription Drugs: From Costs and Bad Reputation to Civica Rx and Amazon to the Rescue

The prices of medicines prescribed in outpatient settings rose, on average, 10.3% in 2018. Wages increased about 2.6%, and consumer prices, 1.3%, based on the 2019 Segal Health Plan Cost Trend Survey. Segal forecasts that medical cost trends will moderate for 2019, lower than 2018 rates. But to the patient, now feeling like a consumer dealing with high-deductibles and the growing sticker shock of specialty drug prices, a so-called “moderate” trend still feels like a big bite in the household budget. Specifically, specialty drug trend is expected to be 14.3% in 2019, compared with 17.7% in 2018 — still several
Self-Care is Healthcare for Everyday People

Patients are the new healthcare payors, and as such, taking on the role of health consumers. In fact, health and wellness consumers have existed since a person purchased the first toothpaste, aspirin, heating pad, and moisturizing cream at retail. Or consulted with their neighborhood herbalista, homeopathic practitioner, therapeutic masseuse, or skin aesthetician. Today, the health and wellness consumer can DIY all of these things at home through a huge array of products available in pharmacies, supermarkets, Big Box stores, cosmetic superstores, convenience and dollar stores, and other retail channels – increasingly, online (THINK, of course, of Amazon — more on
The Top Pain Point in the Healthcare Consumer Experience is Money

Beyond the physical and emotional pain that people experience when they become a patient, in the U.S. that person becomes a consumer bearing expenses and financial pain, as well. 98% of Americans rank paying their medical bills is an important pain point in their patient journey, according to Embracing consumerism: Driving customer engagement in the healthcare financial journey, from Experian Health. Experian is best known as the consumer credit reporting agency; Experian Health works with healthcare providers on revenue cycle management, patient identity, and care management, so the company has experience with patient finance and medical expense sticker shock. In the
Surprise, Surprise: Most Americans Have Faced a “Surprise” Medical Bill

Most Americans have been surprised by a medical bill, a NORC AmeriSpeak survey found. Who’s responsible? Nearly all Americans (86% net responsible) first blame health insurance companies, followed by hospitals (82%). Fewer U.S. patients blamed doctors and pharmacies, although a majority of consumers still put responsibility for surprise healthcare bills on them (71% and 64% net). Most of the surprise bills were for charges associated with a physician’s service or lab test. Most surprise charges were not due to the service being excluded from a health plans provider network. The poll was conducted among 1,002 U.S. adults 18 and over
Disruption Is Healthcare’s New Normal
Googling the words “disruption” and “healthcare” today yielded 33.8 million responses, starting with “Riding the Disruption Wave in Healthcare” from Bain in Forbes, Accenture’s essay on “Big Bang Disruption in Healthcare,” and, “A Cry for Encouraging Disruption” in the New England Journal of Medicine Catalyst. This last article responded to the question, “Can we successfully deliver better quality care for patients at a lower cost?” asked by François de Brantes, Executive Director of the Health Care Incentives Improvement Institute. “Disruption” as a noun and an elephant in our room has been with us in healthcare since the September/October 2000 issue of
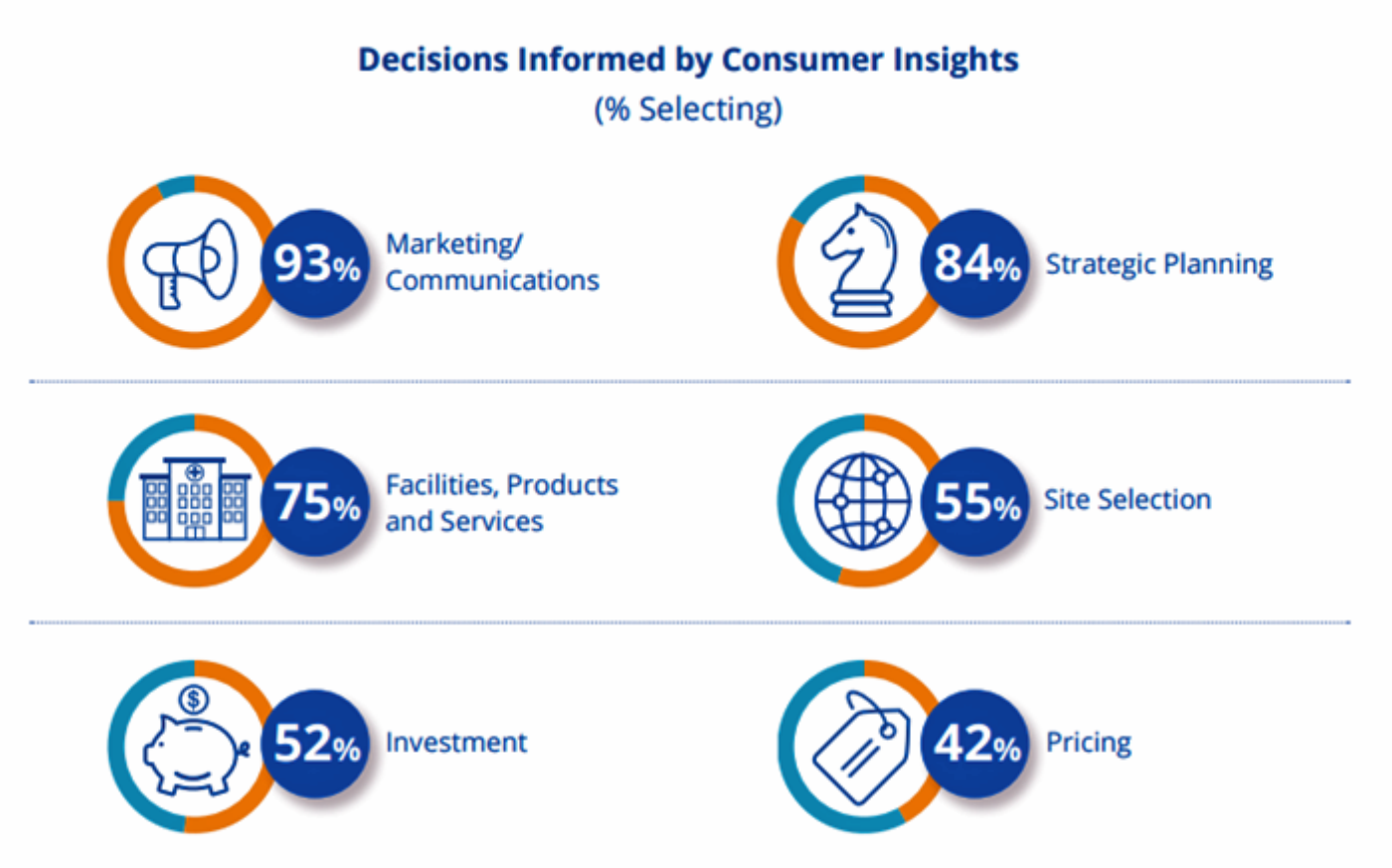
Hospitals Work to Address Customer Experience Gap With Consumers, Kaufman Hall Finds

Hospital and healthcare providers are getting real about improving patient and health consumer experience, the latest Kaufman Hall research finds. The company’s 2018 State of Consumerism in Healthcare report is out, subtitled, “Activity in Search of Strategy.” Kaufman Hall has developed a Healthcare Consumerism Index for healthcare providers based on four pillars: access to care, consumer experience, pricing, and a strong foundation of consumer insights. Based on their assessment of providers on these components, Kaufman Hall found identified four tiers of performance: The top-performing group, Tier 1, includes only 8% of providers. These are the early adopters who allocate resources
Patients have ambitious health goals, and look to doctors for help

Consumers have health goals across many dimensions, topped with eating well, getting fit, reducing stress, sleeping better, feeling mentally well, and improving personal finances. That’s an ambitious health-and-wellness list, identified in the Health Ambitions Study, the first such research Aetna has published. Six in ten people are looking to food and nutrition for health, whether as “medicine” to deal with chronic conditions, for weight loss or general wellness, which is a frequent theme here on Health Populi. Consumers embrace their food habits as a key self-care determinant of health. Fitness, cited by most consumers, is also a can-do, self-powered activity
As Medical Cost Trend Remains Flat, Patients Face Growing Health Consumer Financial Stress

When it comes to healthcare costs, lines that decline over time are generally seen as good news. That’s how media outlets will cover the top-line of PwC’s report Medical cost trend: Behind the numbers 2019. However, there are other forces underneath the stable-looking 6.0% medical trend growth projected for 2019 that will impact healthcare providers, insurers, and suppliers to the industry. There’s this macro-health economic story, and then there’s the micro-economics of healthcare for the household. Simply put: the impact of growing financial risk for healthcare costs will be felt by patients/consumers themselves. I’ve curated the four charts from the
Pope Francis is a Public Health Advocate

“The world today is mostly deaf,” the Pontiff observes in Pope Francis: A Man of His Word, Wim Wenders’ documentary on this religious leader who likes to quote Dostoevsky, joke about mothers-in-law, and advocate for the sick, the poor, the disenfranchised, and Planet Earth. He is, I realized while watching this film and hearing this man of words, a public health advocate. Throughout the film, we see clips of Pope Francis washing the feet of prisoners in Philadelphia, comforting dying children in a pediatric clinic in central Africa, and speaking out to the U.S. Congress about the dangers of climate
Doing Less Can Be Doing More for Healthcare – the Biggest Takeaway From ASCO 2018

