Strengthening Chronic Care Is Both Personal and Financial for the Patient
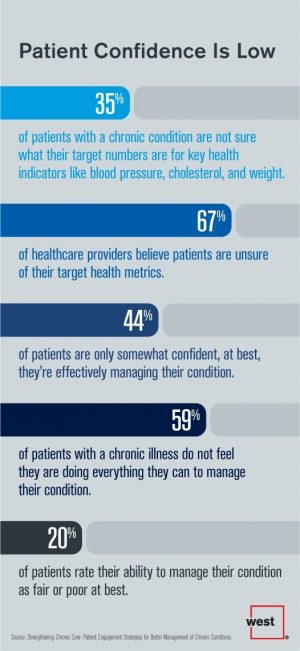
6 in 10 people diagnosed with a chronic condition do not feel they’re doing everything they can to manage their condition. At the same time, 67% of healthcare providers believe patients aren’t certain about their target health metrics. Three-quarters of physicians are only somewhat confident their patients are truly informed about their present state of health. Most people and their doctors are on the same page recognizing that patients lack confidence in managing their condition, but how to remedy this recognized challenge? The survey and report, Strengthening Chronic Care, offers some practical advice. This research was conducted by West
The Pursuit of Health Equity and the State of U.S. Health Care
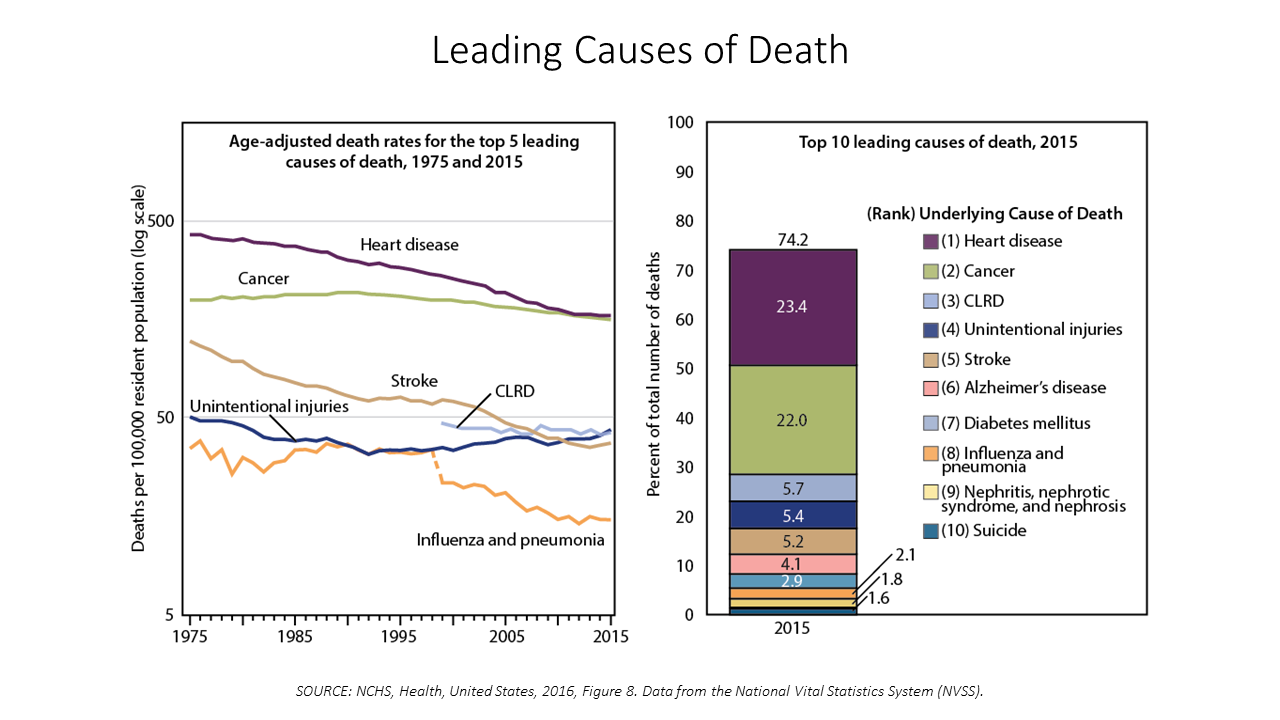
Between 2014 and 2015, death rates increased for eight of the ten leading causes; only death rates caused by cancer fell, and mortality rates for influenza and pneumonia stayed flat. The first chart paints this sobering portrait of Americans’ health outcomes, presented in the CDC’s data-rich 488-page primer, Health, United States, 2016. Think of this publication as America’s annual report on health. Every year, it is prepared and submitted to the President and Congress by the Secretary of the Department of Health and Human Services. This year’s report was delivered by DHHS Secretary Tom Price to President Trump and the
12% of Americans Have At Least 5 Chronic Conditions and Spend 41% of Healthcare Dollars
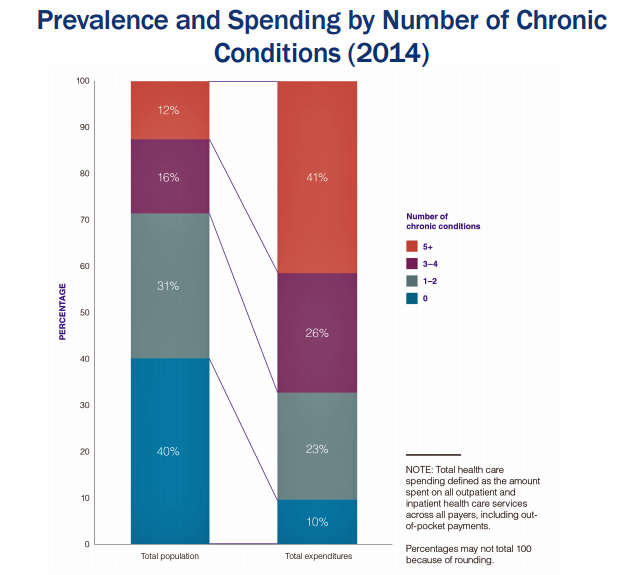
Forget about the 80/20 Rule. Welcome to the 41/12 Metric: 12% of U.S. adults account for 41% of healthcare spending in America, calculated by RAND Corporation in their new report, Multiple Chronic Conditions in the United States. RAND’s report quantifies the growing chronic care landscape in America that will be a burdensome legacy for younger Americans in terms of financial and social costs. First, a definition: RAND defines a chronic condition as a physical or mental health issue that lasts more than one year and causes functional restrictions or requires ongoing monitoring or treatment. Older adults are more likely to
The Mental Health Risks of Social Media for Young People

As addictions go, social media can be more addictive than cigarettes or alcohol, according to a report from the Royal Society for Public Health (RSPH), #StatusOfMind, on social media and young people’s mental health and wellbeing. With 91% of people age 16-24 using the internet for social networking, that addiction connects to rising levels of anxiety and depression, the Royal Society asserts, recommending some calls to action to address this public health problem head-on. While this report focuses on the population in the United Kingdom (UK), the social media trends are at least as prominent in the US. The calls
The Power of Joy in Health and Medicine – Learning From Dr. Regina Benjamin

Former Surgeon General Dr. Regina Benjamin was the first person who quoted to me, “Health isn’t in the doctor’s office. It’s where people live, work, play and pray,” imparting that transformational mantra to me in her 2011 interview with the Los Angeles Times. I wrote about that lightbulb moment here in Health Populi. Dr. Benjamin was the 18th Surgeon General, appointed by President Obama in 2009. As “America’s Doctor,” she served a four-year term, her mission focused on health disparities, prevention, rual health, and children’s health. Today, Dr. Benjamin wears many hats: she’s the Times Picayune/NOLA.com professor of medicine at
Learning Health Behavior Change From the Guru Prochaska
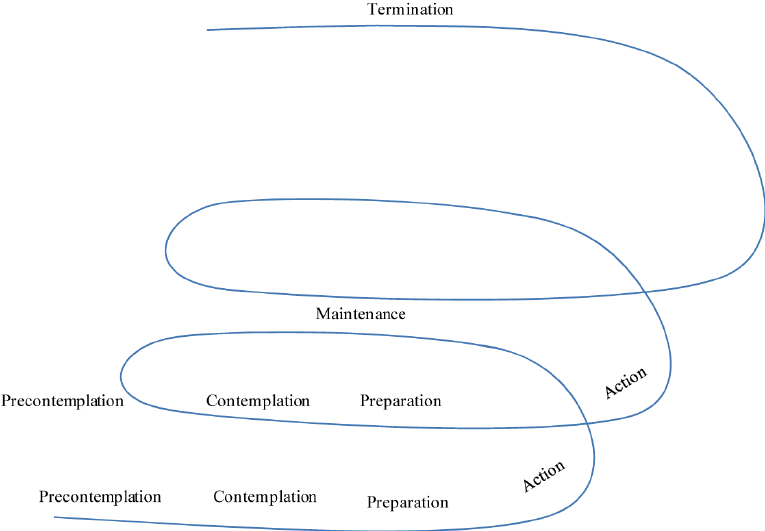