Less can lead to more for so many things: eating smaller portions, lowering sugar consumption, and driving less in favor of walking or cycling come to mind. When it comes to healthcare utilization, doing less can also result in equal or even better outcomes. Groundbreaking research presented at this week’s ASCO meeting found that some women diagnosed with certain forms of cancer do not benefit from undergoing chemotherapy. The American Society of Clinical Oncology (ASCO) is one of the largest medical meetings annually, and at this huge meeting these research results for the TAILORx trial were huge news with big
Health Care for a Typical Working Family of Four in America Will Cost $28,166 in 2018
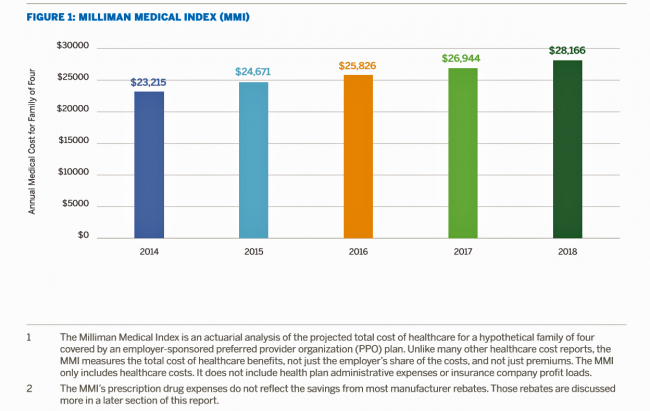
What could $28,166 buy you in 2018? A new car? A year of your child’s college education? A plot of land for your retirement home? Or a year of healthcare for a family of four? Welcome to this year’s edition of the Milliman Medical Index (MMI), one of the most important forecasts of the year in the world of the Health Populi blog and THINK-Health universe. That’s because we’re in the business of thinking about the future of health and health care through the health economics lens; the MMI is a key component of our ongoing environmental analysis of the
Consumers Shop Food for Health, But Cost Is a Barrier to Healthy Eating
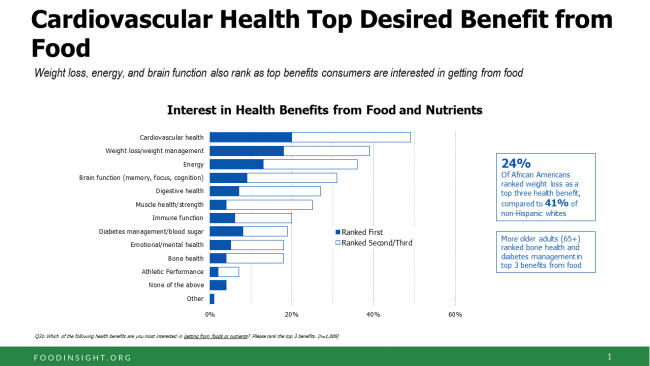
One-third of Americans are following a specific eating pattern, including intermittent fasting, paleo gluten-free, low-carb, Mediterranean diet, and Whole 30, among dozens of other food-styles in vogue in 2018. It’s mainstream now that Americans are shopping food for health, with eyes focused on heart health, weight, energy, diabetes, and brain health, according to the 2018 Food & Health Survey from IFIC, the International Food Industry Council Foundation. But underneath these healthy eating intentions are concerns about the cost of nutritious foods, IFIC reports. And this aspect of home health economics can sub-optimize peoples’ health. Consider the first graph on consumers’
Having Health Insurance Is a Social Determinant of Health: the implications of growing uninsured in the U.S.
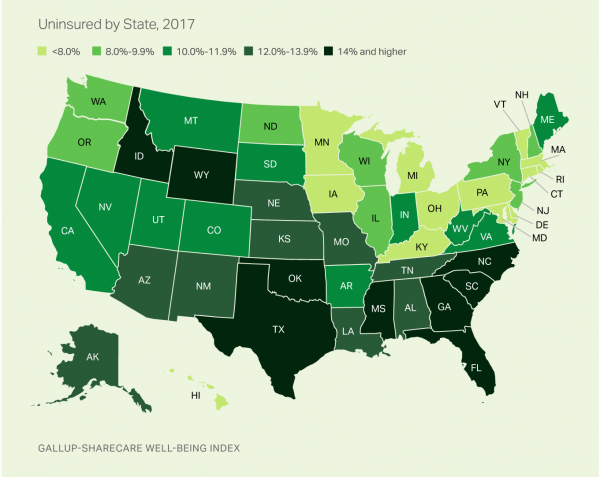
The rolls of the uninsured are growing in America, the latest Gallup-Sharecare Poll indicates. The U.S. uninsurance rate rose to 12.2% by the fourth quarter of 2017, up 1.3 percentage points from the year before. 2017 reversed advancements in health insurance coverage increases since the advent of the Affordable Care Act, and for the first time since 2014 no states’ uninsured rates fell. The 17 states with declines in insurance rates were Arizona, Colorado, Florida, Hawaii, Illinois, Indiana, Iowa, Missouri, New Mexico, New York, North Carolina, South Carolina, Texas, Utah, Washington, West Virginia, Wisconsin, and Wyoming. Among these, the greatest
Healthcare Information In-Security Is the New Normal

Three-fourths of healthcare providers experienced a data breach in 2017, according to the HIMSS 2018 Cybersecurity Survey. Health data insecurity is the new normal. A big piece of addressing the cybersecurity healthcare challenge is educating people who work in healthcare settings, and that has been under-funded. Only 41% of healthcare workers say they receive security training, a Forrester study learned in January 2018. Forrester also found that while healthcare organizations have experienced some of the most egregious cyberattacks, the industry allocates a smaller proportion of IT budgets to security compared with than other organizational types at a rate of 22%
Americans’ Trust in the Healthcare System Low Compared to Rest-of-World’s Health Citizens
In the U.S., trust in the healthcare industry declined by 9 percentage points in just one year, declining from 62% of people trusting — that’s roughly two-thirds of Americans — down to 53% — closer to one-half of the population. I covered the launch of the 2018 Edelman Trust Barometer across all industries here in Health Populi in January 2018, when this year’s annual report was presented at the World Economic Forum in Davos as it is each year. The Edelman team shared this detailed data on the healthcare sector with me this week, for which I am grateful. Check
How We Spend Versus What We Get: America’s Healthcare Spending Makes for Poor Health
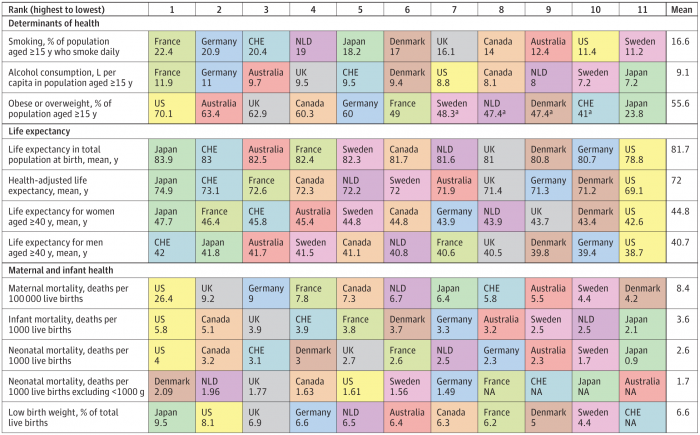
The U.S. spent nearly twice as much as other wealthy countries on healthcare, mostly due to higher prices for both labor and products (especially prescription drugs). And, America spends more on administrative costs compared to other high-income countries. What do U.S. taxpayers get in return for that spending? Lower life spans, higher maternal and infant mortality, and the highest level of obesity and overweight among our OECD peer nations. These sobering statistics were published in Health Care Spending in the United States and Other High-Income Countries this week in JAMA, the Journal of the American Medical Association. The study analyzes
The $4 Trillion Health Economy of 2020
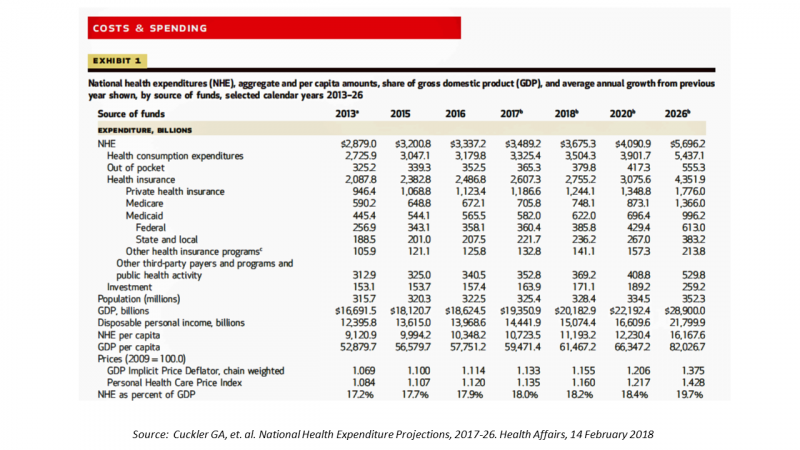
In 2020, national health expenditures (NHE) in the United States will exceed $4 trillion to cover 334.5 million Americans. That equates to 18.4% of the Gross Domestic Product (GDP) and $12,230.40 of health spending per person. I sat in on a press call today with researchers from the Office of the Actuary working in the Centers for Medicare and Medicaid Services (CMS) to review the annual forecast of the NHE, published in Health Affairs in a statistically-dense eleven page article titled, National Health Expenditure Projections, 2017-2026: Despite Uncertainty, Fundamentals Primarily Drive Spending Growth. What are those “fundamentals” pushing up healthcare spending?
The United States of Care Launches to Promote Healthcare for All of US

Let’s change the conversation and put healthcare over politics. Sounds just right, doesn’t it? If you’re reading Health Populi, then you’re keen on health policy, health economics, most of all, patients: now playing starring roles as consumers, caregivers, and payors in their own care. Andy Slavitt, former Acting Administrator of the Centers for Medicare and Medicaid Services (CMS), has assembled a diverse group of health care leaders who care about those patients/people, too, appropriately named the United States of Care. Founders include Dr. Bill Frist, former Republican U.S. Senator from Tennessee, Dave Durenberger, former Republican U.S. Senator from Minnesota, and
The 2018 Edelman Trust Barometer – What It Means for Health/Care in America

Trust in the United States has declined to its lowest level since the Edelman Trust Barometer has conducted its annual survey among U.S. adults. Welcome to America in Crisis, as Edelman brands Brand USA in 2018. In the 2018 Edelman Trust Barometer, across the 28 nations polled, trust among the “informed public” in the U.S. “plunged,” as Edelman describes it, by 23 points to 45. The Trust Index in America is now #28 of 28 countries surveyed (that is, rock bottom), dropping below Russia and South Africa. “The public’s confidence in the traditional structures of American leadership is now fully
In the U.S., Spend More, Get Less Health Care: the Latest HCCI Data

Picture this scenario: you, the consumer, take a dollar and spend it, and you get 90 cents back. In what industry is that happening? Here’s the financial state of healthcare in America, explained in the 2016 Health Care Cost and Utilization Report from the Health Care Cost Institute (HCCI). We live in an era of Amazon-Primed consumers, digital couponing, and expectations of free news in front of paywalls. We are all in search of value, even as the U.S. economy continues to recover on a macroeconomic basis. But that hasn’t yet translated to many peoples’ home economics. In this personal
Hug Your Physician: S/He Needs It – Listening to the 2018 Medscape National Physician Burnout & Depression Report

Two in five U.S. physicians feels burned out, according to the Medscape National Physician Burnout & Depression Report for 2018. This year, Medscape explicitly adds the condition of “depression” to its important study, and its title. In 2017, the Medscape report was about bias and burnout. Physicians involved in primary care specialties and critical care are especially at-risk for burnout, the study found. One in five OBGYNs experience both burnout and depression. Furthermore, there’s a big gender disparity when it comes to feeling burned out: nearly one-half of female physicians feel burnout compared with 38% of male doctors. Being employed by
Healthy Living in Digital Times at CES 2018

Connecting Life’s Dots, the organization Living in Digital Times partners with CES to deliver conference content during the show. At CES 2018, LIDT is connecting a lot of dots to help make health streamline into daily living. Robin Raskin, founder, kicked off LIDT’s press conference setting the context for how technology is changing lifestyles. Her Holy Grail is to help make tech fun for everybody, inclusive for everybody, and loved by everybody, she enthused. LIDT has been a presence at CES for many years, conceiving the contest the Last Gadget Standing, hosting tech-fashion shows with robots, and supporting a young innovators
What Healthcare Can Learn from Volkswagen: A Scenario of a Post-Healthcare World