For us mere humans, behavior change is hard. Changing health behaviors is really tough. Enter Dr. James Prochaska, who has been at the forefront of researching and understanding human and health behavior for several decades. He’s the father of the Transtheoretical Model of Behavior Change (TTM). I have the honor today to listen live to Dr. Prochaska’s talk at the Health Integrated EMPOWER conference in St. Petersburg, Florida, where I’ll be addressing attendees on the new health consumer tomorrow. “Empower,” indeed. Dr. Prochaska is all about how people have good intentions to make good health decisions, but we all slip and
Telehealth and Virtual Healthcare Are Mainstreaming
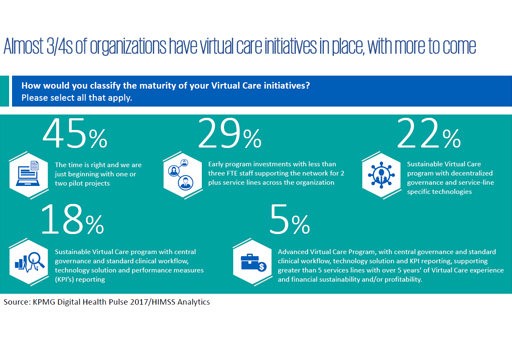
As the annual meeting of the American Telemedicine Association convenes this week in Orlando, there’s a lot of telehealth news to curate. The topline of it all: virtual healthcare is mainstreaming, with more providers, payors, and patients aligning in support of virtual health care delivery. Three-quarters of providers have some form of basic telemedicine or telehealth in place. One-third of healthcare providers use some flavor of virtual care technology in their workflow, according to research from KPMG and HIMSS Analytics summarized in the first graphic. KPMG sees virtual care options — remote patient monitoring, enhanced portals, and web interactions for patient-provider
Diet, Surgery and Pharmacy – The Pillars of Healthcare for 500 Years
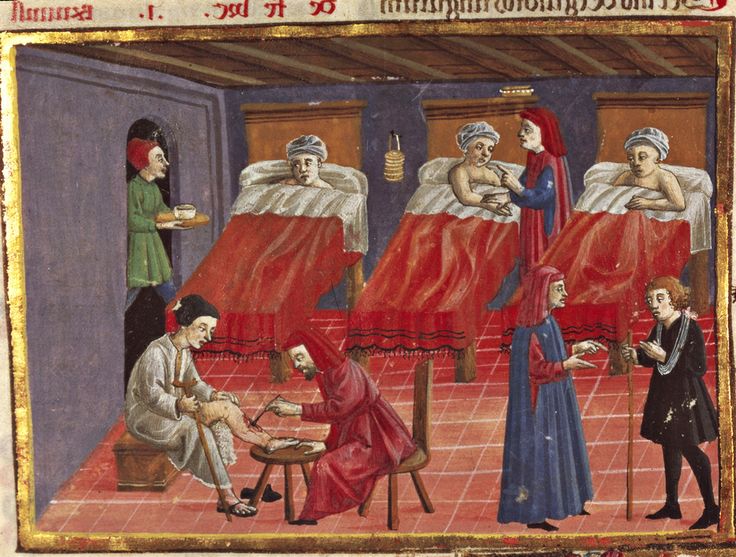
Healthcare was based on three pillars in 16th century Florence, Italy: diet, surgery, and pharmacy. Five centuries later, not much has changed in Italy or the U.S. But how healthcare gets funded and delivered in the context of these pillars significantly varies between the two countries, and impacts each nation’s health. To put this in context, visiting the Biblioteca Medicea Laurenziana (the Medici’s Laurentian Library) today in Florence was a trip through medical-surgical history, starting in the second half of the 16th century. The design of this magnificent library’s foyer and reading room was initially conceived by Michelangelo. The reading room
A New Risk Factor For Mental Health: Climate Change
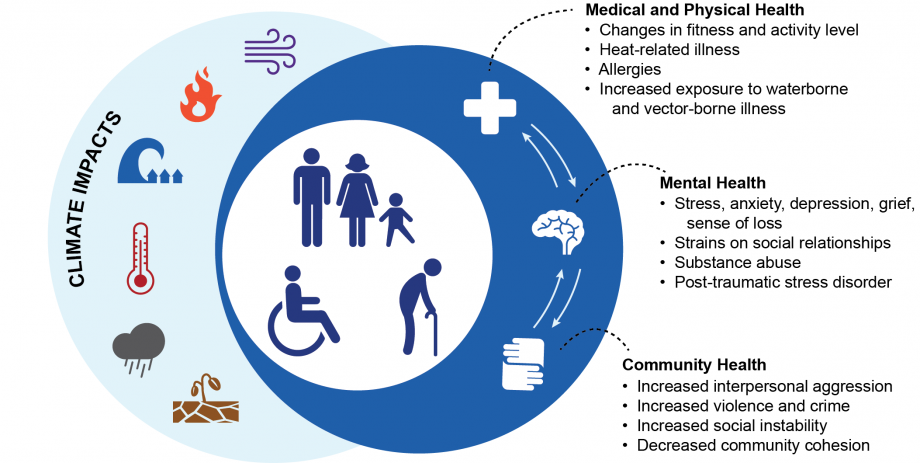
We make our health across many dimensions: via nutrition, safe physical/built environments, financial wellness, education, and the environment among them. In this last category, the environment, new research finds that climate change has a significant impact on health. The report, Mental Health and Our Changing Climate: Impacts, Implications, and Guidance, was sponsored by the American Psychological Association in conjunction with Climate for Health and ecoAmerica. “Climate change-induced severe weather and other natural disasters have the most immediate effects on mental health in the form of the trauma and shock due to personal injuries, loss of a loved one, damage to
You Are The Expert of Your Own Health: adidas and The Future of Fit

The future of wellness combines: Connected (you) Social IRL (in-real-life) Banishing bad (de-tabooing what’s traditionally seen as “bad”) Humanizing data, and The end of experts. These insights come from adidas, whose team developed a forecast of the future of fit, announced at the 2017 South-by-Southwest Festival in Austin this weekend. I had the honor of participating in this forecast and shepherding the SXSW panel on The End of Experts: Crowdsourcing Your Wellness at the adidas meet-up held over the weekend. The future of fit and wellness is Connected, because we are growing to understand that balancing many elements in our daily
Patients Grow Comfortable With Digital Health Tools, CDW Finds
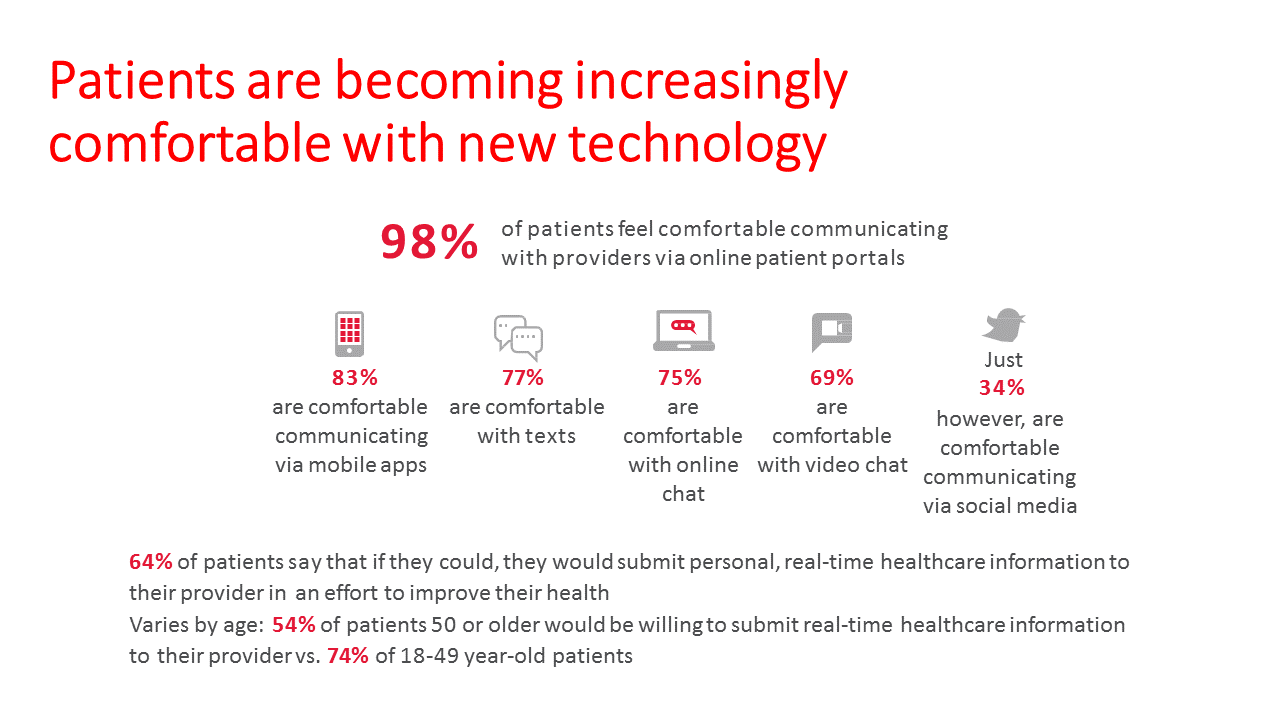
It’s generally thought that healthy people are more health-engaged than people diagnosed with medical issues. But that’s old health school thinking: most health consumers managing chronic conditions say they’ve become more engaged with healthcare over the past two years, according to CDW’s 2017 Patient Engagement Perspectives Study. In 2017, 70% of patients told CDW they’d become more engaged with healthcare, up from 57% in 2016. That’s a 20% growth in the proportion of patients engaging in healthare in just one year. Growing signs of patient engagement are in people driven to access online patient portals for their personal healthcare records: People