As I am finalizing my schedule for meet-ups at CES in Las Vegas for early January 2018, I’m thinking about digital devices and wearable tech, connected cars, smart homes, and the Internet of Things through my all-health, all-the-time lens. My friends at TrendWatching write today about the automaker, Volkswagen, which has a division called MOIA started in 2016. VW, like most car manufacturers, is working on strategies to avoid being disrupted and made irrelevant as tectonic forces like autonomous cars and shared rides innovate and re-define the nature of personal transportation. MOIA is a brand and a self-described “social movement.”
Health Consumers Face the New Year Concerned About Costs, Security and Caring – Health Populi’s 2018 Forecast
As 2018 approaches, consumers will gather healthy New Year’s Resolutions together. Entering the New Year, most Americans are also dealing with concerns about healthcare costs, cybersecurity, and caring – for physical health, mental stress, and the nation. Healthcare costs continue to be top-of-mind for consumer pocketbook issues. Entrenched frugality is the new consumer ethos. While the economy might be statistically improving, American consumers’ haven’t regained confidence. In 2018, frugality will impact how people look at healthcare costs. 88% of US consumers are likely to consider cost when selecting a healthcare provider, a Conduent survey found. Physicians know this: 81% of
Will Getting Bigger Make Hospitals Get Better?
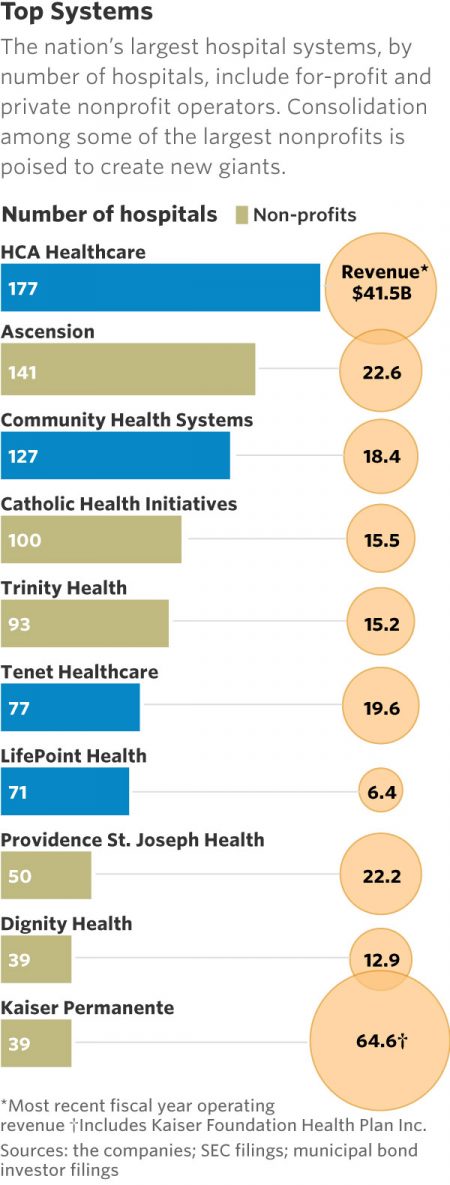
This month, two hospital mega-mergers were announced between Ascension and Providence, two of the nation’s largest hospital groups; and, between CHI and Dignity Health. In terms of size, the CHI and Dignity combination would create a larger company than McDonald’s or Macy’s in terms of projected $28 bn of revenue. (Use the chart of America’s top systems to do the math). For context, other hospital stories this week discuss in southern New Jersey. And this week, the New Jersey Hospital Association annual report called the hospital industry the “$23.4 billion economic bedrock” of the state. Add a third important item
The Patient as Payor – Consumers and the Government Bear the Largest Share of Healthcare Spending in America
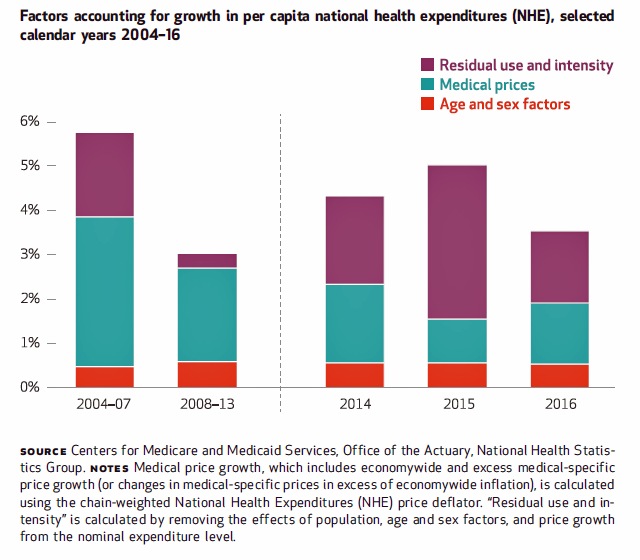
The biggest healthcare spenders in the United States are households and the Federal government, each responsible for paying 28% of the $3.3 trillion spent in 2016. Private business — that is, employers covering healthcare insurance — paid for 20% of healthcare costs in 2016, based on calculations from the CMS Office of the Actuary’s report on 2016 National Health Expenditures. The positive spin on this report is that overall national health spending grew at a slower rate in 2016, at 4.3% after 5.8% growth in 2015. This was due to a decline in the growth rates for the use of
Six Healthcare News Stories to Keep Hospital CFOs Up At Night
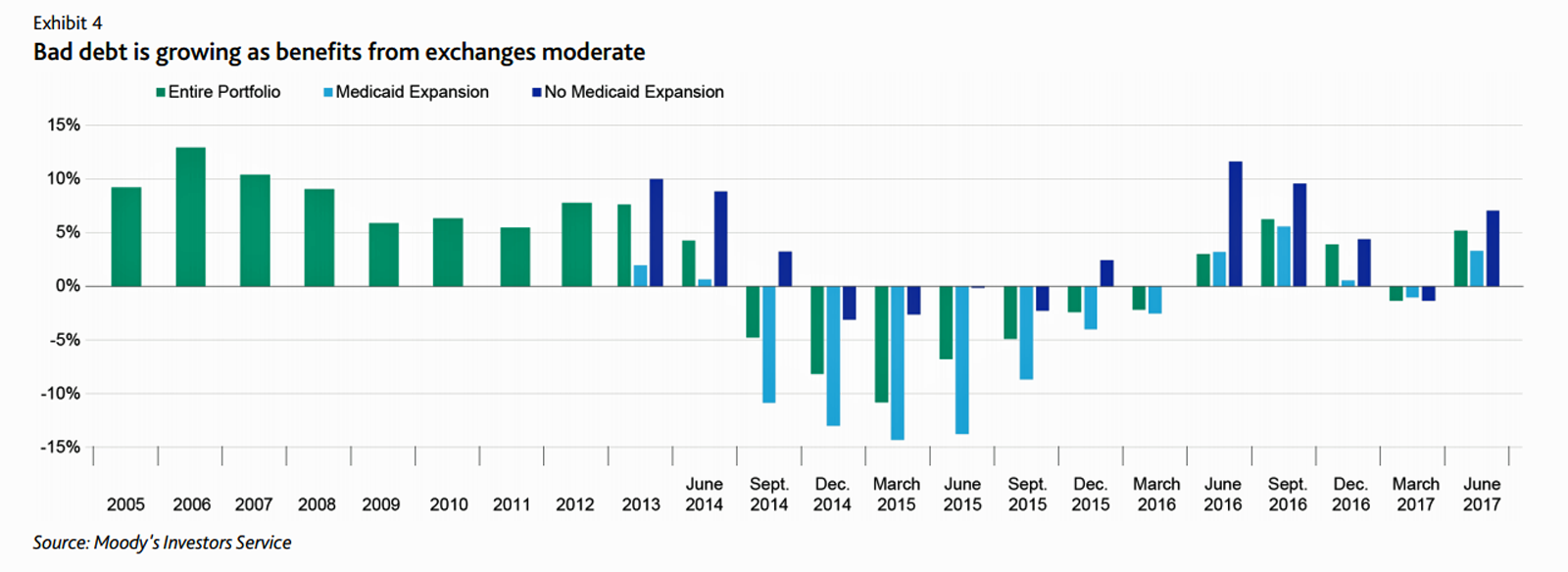
At this moment, the healthcare job I’d least like to have is that of a non-profit hospital Chief Financial Officer (CFO). Five news stories, published in the past 24 hours, tell the tale: First, Moody’s forecast for non-profit hospitals and healthcare in 2018 is negative due to reimbursement and expense pressures. The investors report cited an expected contraction in cash flow, lower reimbursement rates, and rising expense pressures in the midst of rising bad debt. Second, three-quarters of Federally Qualified Health Centers plan to lay off staff given lack of budget allocations resulting from Congressional inaction. Furthermore, if the $3.6
Health (Healthcare, Not So Much) Abounds in Prophet’s Top 50 Brands

U.S. consumers’ most-valued brands include Apple, Google, Amazon, Netflix, Pinterest, Android, Spotify, PIXAR, Disney and Samsung, according to the 2017 Brand Relevance Index from Prophet. The top 50 are shown in the first chart. On the second chart, I’ve circled in red the brands that have reach into healthcare, health, fitness, and wellness. Arguably, I could have circled every brand in the top 50 because in one way or another, depending on the individual, people find health “everywhere” that’s relevant to them based on their own definitions and value-systems. This is Prophet’s third year conducting this study, and I was
What Patients Feel About Technology, Healthcare Costs and Social Determinants
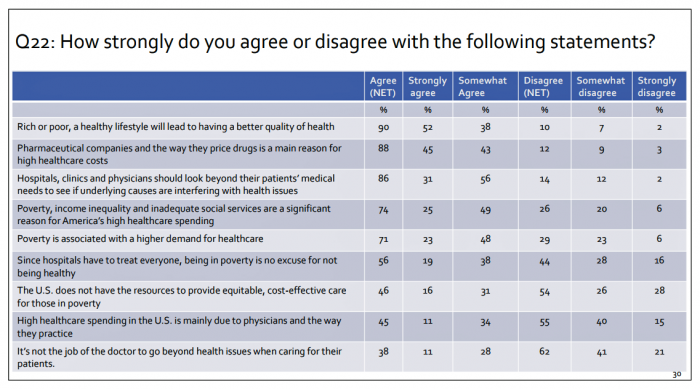
U.S. consumers feel positive about the roles of technology and social determinants in improving healthcare, but are concerned about costs, according to the 2017 Patient Survey Report conducted for The Physicians Foundation. The survey gauged patients’ perspectives across four issues: the physician-patient relationship, the cost of healthcare, social determinants of health, and lifestyle choices. Two key threads in the research explain how Americans feel about healthcare in the U.S. at this moment: the role of technology and the cost of health care. First, the vast majority of consumers view technology, broadly defined, as important for their health care. 85% of people
2017 Rx Cost Trend Over 5 Times U.S. Inflation, Segal Projects
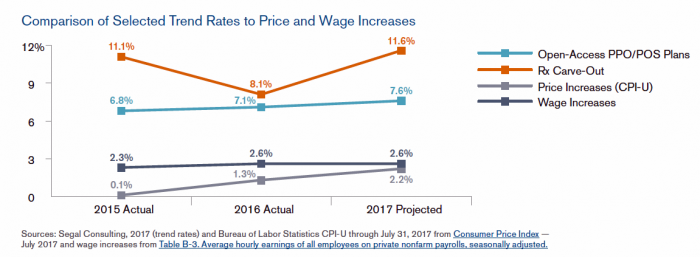
Driven by price increases, costs for the prescription drug benefit carve-out will increase 11.6% this year, based on Segal Consulting’s survey report, High Rx Cost Trends Projected to Be Lower for 2018, published today. The report is accessible on the Segal Co. website. While the Segal team expects prescription drug (Rx) benefit plan cost trends to be “less severe” in 2018, Rx cost increases is a top priority for many sponsors of health plans as their rate of increase far exceeds those for inpatient hospital claims or physician expense. Drug costs continue to be the fastest-growing line item in health
Patients’ Healthcare Payment Problems Are Providers’, Too
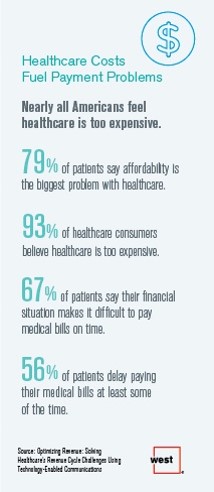
Three-quarters of patients’ decisions on whether to seek services from healthcare providers are impacted by high deductible health plans. This impacts the finances of both patients and providers: 56% of patients’ payments to healthcare providers are delayed some of the time, noted in Optimizing Revenue: Solving Healthcare’s Revenue Cycle Challenges Using Technology Enabled Communications, published today by West. Underneath that 56% of patients delaying payments, 12% say they “always delay” payment, and 16% say they “frequently delay” payment. West engaged Kelton Global to survey 1,010 U.S. adults 18 and over along with 236 healthcare providers to gauge their experiences with
The Digital Gap in Health Consumer/Patient Experience