What’s the Future Of Fit? Join adidas At #SXSW17

The truest form of health reform and consumer-directed health care isn’t in a high-deductible health plan or a health savings account, and it doesn’t come out of Washington DC or your employer’s health benefits office. It comes from you in the form of self-care and DIY healthcare. In this case, think “inspired by sport, powered by you.” I’ll be participating on a panel at this weekend’s South-by-Southwest Festival in Austin, Texas, along with three wellness innovators: Nick Buettner of the Blue Zones project, Mary Liz McCurdy of Google, and John Wilbanks from Sage Bionetworks. Together, our quartet will brainstorm the
Your Zip Code Is Your Wellness Address

Geography is destiny, Napoleon is thought to have first said. More recently, the brilliant physician Dr. Abraham Verghese has spoken about “geography as destiny” in his speeches, such as “Two Souls Intertwined,” The Tanner Lecture he delivered at the University of Utah in 2012. Geography is destiny for all of us when it comes to our health and well-being, once again proven by Gallup-Healthways in The State of American Well-Being 2016 Community Well-Being Rankings. The darkest blue circles in the U.S. map indicate the metro areas in the highest-quintile of well-being. The index of well-being is based on five metrics, of consumer self-ranking
Stress Is A Social Determinant of Health – Money and Politics Top the List in 2017

The American Psychological Association reports that Americans are experiencing greater levels of stress in 2017 for the first time since initiating the Stress in America Survey ten years ago in 2007. This is a statistically significant finding, APA calculated. The member psychologists of the American Psychological Association (APA) began to report that patients were coming to appointments increasingly anxious about the 2016 Presidential election. So the APA polled U.S. adults on politics for the first time in ten years of conducting the Stress in America survey. Two-thirds of Americans are stressed and/or anxious about the future of the nation, and
How Amazon Has Primed Healthcare Consumers

We are all Amazon Prime primed as consumers now. So it should not surprise healthcare providers, plans and suppliers that consumers expect just-in-time convenience for their healthcare, Accenture has found. Mind the gap: 8 in 10 U.S. patients would welcome some aspect of virtual healthcare, but only 1 in 5 providers is meeting that need. The consumer demand for virtual care is palpable for: Tracking biometrics, among 77% of consumers (say, for measuring blood pressure or blood glucose for people managing diabetes) Following up appointments, for 76% of people after seeing a doctor or being discharged from hospital Receiving reminders
Consumers Taking Healthcare Into Own Hands at CES 2017

Consumer electronics (CE) aren’t just big screen TVs, sexy cars, and videogames anymore. Among the fastest-growing segments in CE is digital health, and health-tech will be prominently featured at the 2017 CES in Las Vegas hours after the champagne corks have popped at the start of the new year. On the second day of 2017, I’ll be flying to Las Vegas for several days of consumer technology immersion, learning about connected and smart homes and cars, and shiny new things all devoted to personal health. Welcome to my all-health lens on CES 2017, once referred to as the Consumer Electronics
Retail Trumps Healthcare in 2017: the Health Populi Forecast for the New Year

Health citizens in America will need to be even more mindful, critical, and engaged healthcare consumers in 2017 based on several factors shaping the market; among these driving forces, the election of Donald Trump for U.S. president, the uncertain future of the Affordable Care Act and health insurance, emerging technologies, and peoples’ growing demand for convenience and self-service in daily life. The patient is increasingly the payor in healthcare. Bearing more first-dollar costs through high-deductible health plans and growing out-of-pocket spending for prescription drugs and other patient-facing goods and services, we’re seeking greater transparency regarding availability, cost and quality of
1 in 3 Americans Still Self-Rations Healthcare
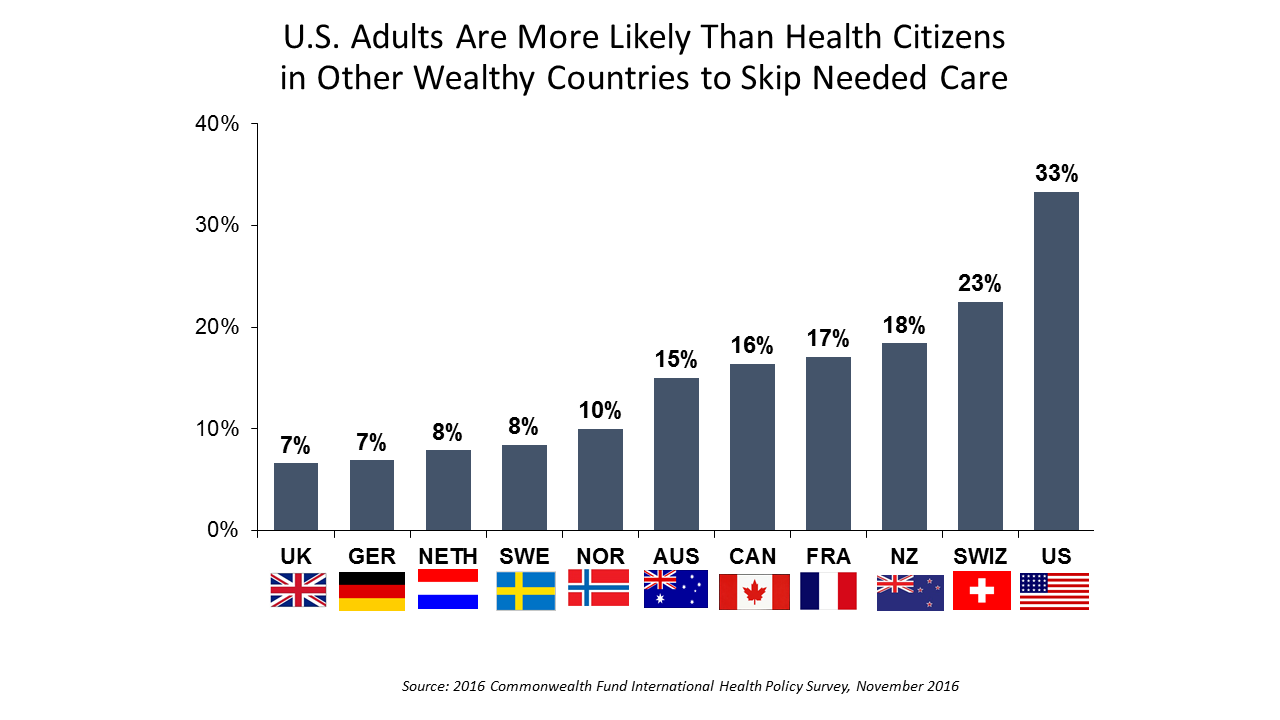
People in the U.S. are much more likely to go without health care they need compared with health citizens in 10 other wealthy countries, according to the Commonwealth Fund’s 2016 international survey. One-third of Americans did not seek care due to costs, including going without recommended care, failing to fill a prescription drug, and/or not seeing a doctor when sick. While this self-rationing proportion of Americans dropped from 37% in 2013, the U.S. still ranks #1 in foregoing necessary healthcare due to cost. “In comparison to adults in the other 10 countries, adult sin the U.S. are sicker and more
Stress and Health During #Election2016
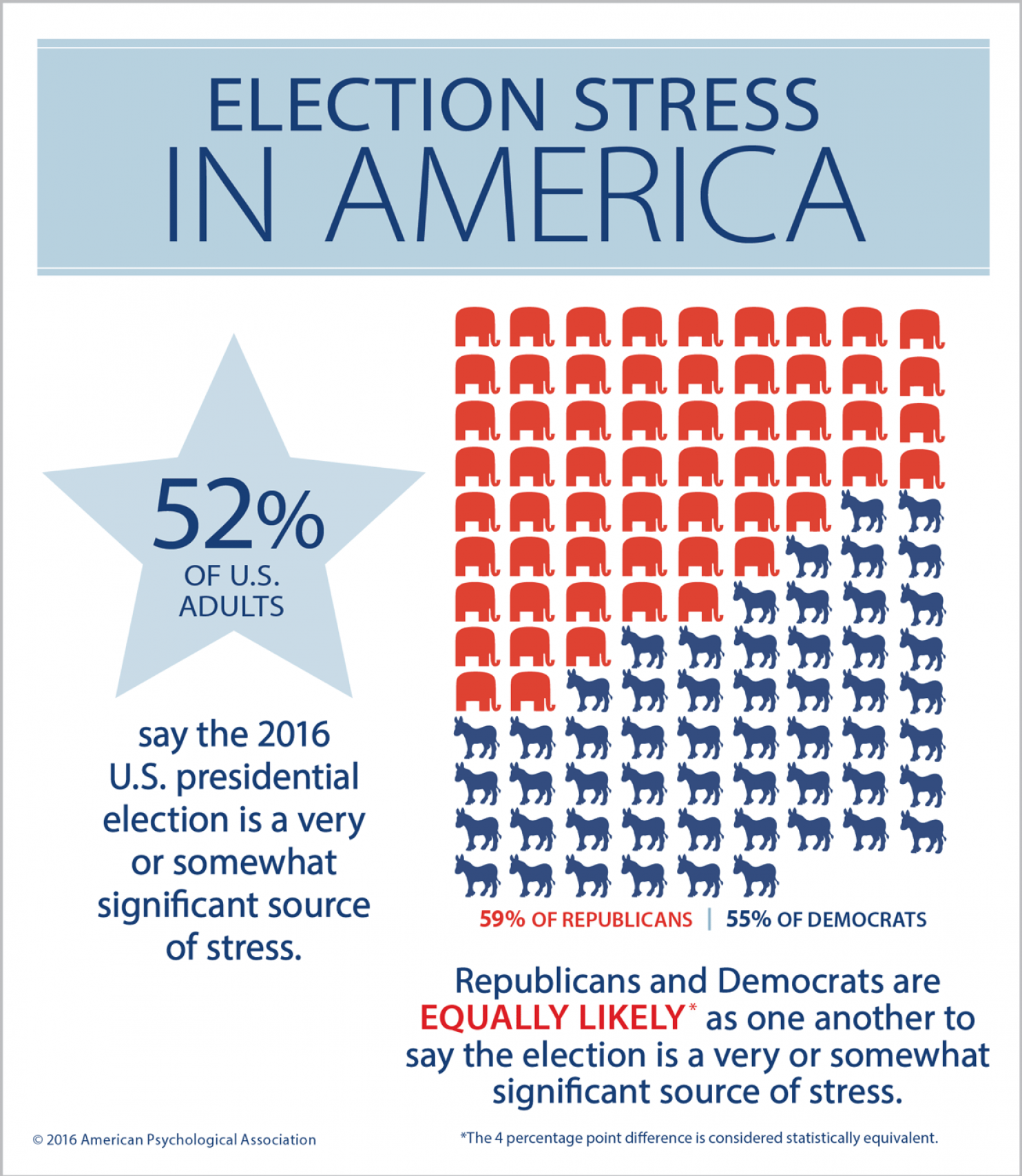
The American Psychological Association, which conducts the annual Stress in America survey, has found rising levels of stress during #Election2016. 1 in 2 U.S. adults says the U.S. presidential election is a source of stress, with Democrats and Republicans equally likely to feel this way. So the APA is offering tips on how we can deal with the health impacts of election season stress. These include: Take a digital break and limiting your media consumption, reading or listening to “just enough to stay informed.” Instead, go for a walk and do things you enjoy. Avoid getting into and limit discussions about the
Building the Primary Care Dream Team
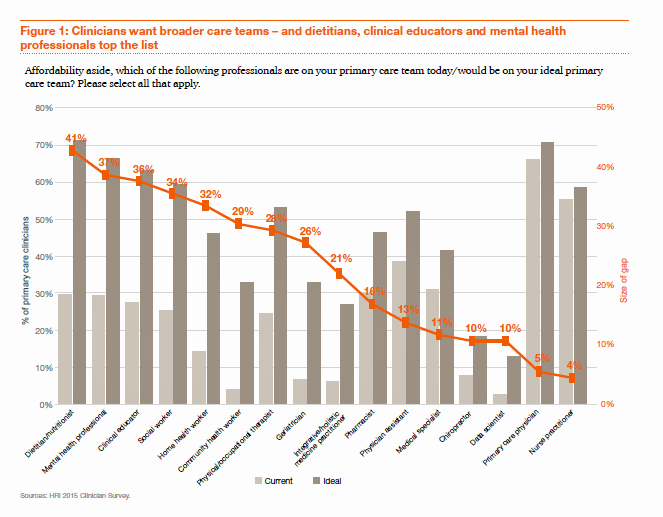
“Today’s primary care won’t work tomorrow,” given the shortage of primary care providers (PCPs) and the need to do more in healthcare with fewer resources in the emerging value-based economy. So let’s re-imagine primary care models, PwC asserts, and makes the case in their report, ROI for primary care: Building the dream team. What’s the financial impact of this dream team on healthcare providers? It’s potentially $1.2 million in savings for every 10,000 patients served, PwC calculates. Historically, physicians have been loath to share their work with non-physicians because of how doctors have been paid — on the basis of fee-for-service,
Most Digital Health Consumers Say They Benefit from Connected Health
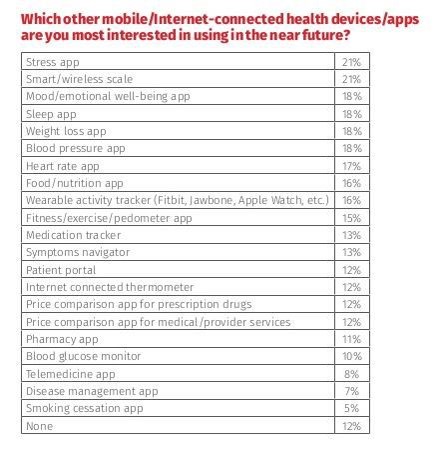
Managing stress, weight, mental health, sleep, and heart function are among the top-most desired reasons already-connected health consumers are interested in further connecting their health, according to The 2016 HealthMine Digital Health Report. The most popular tools people use to digitally manage their health deal with fitness and exercise (among 50% of connected health consumers), food and nutrition (for 46%), and weight loss (for 39%). 3 in 4 people who use digital health tools say they have improved their health by connecting to these tools. 57% of digital health users also say going health-digital has lowered their healthcare costs. The survey
Medical Tourism On A Cruise Ship

Health is everywhere: where we live, work, play, and learn, as I’ve often written here on Health Populi. While I’ve also analyzed the market for medical tourism over the past twenty years, this week I’ve learned that it extends to the cruise travel industry along with hospitals and clinics around the world. I had the pleasure of meeting up this week with Hannah Jean Taylor, Manager of the Mandara Spa on Norwegian Cruise Line‘s ship, The Norwegian Breakaway. This vessel accommodates nearly 4,000 passengers who enjoy the services of over 1,600 staff members in the hotel, entertainment, and operational crews.