9 in 10 hospitals and health systems prioritize improving the consumer/patient experience, but only 30% of providers are building these capabilities. This consumer experience gap was found by Kaufman Hall in their survey research published in the report, 2017 State of Consumerism in Healthcare: Slow Progress in Fast Times. Digital health innovations will play big roles in supporting that consumer health experience for most health providers: 58% prioritize offering digital tool and information for consumer engagement, and 56% of providers look to develop a range of virtual/telehealth access points. But it appears that while healthcare providers’ spirits are willing, their flesh
Health Equity Lessons from July 23, 1967, Detroit
On July 23, 1967, I was a little girl wearing a pretty dress, attending my cousin’s wedding at a swanky hotel in mid-town Detroit. Driving home with my parents and sisters after the wedding, the radio news channel warned us of the blazing fires that were burning in a part of the city not far from where we were on a highway leading out to the suburbs. Fifty years and five days later, I am addressing the subject of health equity at a speech over breakfast at the American Hospital Association 25th Annual Health Leadership Summit today. In my talk,
Weaving Accenture’s Five Digital Health Technology Trends for 2017

Technology should serve people, and Accenture has identified five major key trends that, together, could forge a person-centered, -friendly, -empowering healthcare system. This is Accenture’s Digital Health Technology Vision for 2017. “Should” and “could” are the important adverbs here, because if tech doesn’t deliver, driving efficiency and effectiveness, personalizing medical treatments, and inspiring people to become more health literate and health-engaging, then tech is just a Field of Dreams being built and available, with no people taking advantage of the potential benefits. The five new-new tech trends are: AI is the new UI, where healthcare experience is everything Ecosystem power
Is There Political Will for Healthcare Access in the US?
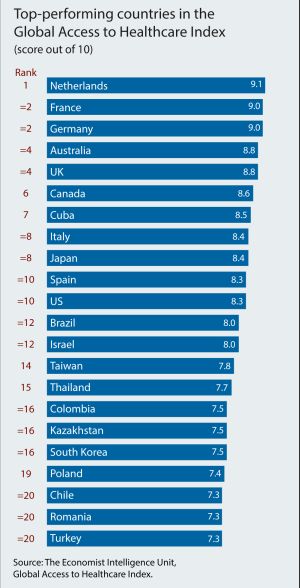
The Netherlands, France and Germany are the best places to be a patient, based on the Global Access to Healthcare Index, developed by the Economist Intelligence Unit (EIU). Throughout the world, nations wrestle with how to provide healthcare to health citizens, in the context of stretched government budgets and demand for innovative and accessible services. The Global Access to Healthcare Index gauges countries’ healthcare systems in light of peoples’ ability to access services, detailed in Global Access to Healthcare: Building Sustainable Health Systems. The United States comes up 10th in line (tied with Spain) in this analysis. Countries that score the
The Pursuit of Health Equity and the State of U.S. Health Care
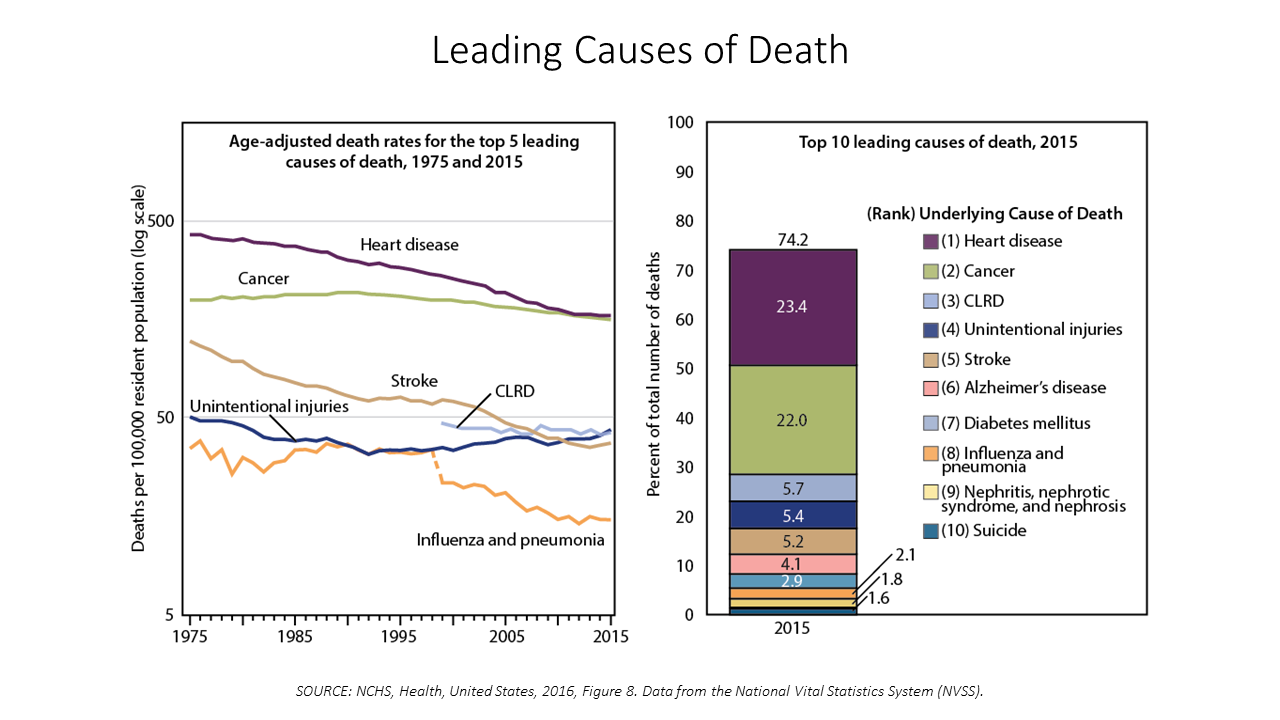
Between 2014 and 2015, death rates increased for eight of the ten leading causes; only death rates caused by cancer fell, and mortality rates for influenza and pneumonia stayed flat. The first chart paints this sobering portrait of Americans’ health outcomes, presented in the CDC’s data-rich 488-page primer, Health, United States, 2016. Think of this publication as America’s annual report on health. Every year, it is prepared and submitted to the President and Congress by the Secretary of the Department of Health and Human Services. This year’s report was delivered by DHHS Secretary Tom Price to President Trump and the
Costs of Healthcare Top Americans’ Financial Concerns: It’s Financial Health Matters Day
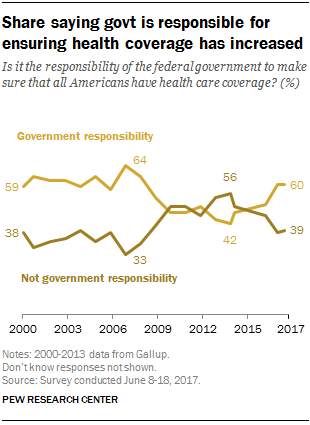
Americans are most worried about healthcare costs among all financial concerns; most people in the U.S. also believe the Federal government should ensure that all people have health coverage. Two polls published in the past week point to the fact that most U.S. health citizens are concerned about health care for themselves and their families, driving a growing proportion of people to favor a single-payer health system. The first line chart illustrates a dramatic trajectory up of the number of American identifying healthcare costs as their #1 financial problem, rising from 10% of people in 2013 to 17% in 2017.
Consumer Experience Is An Integral Part of the Healthcare Experience
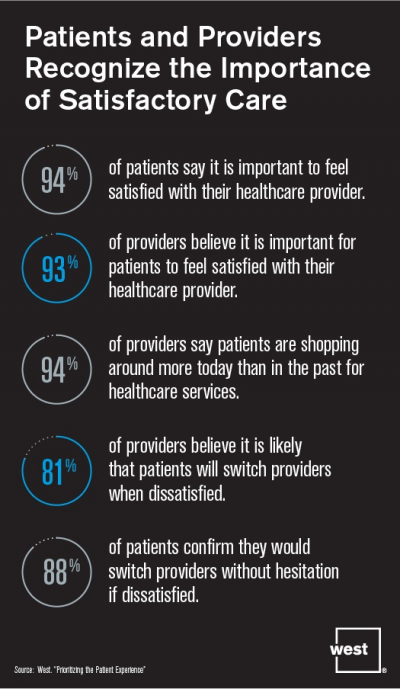
Patient satisfaction should be baked into healthcare provider service goals, according to Prioritizing the Patient Experience from West Corporation, the communications company. West is in the business of improving communications systems, and has a vested interest in expanding comms in health. This research polled patients and providers to assess how each healthcare stakeholder perceives various patient satisfaction issues, which when done well are grounded in sound communications strategy and technologies. Patient satisfaction is directly linked to the bottom lines of healthcare organizations, West contends, due to two key drivers: Evolving payment models are increasingly tying patient satisfaction to reimbursements; and,
Pharmacy and Outpatient Costs Will Take A Larger Portion of Health Spending in 2018
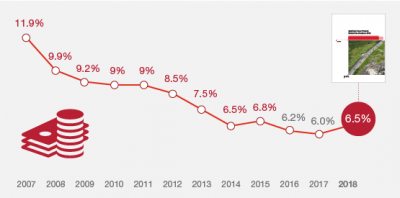
Health care costs will trend upward by 6.5% in 2018 according to the forecast, Medical Cost Trends: Behind the Numbers 2018, from PwC’s Health Research Institute. The expected increase of 6.5% is a half-percentage point up from the 2017 rate of 6.0%, which is 8% higher than last year’s rate matching that of 2014. PwC’s Health Research Institute has tracked medical cost trends since 2007, as the line chart illustrates, when trend was nearly double at nearly 12%. The research consider medical prices, health care services and goods utilization, and a PwC employer benefit cost index for the U.S. The key
U.S. Consumers Expect, But Don’t See, Innovation From the Health & Wellness Industry
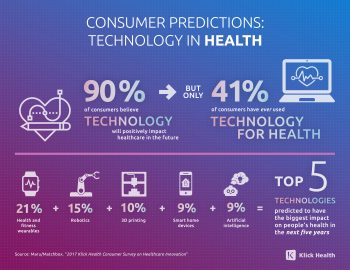
U.S. consumers consider Consumer Electronics to be the most innovative industry they know. But people believe that Health & Wellness should be the most innovative sector in the economy. Welcome to the 2017 Klick Health Consumer Survey, which focuses on health innovation in the context of peoples’ hopes for technology to improve health and healthcare. 1 in 2 people say that technology has had a positive impact on their health and wellness, skewing slightly more toward younger people (although 45% of people 55 years of age and older agree that tech positively contributes to health. 41% of consumers say they’ve
Digital Healthcare At the Inflection Point, Via Mary Meeker
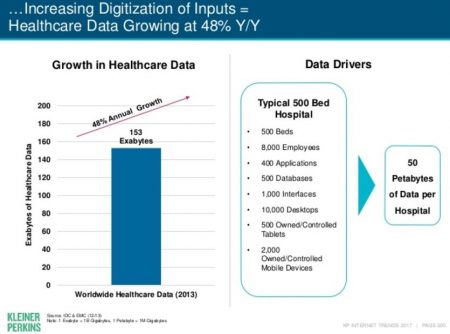
Healthcare is at a digital inflection point, asserts Internet Trends 2017 – Code Conference, by the iconic Mary Meeker of Kleiner Perkins. Published May 31, 2017, few tech-focused reports have the gravitas or generate the readership that this report does. I’m one of Meeker’s perennial readers, covering this report through my health/care lens here on Health Populi for several years (links to previous posts below). Of the report’s 355 pages, 22 are devoted to healthcare (pages 288-319), a section curated by Noah Kaufman of KP. This section of the report assembles data from a range of publicly available sources,
Most Physicians Say Patients, Doctors and Hospitals Are All Losers Under Trump
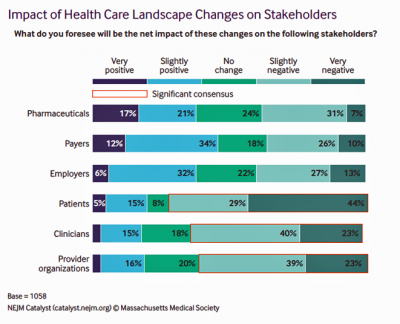
“Overall, Council members express pessimism about the health are landscape in the wake of the Trump administration’s proposed plans, citing no clear winners, only losers: patients, clinicians, and provider organizations.” This is the summary of the Leadership Survey report, Anticipating the Trump Administration’s Impact on Health Care, developed by the New England Journal of Medicine‘s NEJM Group. The first chart illustrates the “biggest healthcare losers” finding, detailed on the bottom three bars of patients, clinicians, and provider organizations. The stakeholders that will fare best under a President Trump healthcare agenda would be drug companies, payers, and employers. The biggest loser
Valuing Children = Valuing Health: Learning From Florence, Italy

This week I celebrate two spring holy holidays in one city that embraces spirituality, civility, and culture: Florence, Italy. Today, I had the special opportunity to tour Ospedale degli Innocenti: the Hospital of the Innocents. The hospital is now an institute for studying the culture and economics of children, and a museum telling a unique story of Florentine babies born in the early 15th century, spanning our contemporary era. The founding and root history of this beautiful place has lessons to teach us even today. It is key to realize, first, that Florentine humanism exalted the ideal virtues of the
Americans Are Not Sold On the American Health Care Act
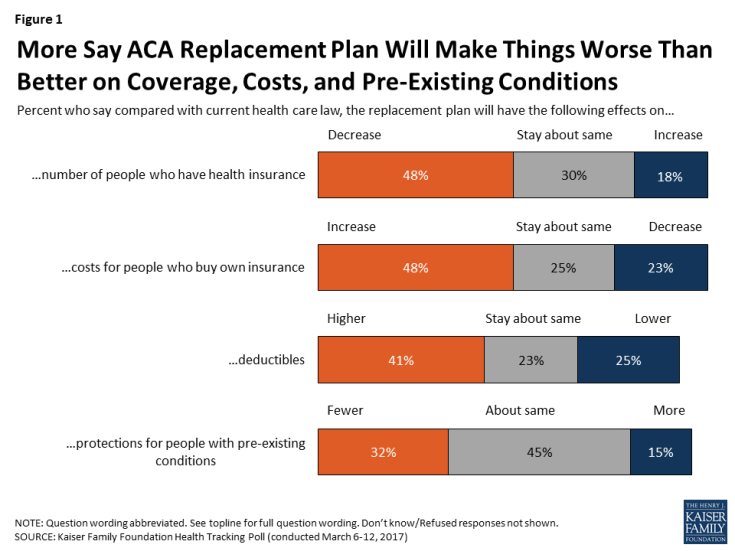
Most Americans do not believe that TrumpCare, the GOP plan to replace the Affordable Care Act (the ACA, aka ObamaCare), will make things better for U.S. health citizens when it comes to peoples’ health insurance coverage, the premium costs charged for those health plans, and protections for people with pre-existing medical conditions. The March 2017 Kaiser Family Foundation Health Tracking Poll examined U.S. adults’ initial perceptions of AHCA, the American Health Care Act, which is the GOP’s replacement plan for the ACA. There are deep partisan differences in perceptions about TrumpCare, with more Republicans favorable to the plan — although not
From EHRecords to EHDelivery: Talking With Dr. Roy Schoenberg of American Well

Telehealth has come of age at HIMSS in 2017. No longer is the concept relegated to footnote or edge-booth status on the conference floor. Instead, telehealth, broadly defined, is now a mainstream concept embraced by healthcare providers, payors and, increasingly, consumers. I spent time brainstorming telehealth with one of the pioneers of modern telehealth in the U.S., Dr. Roy Schoenberg, who co-founded American Well with his brother Ido Schoenberg, in 2007. As such, the company is among the most mature telehealth entities operating in America, delivering live video health visits to millions of health consumers through the American Well telehealth
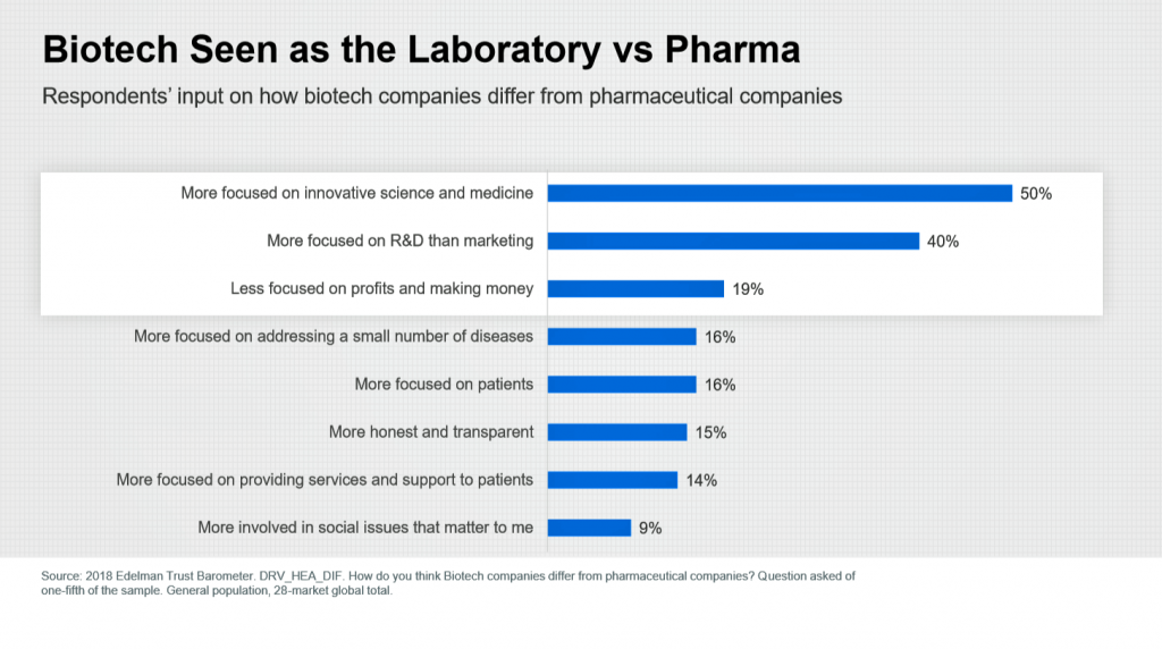
Pharma’s Branding Problem – Profits Over Patients
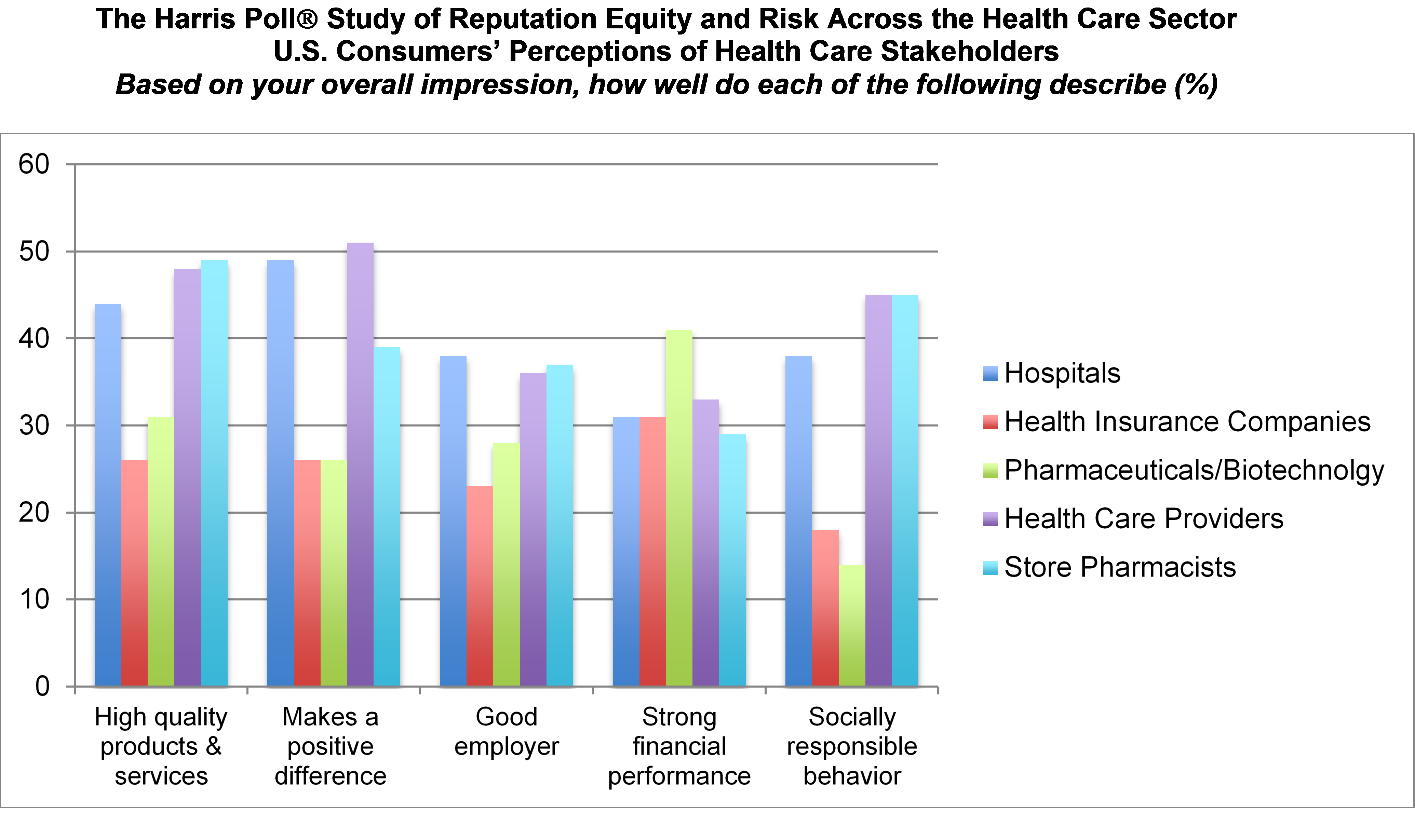
Nine in 10 U.S. consumers think pharma and biotech put profits above patient interests, according to the latest Harris Poll studying reputation equity across organizations serving health care. Notice the relatively low position of the green bars in the first chart (with the exception of the impression for “strong financial performance); these are the pharma/biotech consumer impressions. The health industry stakeholders consumers believe would more likely place them above making money are health care providers, like doctors and nurses, hospitals, and pharmacists. Health insurance companies fare somewhat better than pharma and biotech in this Poll, although rank low on social
Retail Trumps Healthcare in 2017: the Health Populi Forecast for the New Year