Employers Changing Health Care Delivery – Health Reform At Work
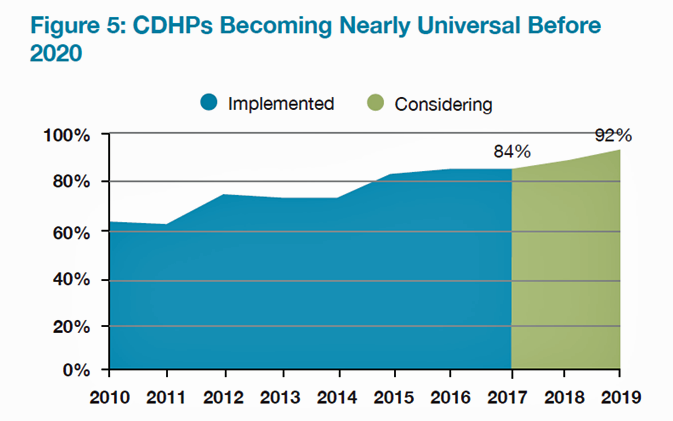
Large employers are taking more control over health care costs and quality by pressuring changes to how care is actually delivered, based on the results from the 2017 Health Plan Design Survey sponsored by the National Business Group on Health (NBGH). Health care cost increases will average 5% in 2017 based on planned design changes, according to the top-line of the study. The major cost drivers, illustrated in the wordle, will be specialty pharmacy (discussed in yesterday’s Health Populi), high cost patient claims, specific conditions (such as musculoskeletal/back pain), medical inflation, and inpatient care. To temper these medical trend increases,
The Drug Epidemic-Testing and Data Arm the Battle
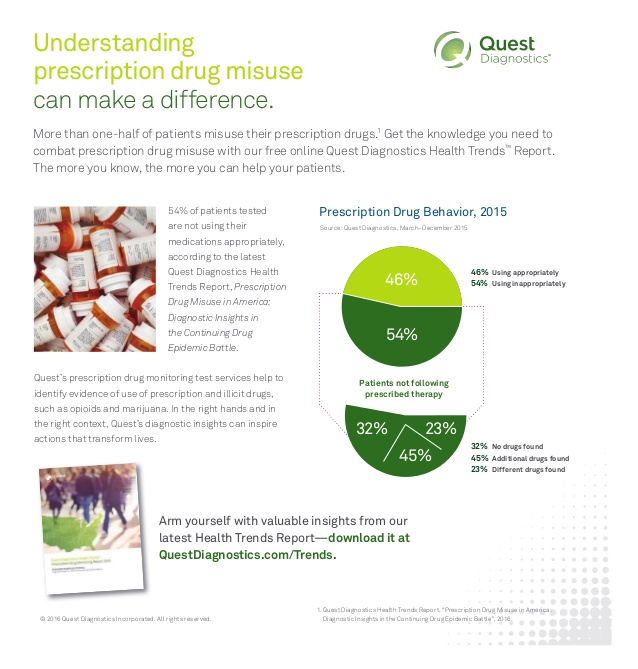
More than 40 Americans die every day from prescribed opiate overdoses, Dr. Tom Frieden of the CDC has recognized. The harms of pain-killing drugs have been substantial: Dr. Frieden observed, “the prevalence of opioid dependence may be as high as 26% among patients in primary care receiving opioids for chronic non-cancer-related pain.” There were more deaths due to drug overdoses in 2014 than in any previous year, 61% of which involved opioid pain relieving medications such as oxycodone and hydrocodine, and heroin which has grown in use over the past few years. The CDC has recommended that healthcare providers do
Health in America: Improving, But Disparities Need Policy Prescriptions
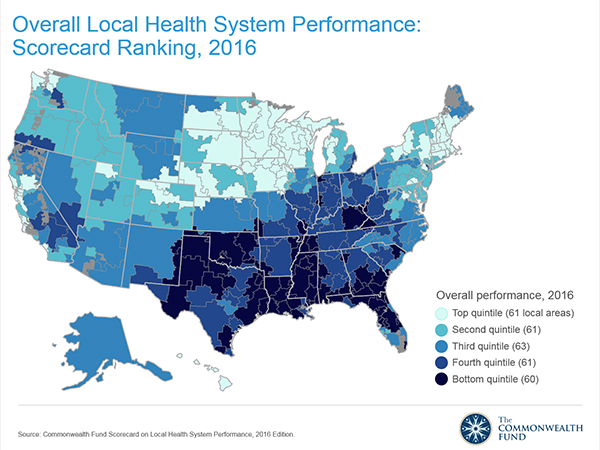
The bad news: mortality rates haven’t improved much and obesity rates rose in one-third of communities. The good news: public health gains can be made in resource-poor communities with the right health policies, based on research from The Commonwealth Fund, Rising to the Challenge, the Fund’s Scorecard on local health system performance for 2016. The top-line of this benchmark report is that health care in the U.S. has, overall, improved more than it’s declined. Among the big levers driving health care improvement in the past year have been the further expansion of health citizens covered with insurance through the Affordable
More Patients Morph Into Financially Burdened Health Consumers
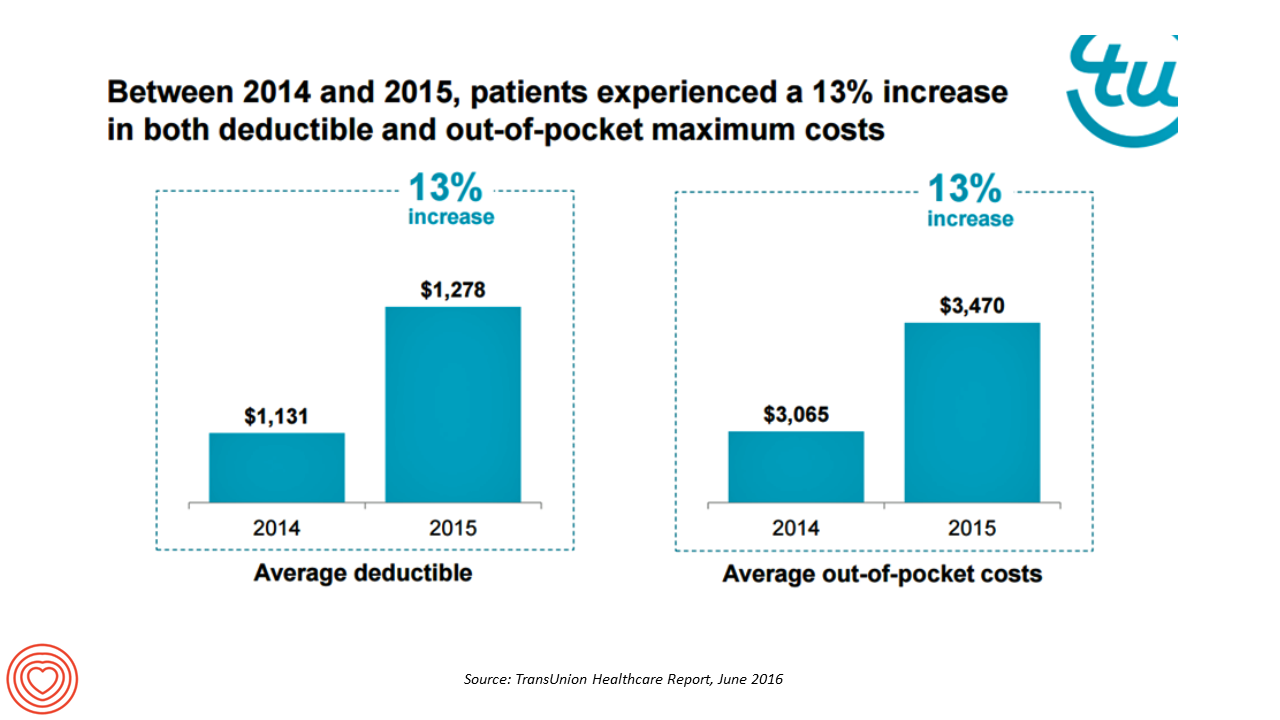
Health care payment responsibility continues to shift from employers to employee-patients, More of those patients are morphing into financially burdened health consumers, according to TransUnion, the credit agency and financial risk information company, in the TransUnion Healthcare Report published in June 2016. Patients saw a 13% increase in their health insurance deductible and out-of-pocket (OOP) maximum costs between 2014 and 2015. At the same time, the average base salary in the U.S. grew 3% in 2015, SHRM estimated. Thus, deductibles and OOP costs grew for consumers more than 4 times faster than the average base salary from 2014 to 2015. In
Workplace Wellness Goes Holistic, Virgin Pulse Finds
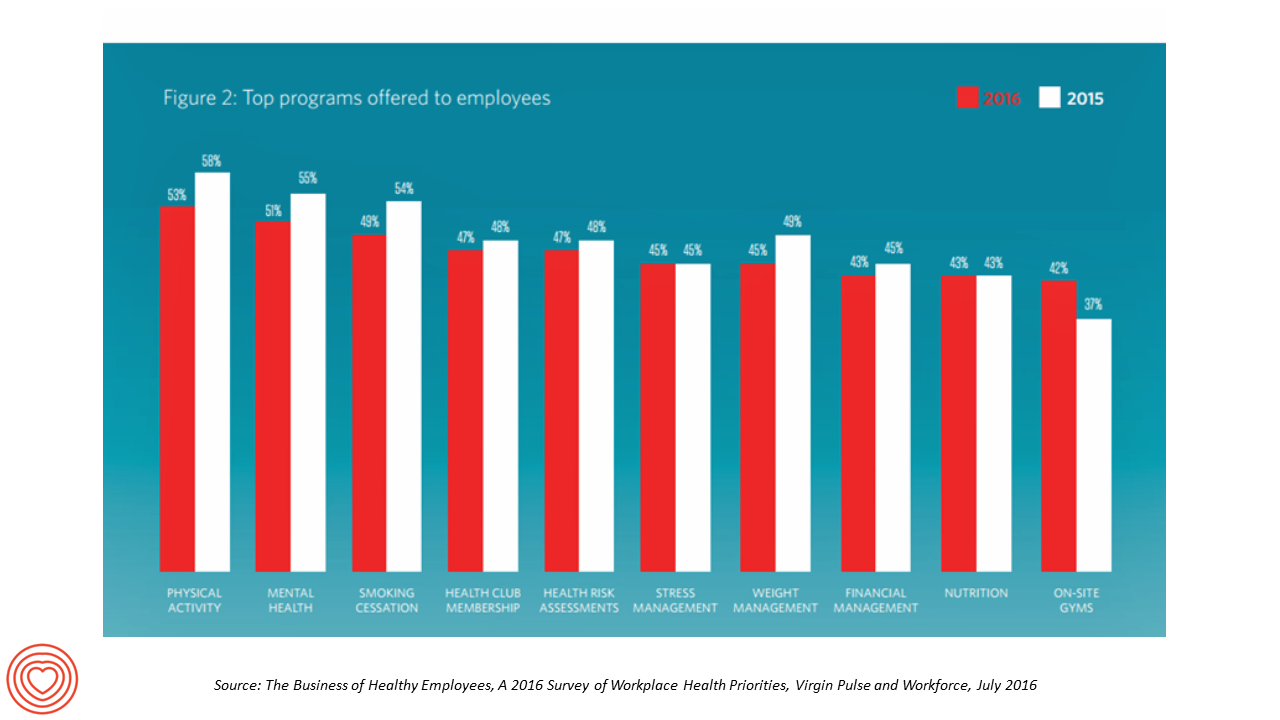
“Work is the second most common source of stress, just behind financial worries,” introduces The Business of Healthy Employees report from Virgin Pulse, the company’s 2016 survey of workplace health priorities published this week. Virgin Pulse collaborated with Workforce magazine, polling 908 employers and 1,818 employees about employer-sponsored health care, workers’ health habits, and wellness benefit trends. Workplace wellness programs are becoming more holistic, integrating a traditional physical wellness focus with mental, social, emotional and financial dimensions for 3 in 4 employers. Wearable technology is playing a growing role in the benefit package and companies’ cultures of health, as well
The Health Disparities of Being Gay
#PrayForOrlando The club Pulse, site of the biggest mass gun shooting in U.S. history, was named to honor one of the co-owner’s brothers, who succumbed to AIDS in 1991. In today’s Health Populi, I soberly ponder the lost lives in the Orlando massacre of people who joyfully convened in a safe haven to celebrate life, liberty, and their pursuits of happiness. Over fifty people ended up dead, and there will be more mortalities as the health workers at Orlando Regional Medical Center continue to fight the post-trauma battle to save gunned-down lives. We define “health” broadly in Health Populi and
Are We Health Engaged Yet? Frost & Sullivan Responds “Meh”
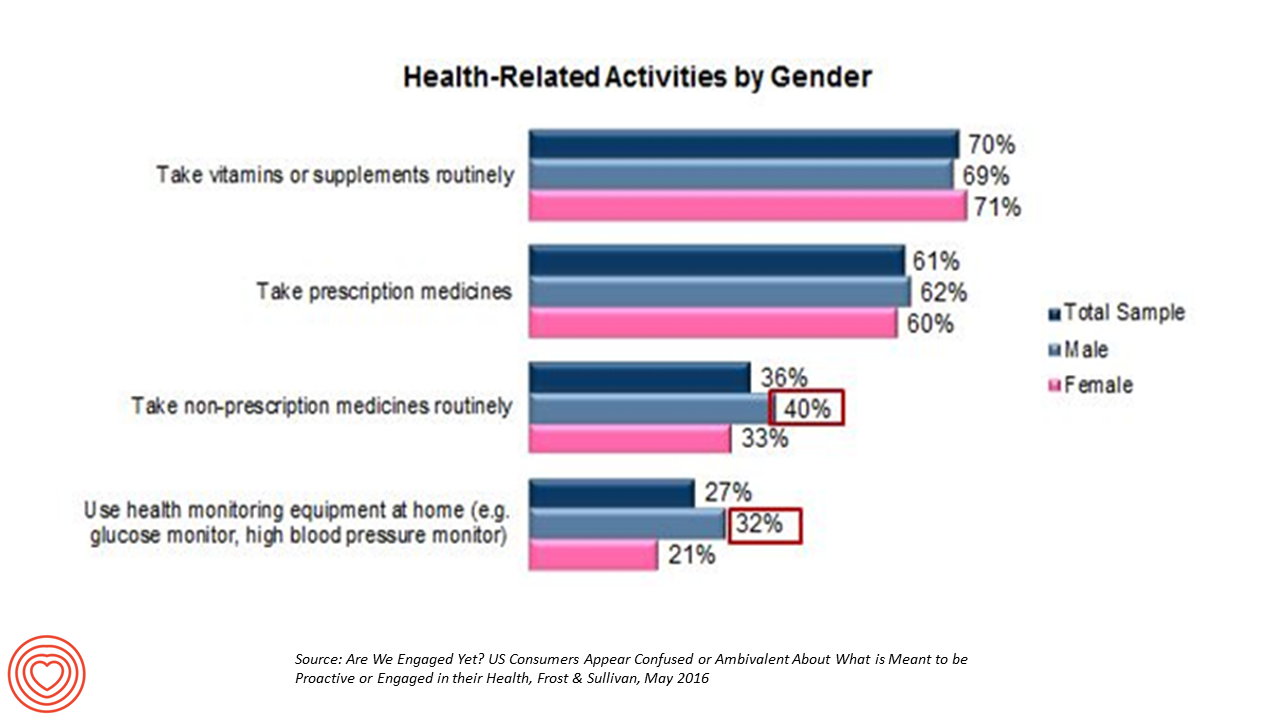
The top health-related activities among U.S. adults include routinely taking vitamins and supplements, and prescription medicines, according to Frost & Sullivan’s report, Are We Engaged Yet? Their response to the titular question lies in in the subtitle: “US consumers appear confused or ambivalent about what it means to be proactive or engaged in their health.” 1 in 2 U.S. adults says they’re “somewhat engaged” in their healthcare, according to Reenita Das’s write-up on the study in Forbes magazine. She notes that: Consumers with higher incomes have more confidence in their access to health care services and quality of care Budget-constrained consumer