Health citizens in America will need to be even more mindful, critical, and engaged healthcare consumers in 2017 based on several factors shaping the market; among these driving forces, the election of Donald Trump for U.S. president, the uncertain future of the Affordable Care Act and health insurance, emerging technologies, and peoples’ growing demand for convenience and self-service in daily life. The patient is increasingly the payor in healthcare. Bearing more first-dollar costs through high-deductible health plans and growing out-of-pocket spending for prescription drugs and other patient-facing goods and services, we’re seeking greater transparency regarding availability, cost and quality of
The Shift to Healthcare Value in a Post-Trump America, via PwC
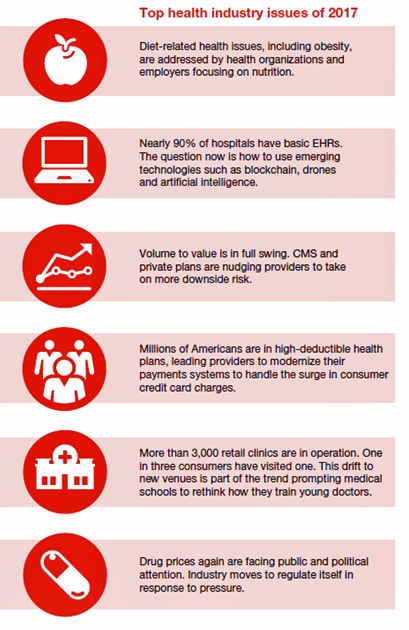
In President Donald Trump’s preliminary thoughts about health care in America, the landscape would feature a mix of tax credits, health savings accounts, high-risk pool, state Medicaid block grants, and regulatory control shifting from the Federal government to the states, according to PwC’s forecast for the new year, Top health industry issues of 2017. PwC frames the 2017 top healthcare issues under the overall strategic imperative of value, with three categories: Adapting for value Innovating for value Building for value. The ten top issues that will shape U.S. healthcare for the next year, PwC expects, will be: An uncertain fate for the
U.S. Healthcare Spending Hit Nearly $10,000 A Person In 2015
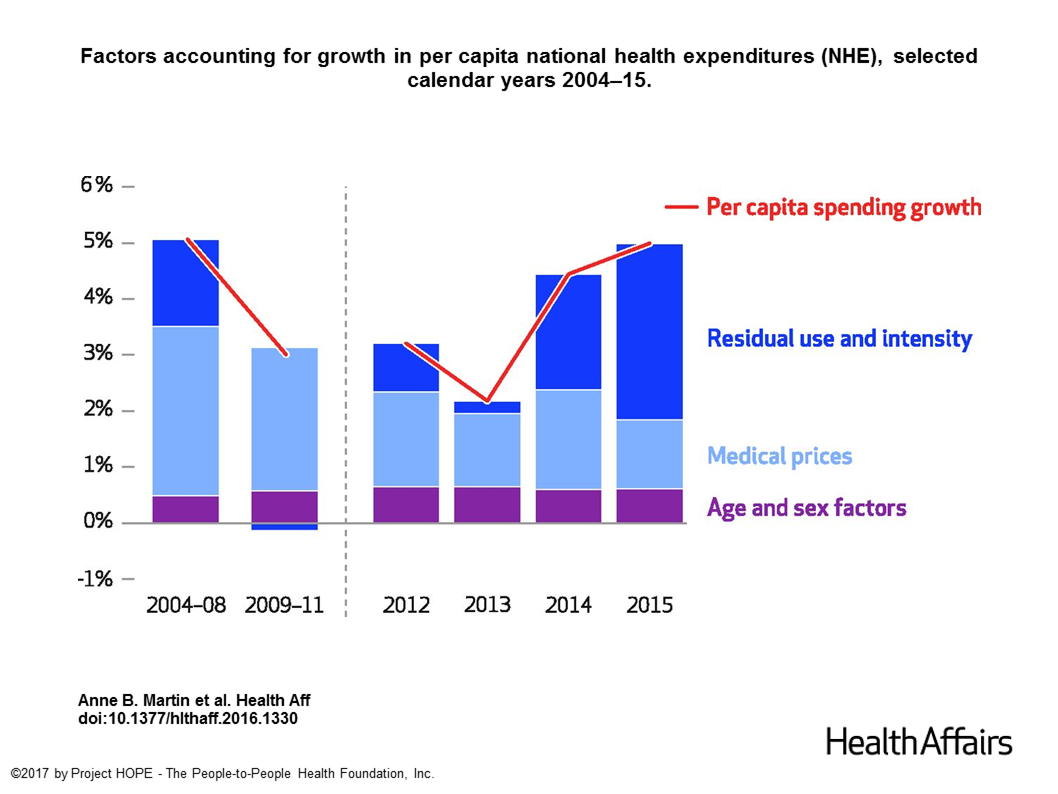
Spending on health care in the U.S. hit $3.2 trillion in 2015, increasing 5.8% from 2014. This works out to $9,990 per person in the U.S., and nearly 18% of the nation’s gross domestic product (GDP). Factors that drove such significant spending growth included increases in private health insurance coverage owing to the Affordable Care Act (ACA) coverage (7.2%), and spending on physician services (7.2%) and hospital care (5.6%). Prescription drug spending grew by 9% between 2014 and 2015 (a topic which I’ll cover in tomorrow’s Health Populi discussing IMS Institute’s latest report into global medicines spending). The topic of
Both Healthcare Prices and Use of Services Driving Up Spending
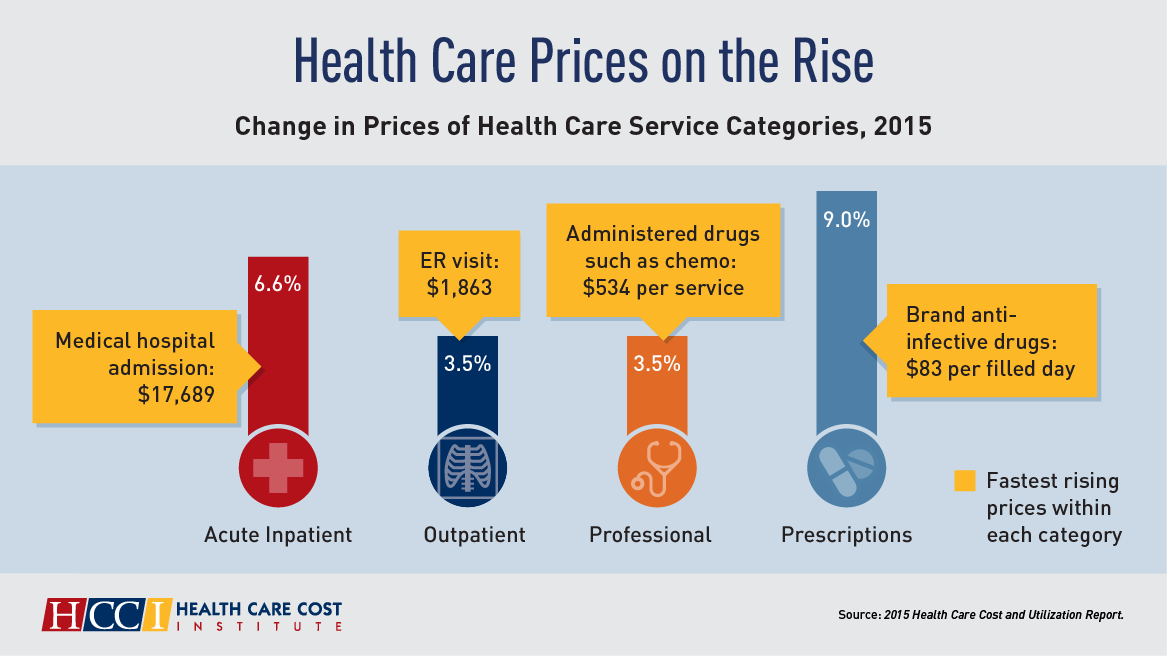
Health care spending grew 4.6% in 2015, higher than the rise in either 2013 or 2014, according to the 2015 Health Care Cost and Utilization Report published by HCCI, the Health Care Cost Institute. The key contributors to health care spending by percentage were, first and foremost, prescription drugs which rose 9% in the year — notably, specialty medicines like anti-infective drugs (such as those for Hepatitis C and HIV) costing on average $83 per “filled day.” This cost doubled from $53 per person in 2012 to $101 per person in 2015. Hospital costs saw the second greatest percentage price increase
The Patient Is The Best Sensor – Consumers At the Center of Health