Connecting Mental Health Spending to Job Creation in the U.S.
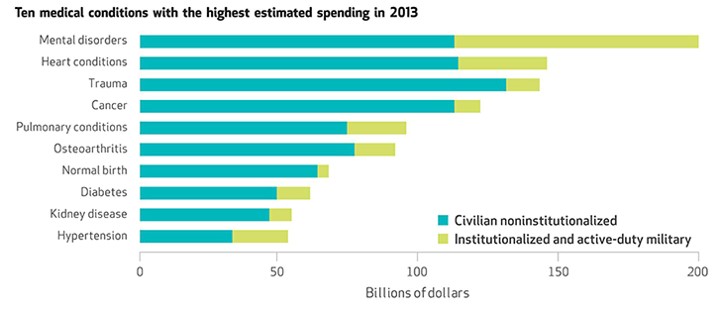
Heart disease and cancer may be the top killers of people who live in the U.S., but the top health spending line item was for mental disorders: $201 billion in 2013. The chart explains a critical aspect of the spending in that top green portion of the bar: the turquoise segment was for spending on “civilian noninstitutionalized” people, and the green was for “institutionalized and active-duty military.” Mental health issues account, by far, for the largest medical spending in a single condition as shown by the top green bar segment in the chart. These insights come from the Commerce Department’s Bureau
GoHealthEvents, An Online Source For Consumer Retail Health Opportunities
“Health comes to your local store,” explains the recently-launched portal, GoHealthEvents. This site is a one-stop shop for health consumers who are seeking health screenings and consults in local retail channels like big box stores, club stores, drug stores, and grocery stores. Events covered include cholesterol, diabetes, heart health, nutrition, osteoporosis, senior health, vaccinations and immunizations. By simply submitting a zip code, a health consumer seeking these kinds of services can identify where and when a local retailer will provide it. I searched on my own zip code in suburban Philadelphia, and found the following opportunities taking place in the
Beauty Meets Pharma in Retail Health – At Coin in Florence

All over the world, people define their health and wellness across many dimensions…physical, mental, financial, and appearance. In Florence, Italy, I happened upon a riff on this last component on “look good, feel good” at the Coin Department store located on Via Del Calzaiuoli in central Firenze. Welcome to Coin’s Health&Beauty Store. The two photos tell a story about health, where we live, work, play, and shop, the mantra for public health focused on the social determinants of health beyond healthcare. Here at Coin, adjacent to the holistic brands of Clarins and other luxury labels, is a pharmacy along with
Building Health Bridges — Health:Further Goes Beyond the Disruptive

Most people in the U.S. acknowledge that their richest country in the world has a broken healthcare system, especially when it comes to costs. A handful of think tanks and lawmakers offer fixes for American healthcare. Now there’s a new problem-solver in healthcare town, Health:Further, and they aim to move U.S. health forward by building bridges between stakeholders in the U.S. health ecosystem. My longtime colleague and friend, Andre Blackman of Pulse+Signal, has joined the organization as “Producer.” Here, we’ll learn more from my (JSK) interview with Andre (AB) about the organization, their mission, and plans to go beyond “disruption”
The 2016 THINK-Health Health/Care Forecast
It’s time to get the tea leaves out and mash up trends in my world of health, health care, technology, policy and people for 2016. We’ll start with the central player: people, consumers, patients, caregivers all. Health consumerism on the rise. People – call us patients, consumers, caregivers – will take on even more financial and clinical decision making risk in 2016. Growing penetration of high-deductible and consumer-driven health plans will push (not just nudge) people into the role of health care consumers, and the emerging businesses and programs serving the transparency market for price and quality will gain traction
Connectivity Is A Social Determinant of Health
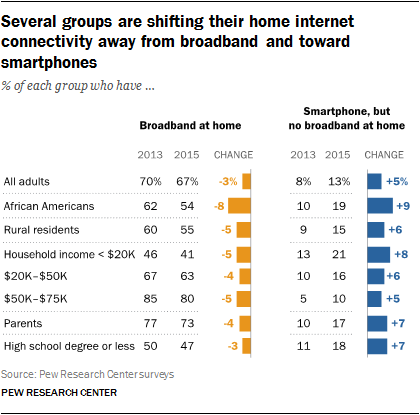
It’s Christmastime, so I’m thinking about connections. “Connectivity” can be social (offline and online), which is indeed a health factor (see Christakis and Fowler on being Connected). But the kind of connectivity to which I’m referring is broadband, WiFi, the kind most often associated with data plans, cable to the home, and free WiFi at your favorite coffee or fast food joint. That kind of connectivity is also a social determinant of health, and is increasingly becoming so for all people. Yet as peoples’ need for internet connectivity is fast growing, especially for health, home broadband connectivity has reached a
Social Determinants Impact Health More Than Health Care
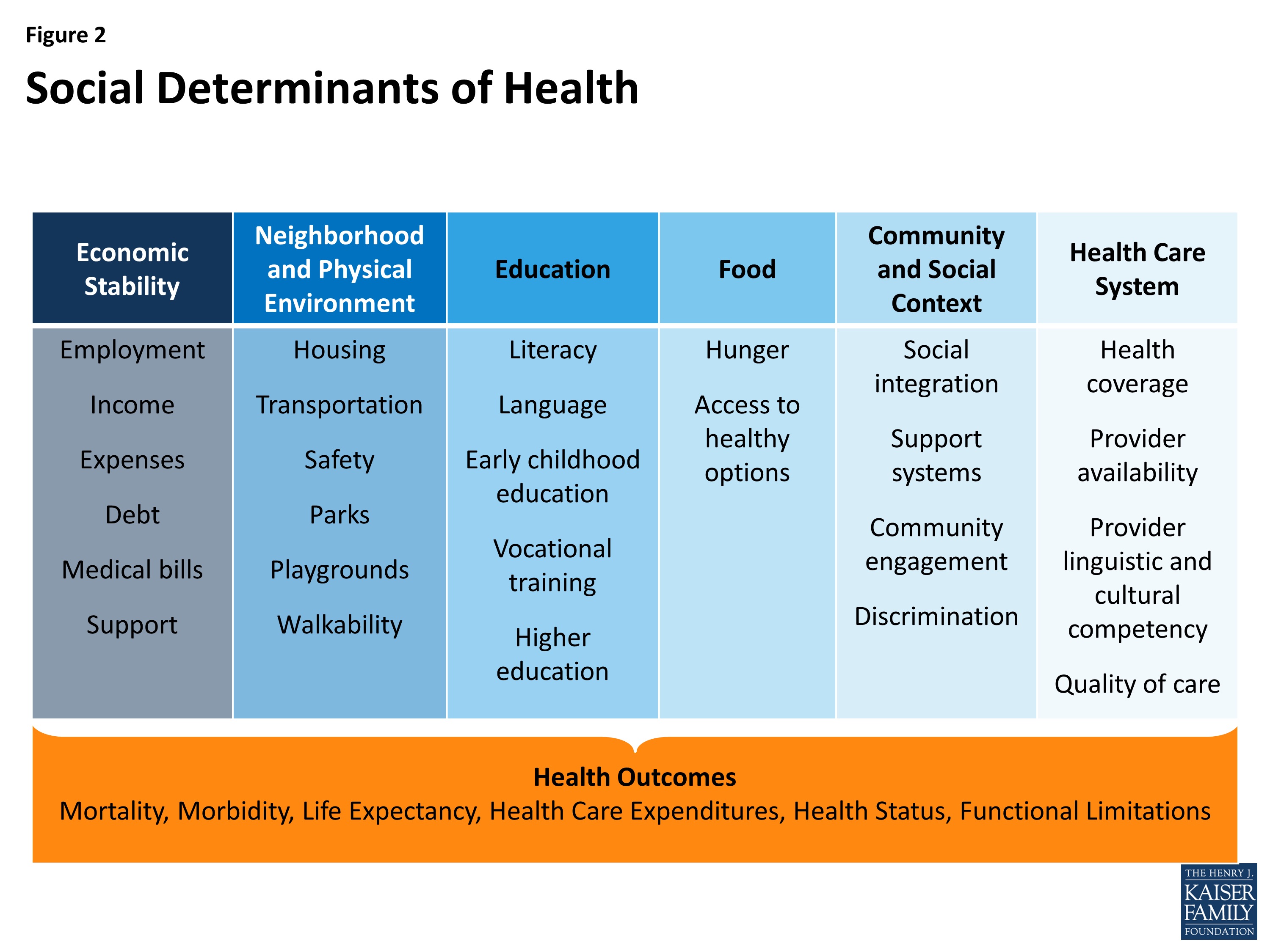