“The patient is the best sensor,” asserted Jamie Heywood, founder of Patients Like Me, during the perennial meeting sponsored by PwC, the 180° Health Forum. This event featured several panels of PwC’s curated group of so-called “provocateurs” in healthcare, and I was grateful to be one of nine selected for the event. Heywood joined Dr. Leanna Wen, Baltimore City Health Commissioner, and me in a panel called, “Strange Bedfellows or Soul Mates? The New Dating Game in Health.” The theme of our collective brainstorm was how collaborations across the ecosystem could help make health and healthcare better. The drawing is
Hospitals Need to Cross the Health Consumer Chasm
Most U.S. hospitals have not put consumerism into action, a new report from KaufmanHall and Caden’s Consulting asserts from the second paragraph. Patient experience is the highest priority, but has the biggest capability gap for hospitals, the report calls out. KaufmanHall surveyed 1,000 hospital and health system executives in 100 organizations to gauge their perspectives on health consumers and the hospital’s business. KaufmanHall points out several barriers for hospitals working to be consumer-centered: Internal/institutional resistance to change Lack of urgency Competing priorities Skepticism Lack of clarity (vis-a-vis strategic plan) Lack of data and analytics. The key areas identified for consumer centricity
How Value and Consumerism Will Reshape the $5 Trillion Healthcare Market
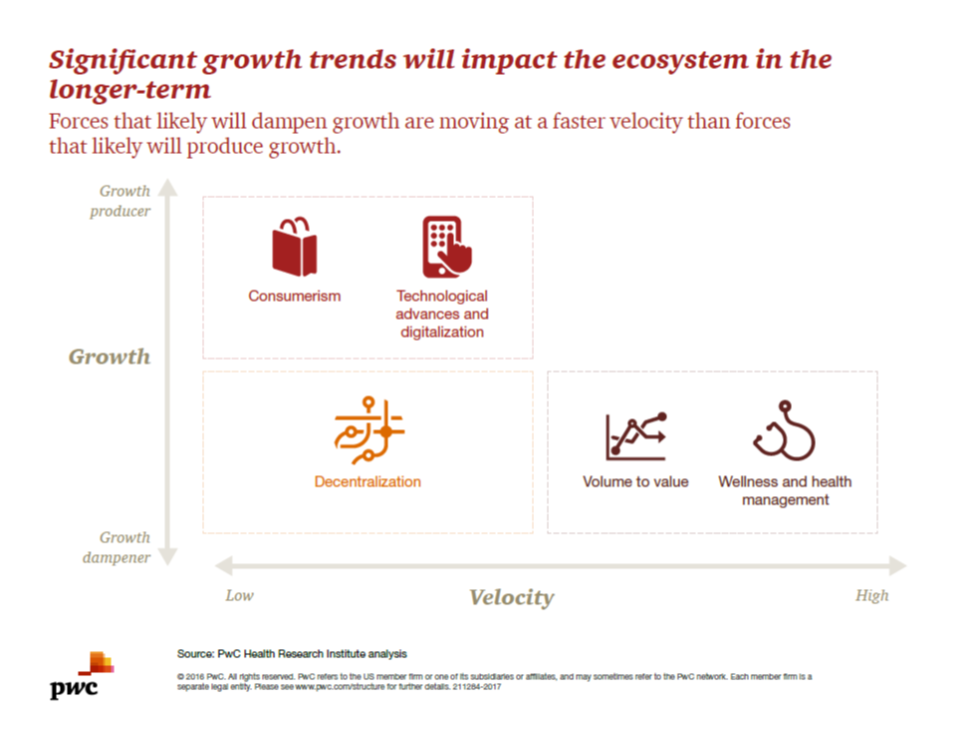
Existing healthcare industry players – the stakeholders of hospitals, physicians, pharma/life sciences, medical device manufacturers, and health plans – are operating in a whirlwind of change. While there are many uncertainties in this period of transition, there’s one operational certainty: learn to do more with less payment. That’s due to the growing pursuit of payors paying for value, not on the basis of volume or what’s “done” to a patient in care delivery. At the same time, another force re-shaping healthcare is interest and focus on wellness and health management. Combined with the growing health economic value proposition, wellness and
Retail Clinics Continue to Shape Local Healthcare Markets
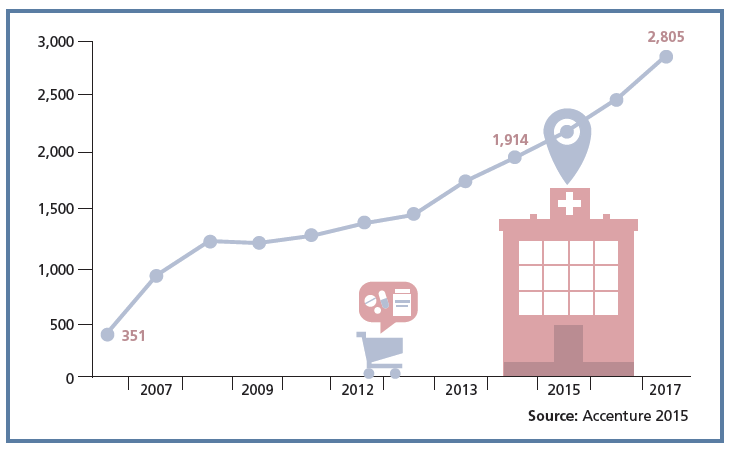
Retail clinics are a growing source of primary care for more U.S. health consumers, discussed in a review of retail clinics published by Drug Store News in July 2016. There will be more than 2,800 retail clinics by 2018, according to Accenture’s tea leaves. Two key drivers will bolster retail clinics’ relevance and quality in local health delivery systems: Retail clinics’ ability to forge relationships with legacy health care providers (physicians, hospitals); and, Clinics’ adoption and effective use of information technology that enables data sharing (e.g., to the healthcare provider’s electronic health records system) and data liquidity (that is, securely moving
U.S. Health Spending Will Comprise 20% of GDP in 2025
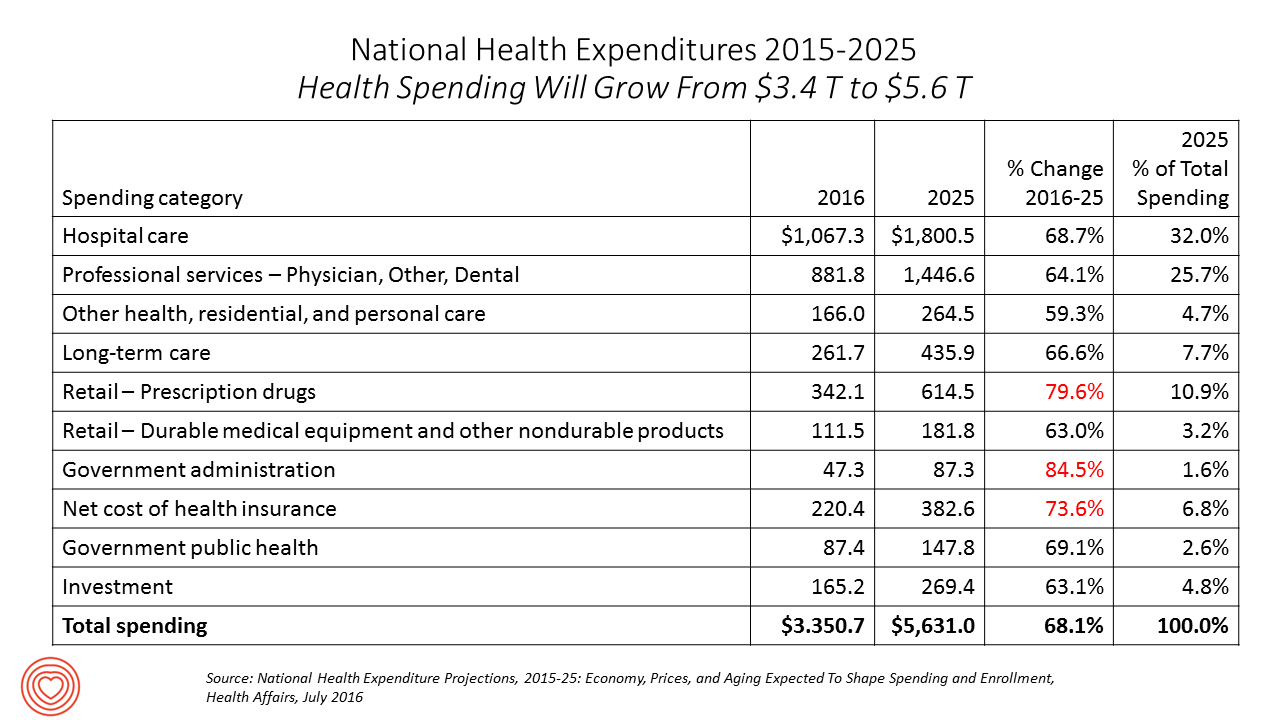
Spending on health care in America will comprise $1 in every $5 of gross domestic product in 2025, according to National Health Expenditure Projections, 2015-25: Economy, Prices, And Aging Expected to Shape Spending and Enrollment, featured in the Health Affairs July 2016 issue. Details on national health spending are shown by line item in the table, excerpted from the article. Health spending will grow by 5.8% per year, on average, between 2015 and 2025, based on the calculations by the actuarial team from the Centers for Medicare and Medicaid Services (CMS), authors of the study. The team noted that the Affordable Care
In Healthcare, Pharmacists and Doctors Most Trusted. Insurance Execs and Congress? Not.
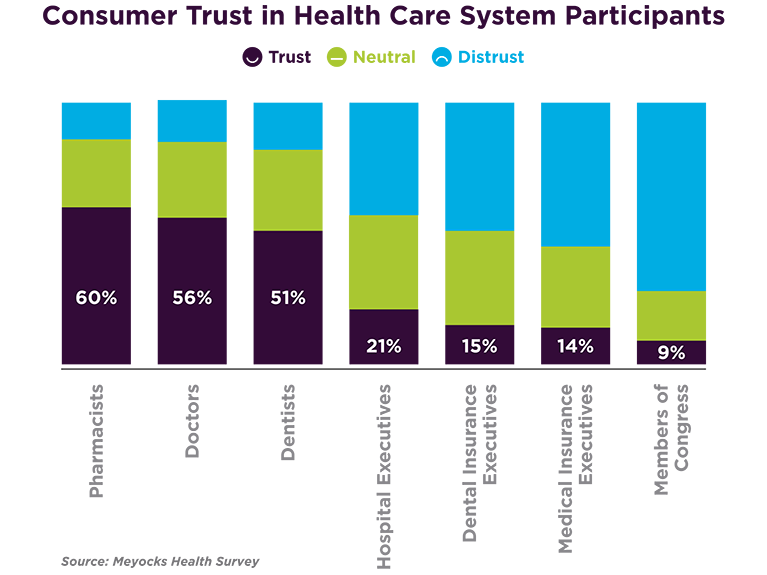
When consumers consider the many stakeholder organizations in healthcare, a majority trust pharmacists first, then doctors and dentists. Hospital and health insurance execs, and members of Congress? Hardly, according to a survey from Meyocks, a marketing consultancy. Meyocks conducted the survey via email among 1,170 US adults, 18 years of age and older. This survey correspondends well with the most recent Gallup Poll on most ethical professions, conducted in December 2015. In that study, pharmacists, nurses and doctors come out on top, with advertisers (“Mad Men”), car salespeople, and members of Congress at the bottom, as shown in the second
Most Wired Hospitals Spending on Cybersecurity, Telehealth and Population Health