The factors of where people are born, live, work and age — social determinants — shape human health more than health care. Yet in the U.S. much more resource per capita is funneled into healthcare services than into social ones. Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity was published by The Kaiser Commission on Medicaid and the Uninsured in November 2015, calling attention to the opportunity and wisdom of baking health into all public policy. The social determinants of health (SDOH) include economic stability, the physical environment and neighborhood, education, food, community and
Death Rates Rise For Middle-Age White Men: Economics and Mental Health in America
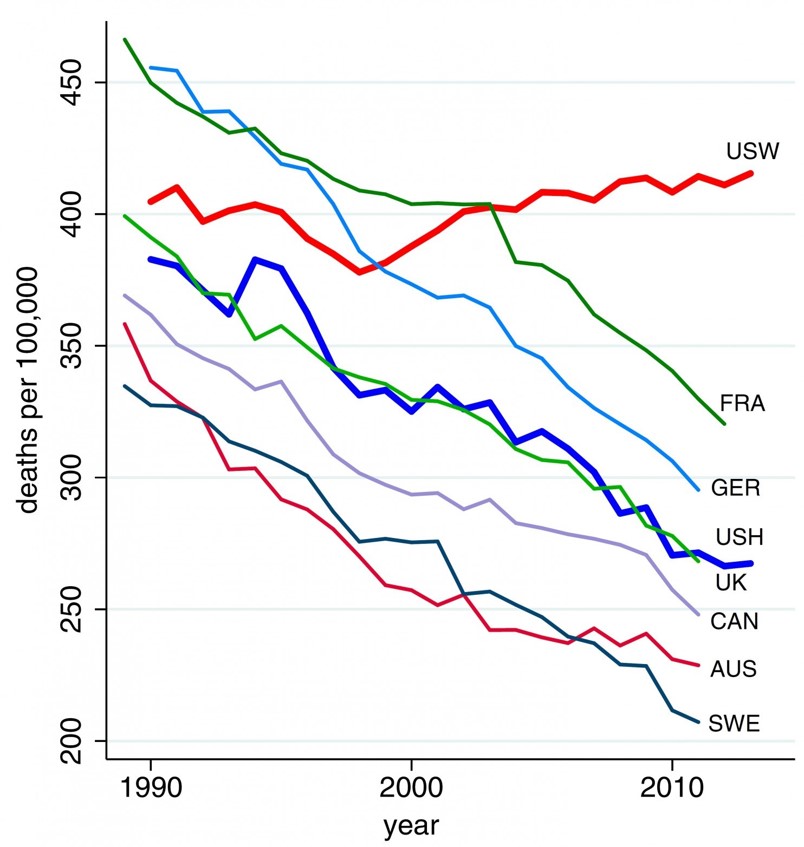
Shocking statistics were published in this week’s Proceedings of the National Academy of Sciences showing rising death rates for middle-age men. The major causes: suicide, drug and alcohol poisoning, and liver diseases. The line chart illustrates the death rates per 100,000 population of U.S. whites (“USW”), the top line on the graph, compared with 45-54 year old men in France, Germany, the United Kingdom, Canada, Australia, and Sweden — along with U.S. Hispanic males (“USH”) — for whom death rates have fallen since 1990. The authors note that the increase in midlife mortality is only partly understood. Increased availability of
Virtual Visits Would Conserve Primary Care Resources in US Healthcare
By shifting primary care visits by 5 minutes, moving some administrative tasks and self-care duties to patients, the U.S. could conserve billions of dollars which could extend primary care to underserved people and regions, hire more PCPs, and drive quality and patient satisfaction. Accenture’s report, Virtual Health: The Untapped Opportunity to Get the Most out of Healthcare, highlights the $10 bn opportunity which translates into conserving thousands of primary care providers. PCPs are in short supply, so virtual care represents a way to conserve precious primary care resources and re-deploy them to their highest-and-best-use. The analysis looks at three scenarios
The rise and rise of noncommunicable diseases
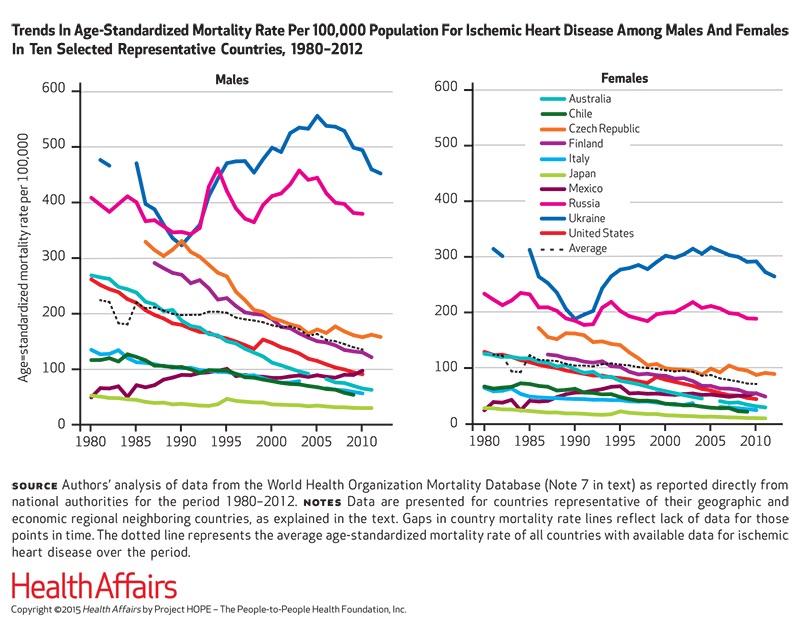
Noncommunicable diseases (NCDs) are the #1 cause of death in the world. NCDs are the yin to the yang of infectious diseases. Mortality from infectious disease has fallen as national economies have developed, while NCDs such as heart disease, respiratory disease, cancer, diabetes, and other NCDs are a growing burden. Health Affairs devotes its September 2015 issue to The Growing Burden of Noncommunicable Diseases, featuring research focusing both on global trends and U.S.-specific challenges. In their look into the relationships between NCDs, unhealthy lifestyles and country wealth, Thomas Bollyky et. al. note that NCDs aren’t only the “diseases of affluence,”
Beauty, Health and Power
CVS is expanding the beauty aisles in stores, along with adding fresh and refrigerated foods and healthy snacks to its offerings. This is part of the company’s re-positioning in its post-tobacco mission, having re-branded from CVS/pharmacy to CVS Health last year. (You can read more about this strategic transformation here in Health Populi and here in my Huffington Post column). When CVS made this announcement, a portfolio manager for Gabelli Funds noted that health and beauty products have very high profit margins. These margins will be useful as CVS replaces the tobacco sales lost last year when the company went tobacco-free.
Employers go beyond physical health in 2015, adding financial and stress management

Workplace well-being programs are going beyond physical wellness, incorporating personal stress management and financial management. Nearly one-half of employers offer these programs in 2015. Another one-third will offer stress management in the next one to three years, and another one-fourth will offer financial management to workers, according to Virgin Pulse’s 2015 survey of workplace health priorities, The Busness of Healthy Employees. The survey was published June 1st 2015, kicking off Employee Wellbeing Month, which uses the Twitter hashtag #EWM15. It takes a village to bolster population health and wellness, so Virgin Pulse is collaborating with several partners in this effort
All women are health workers
The spiritual and emotional top the physical in women’s definition of “health,” based on a multi-country survey conducted in Brazil, Germany, Japan, the UK and the U.S. The Power of the Purse, a research project sponsored by the Center for Talent Innovation, underscores women’s primary role as Chief Medical Officers in their families and social networks. The research was sponsored by health industry leaders including Aetna, Bristol-Myers Squibb, Cardinal Health, Eli Lilly and Company, Johnson & Johnson, Merck & Co., Merck KGaA, MetLife, Pfizer, PwC, Strategy&, Teva, and WPP. The study’s summary infographic is titled How the Healthcare Industry Fails
Mental health at the workplace – US companies rank #1 for stress