Investing information technology dollars in telehealth and mobile platforms, patient engagement, and cybersecurity are major focuses for leading IT-savvy hospitals in America, according to the 2016 Most Wired survey of healthcare organizations, released in July 2016 sponsored by Hospitals and Health Networks and Health Forum, a division of the American Hospitals Association. This survey, in its 18th year, has become an important benchmark measuring the adoption of information technology tools and services among American hospitals and health systems. The complete list of Most Wired hospitals for 2016 can be found here. The most popular telehealth services offered by the Most Wired hospitals are
What Health Care Can Learn from the Blood Clot Community
“Our goal is to create an aware and engaged, irritating set of patients who create a dialogue with health care providers once they’ve had a [blood] clot,” explained Randy Fenninger, CEO of the National Blood Clot Alliance (NBCA). NBCA’s tagline and hashtag is “Stop the Clot.” Welcome to the multi-stakeholder community involved with deep vein thrombosis (DVT) and, clinically speaking, Venous Thromboembolism (VTE). We’re talking blood clots, and the public health burden of this condition is big: it’s a leading cause of death and disability. One in 4 people in the world die of conditions caused by thrombosis. I had
Happy Patients, Healthy Margins – the Hard ROI for Patient-Centered Care
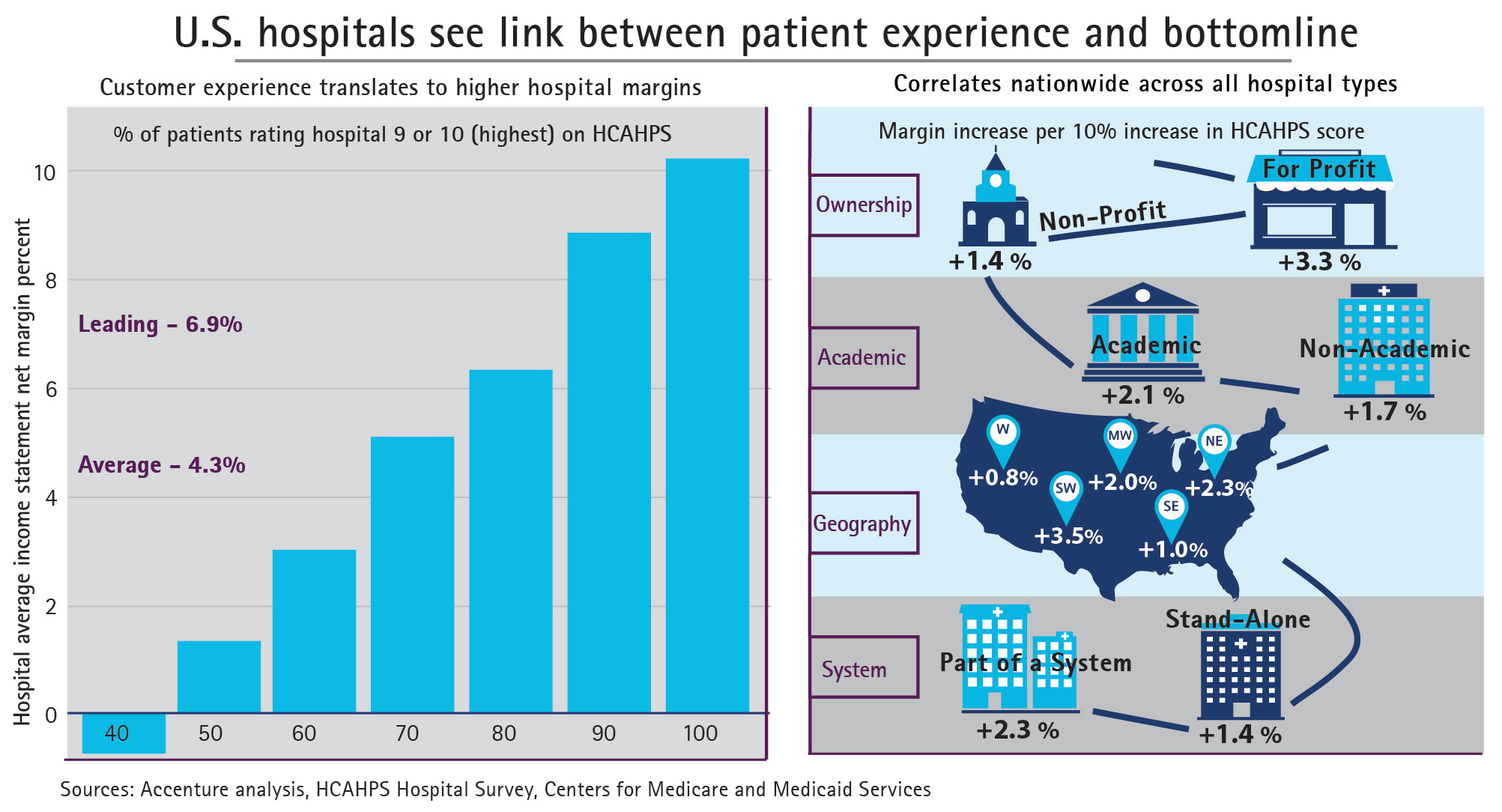
Hospital margins can increase 50% if health providers offer patients a better customer experience, Accenture calculates in the paper, Insight Driven Health – Hospitals see link between patient experience and bottom line. Specifically, hospitals with HCAHPS scores of 9 or 10, the highest recommendations a patient can give in the survey, more likely enjoy higher margins (upwards of 8%). The Hospital Computer Assessment of Healthcare Providers and Systems (HCAHPS) survey is administered by the Centers for Medicare and Medicaid Services (CMS) and measures patients’ exeperiences in hospital post-discharge. The correlation, simply put, is “Happy Patients, Healthy Margins,” Accenture coined in
The Hospital of the Future Won’t Be a Hospital At All
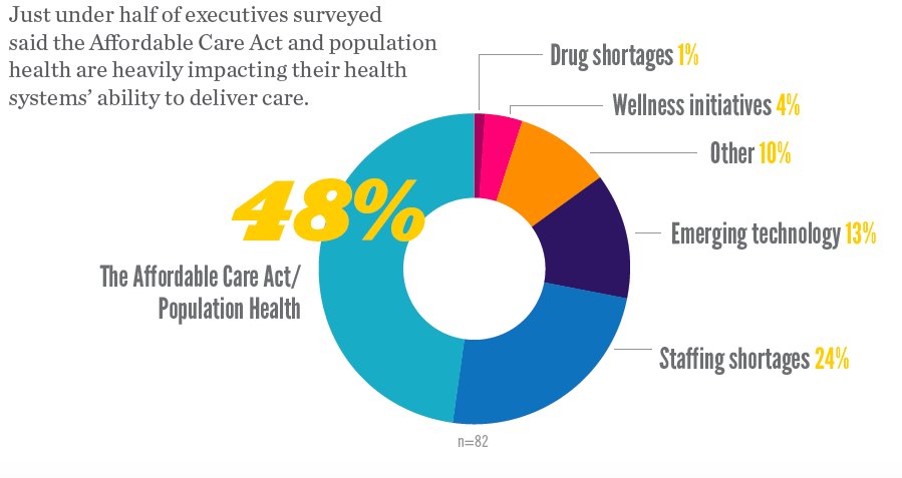
In the future, a hospital won’t be a hospital at all, according to 9 in 10 hospital executives who occupy the c-suite polled in Premier’s Spring 2016 Economic Outlook. Among factors impacting their ability to deliver health care, population health and the ACA were the top concerns among one-half of hospital executives. 1 in 4 hospital CxOs think that staffing shortages have the biggest impact on care delivery, and 13% see emerging tech heavily impacting care delivery. Technology is the top area of capital investment planned over the next 12 months, noted by 84% of hospital execs in the survey.
Telehealth Comes of Age at HIMSS 2016
Telehealth will be in the spotlight at HIMSS 2016, the biggest annual conference on health information technology (HIT) that kicks off on 29th February 2016 in Las Vegas – one of the few convention cities that can handle the anticipated crowd of over 50,000 attendees. Some major pre-HIMSS announcements relate to telehealth: American Well, one of the most mature telehealth vendors, is launching a software development kit (SDK) which will enable The new videoconferencing option can simultaneously connect patients with multiple physicians and specialists, and the SDK is designed to enable users to incorporate telemedicine consults into patient portals and
Rural Hospitals in America – Health Disparities, Hospital Disparities
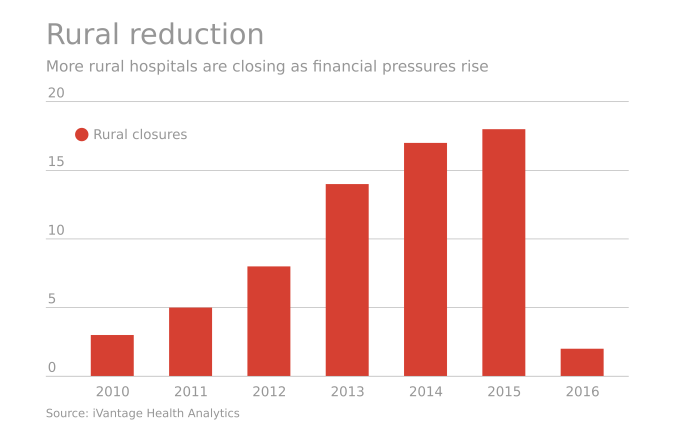
Rural hospitals operating in the U.S. have a higher risk of mortality — closure — than other hospitals in America. The U.S. health care landscape is littered with examples of health disparities among the nation’s health citizens – for example, women’s lower access to heart-health care, Latinos’ higher rates of Type 2 Diabetes, and African-Americans’ greater risks of stroke, many cancers, maternal mortality, and many other causes of mortality and diminished health. A report from iVantage, Rural Relevance – Vulnerability to Value, documents the fiscally challenging environment for rural hospitals in America. There are at least 673 facilities at-risk of closure
Building Health Bridges — Health:Further Goes Beyond the Disruptive

Most people in the U.S. acknowledge that their richest country in the world has a broken healthcare system, especially when it comes to costs. A handful of think tanks and lawmakers offer fixes for American healthcare. Now there’s a new problem-solver in healthcare town, Health:Further, and they aim to move U.S. health forward by building bridges between stakeholders in the U.S. health ecosystem. My longtime colleague and friend, Andre Blackman of Pulse+Signal, has joined the organization as “Producer.” Here, we’ll learn more from my (JSK) interview with Andre (AB) about the organization, their mission, and plans to go beyond “disruption”
Diagnosis: Acute Health Care Angst In America
There’s an overall feeling of angst about healthcare in America among both health care consumers and the people who provide care — physicians and administrators. On one thing most healthcare consumers and providers (can agree: that the U.S. health care system is on the wrong track. Another area of commonality between consumers and providers regards privacy and security of health information: while healthcare providers will continue to increase investments in digital health tools and electronic health records systems, both providers and consumers are concerned about the security of personal health information. In How We View Healthcare in America: Consumer and Provider Perspectives,
U.S. Health At A Glance – Not So Healthy
People in the U.S. have lower life expectancy, a growing alcohol drinking problem, and relatively high hospital inpatient rates for chronic conditions compared with other OECD countries. And, the U.S. spends more on health care as a percent of GDP than any other country in the world. This isn’t new-news, but it confirms that U.S. health citizens aren’t getting a decent ROI on health spending compared with health citizens around the developed world. In the OECD’s latest global look at member countries’ health care performance, Health at a Glance 2015, released today, the U.S. comes out not-so-healthy in the context
Physical Healthcare Facilities Can Bolster Health Consumerism
Reluctantly accepting the Affordable Care Act, health executives and their architects now see opportunities for re-imagining the hospital and health care services, according to Healthcare Industry Trends, a publication that’s part of the 2015 Building & Development Leadership Series provided by Mortenson, a construction services firm that’s active with healthcare organizations. Mortenson conducted a survey at the 2015 ASHE Planning, Design, and Construction Summit, the results of which were published in this report. The over 300 respondents included healthcare executives, facilities managers, and healthcare architects. Thus the lens on the data in this survey is through the eyes of physical
Virtual Visits Would Conserve Primary Care Resources in US Healthcare
By shifting primary care visits by 5 minutes, moving some administrative tasks and self-care duties to patients, the U.S. could conserve billions of dollars which could extend primary care to underserved people and regions, hire more PCPs, and drive quality and patient satisfaction. Accenture’s report, Virtual Health: The Untapped Opportunity to Get the Most out of Healthcare, highlights the $10 bn opportunity which translates into conserving thousands of primary care providers. PCPs are in short supply, so virtual care represents a way to conserve precious primary care resources and re-deploy them to their highest-and-best-use. The analysis looks at three scenarios
Palliative Care: Getting End of Life Care (W)right
I lost a best friend last week. His memorial service, held this past weekend, was a celebration of his life. And part of that well-lived life was a very conscious planning of his last days. The Economist published its 2015 Quality of Death Index, a data-driven treatise on palliative care, the very week my dear friend Rick died. This gives me the opportunity to discuss palliative care issues with Health Populi readers through The Economist’s lens, and then in the Hot Points below through my personal context of this remarkable man’s end-of-life choices. The Economist ranks 80 countries on several
The Tricky Journey From Volume To Value In Health Care – Prelude To Health 2.0
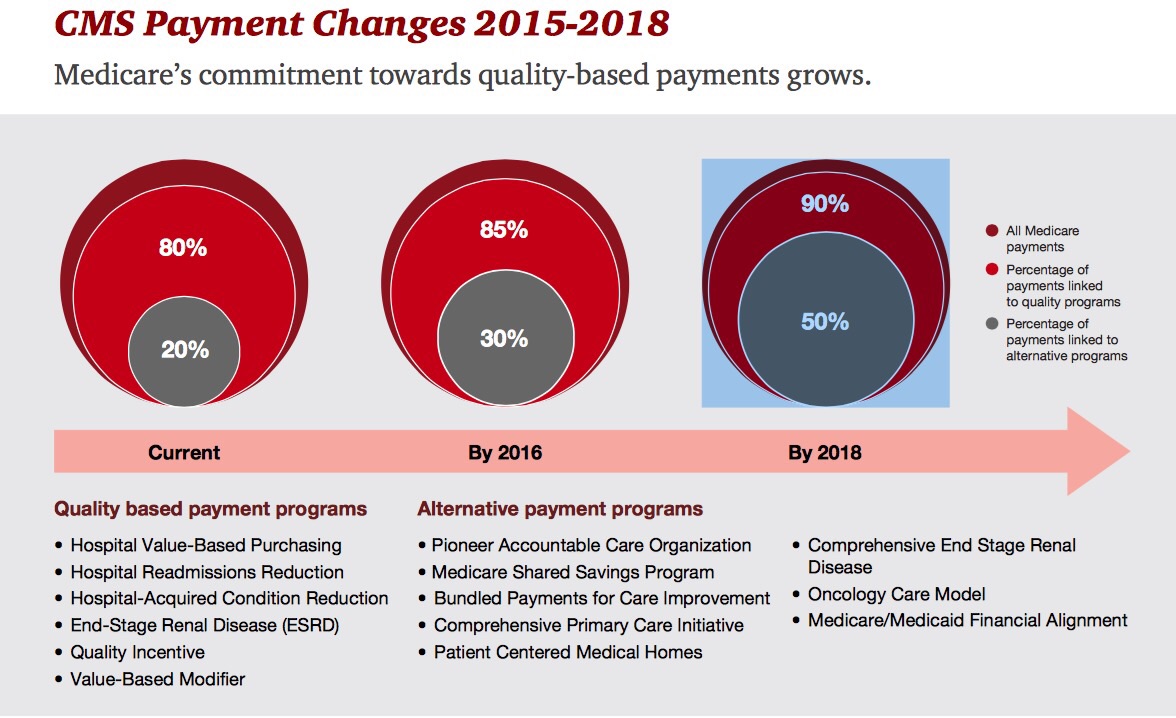
By 2018, 90% of health care delivered to people enrolled in Medicare will be paid-for on the basis of quality, not on the amount of services delivered (that is, volume). But as providers must up their game in that new value-oriented health payment world, they are bound up in work flows and organizational structures built for fee-for-service reimbursement. This changing future is discussed in Healthcare’s alternative payment landscape, PwC’s Healthcare Research Institute report on the volume-to-value shift. PwC notes that health care providers’ ability to adapt to changing payment regimes vary and fall into four categories: traditional, lagging, vanguard and





 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.