People with anxiety, depression, interpersonal challenges, and substance abuse go to work every day. Together, these factors erode the mental health and wellbeing of workers, and this negatively impacts companies’ productivity, workplace morale, and profitability. Employers are increasingly taking notice of their role in promoting mental health on-the-job, a trend captured in the report Promoting Mental Well-being: Addressing Worker Stress and Psychosocial Risks, an international survey of employers published in May 2015 by Buck Consultants, part of Xerox. The survey polled 439 employers in 31 countries, and the report focuses on the results in four of those nations: Brazil, Singapore, the
Supersize Rx: the impact of specialty drug spending and Hep C in 2014
The number of people in the U.S. spending over $100,000 a year on prescription drugs tripled in 2014, according to Super Spending: U.S. Trends in High-Cost Medication Use, from The Express Scripts Lab. Express Scripts is a pharmacy benefits management company that manages over one billion prescriptions a year. The company analyzed prescription drug claims for 31.5 million health plan members for this study, in commercially insured, Medicare, and Medicaid plans. The big-dollar story in 2014 was Hepatitis C, with a relatively small patient population but a super-sized drug spend as the first chart shows: a very tall blue bar (Rx
Doctors who write right: Gawande, Topol and Wachter put people at the center of health/care
There’s a trifecta of books written by three brilliant doctors that, together, provide a roadmap for the 21st century continuum of health care: The Patient Will See You Now by Eric Topol, MD; The Digital Doctor from Robert Wachter, MD; and, Being Mortal, by Atul Gawande. Each book’s take provides a lens, through the eyes of a hands-on healthcare provider, on healthcare delivery today (the good, the warts and all) and solutions based on their unique points-of-view. This triple-review will move, purposefully, from the digitally, technology optimistic “Gutenberg moment” for democratizing medicine per Dr. Topol, to the end-game importance of
A health agenda comes to the 2015 Oscars
The 87th annual 2015 Oscars show (#Oscars15) feted more than the movie industry: the event celebrated health in both explicit and subtle ways. Julianne Moore took the golden statuette for Best Actress, playing the title role in Still Alice, the story a woman diagnosed with early-onset Alzheimer’s Disease. In accepting her award, Moore spoke of the need to recognize and “see” people with Alzheimer’s – so many people feel isolated and marginalized, Moore explained. Movies help us feel seen and not alone – and people with Alzheimer’s need to be seen so we can find a cure, she asserted. See Moore’s lovely
Hug your physician – chances are, s/he’s burned out
If you’re meeting with a physician in the next week or two, put on your empathy hat: chances are, they are feeling burned-out. Overall 46% of physicians report they were burned out in 2014, up from just under 40% last year. Medscape’s Physician Lifestyle Report 2015 finds that at least one-half of physicians are burned-out who work in critical care, emergency medicine, family medicine, internal medicine, general surgery, and infectious disease (including HIV). And, at least 37% of physicians are burned-out working in all other specialties, shown in the first chart. Medscape gauges doctors’ self-assessments of burnout with a lens
Health and wellness at CES 2015 – trend-weaving the big ideas
Health is where we live, work, play and pray — my and others’ mantra if we want to truly bend (down) the cost curve and improve medical outcomes. If we’re serious about achieving the Triple Aim — improving public health, lowering spending, and enhancing the patient/health consumer experience (which can drive activation and ongoing engagement) — then you see health everywhere at the 2015 Consumer Electronics Show in Las Vegas this week. With this post, I’ll share with you the major themes I’m seeing at #CES2015 related to health, wellness, and DIYing medical care at home. The meta: from health care to self-care.
Trend-weaving the 2015 health care trends
‘Tis the season for annual health trendcasting, which is part of my own business model. Here’s a curated list of some of my favorite trend reports for health care in the new year, with my Hot Points in the conclusion, below, summarizing the most salient trends among them. TechCrunch’s Top 5 Healthcare Predictions for 2015: In this succinct forecast, Walmart grows its presence as a health plan, startups get more pharm-funding, hospitals channel peer-to-peer lending, Latinos emerge as a “most-desired” health care segment, and Amazon disrupts the medical supply chain. Experian 2015 Data Breach Forecast: Healthcare security breaches will be
Irrational exuberance in mobile health? Live from the mHealth Summit 2014
Mobile and digital technologies will bend the health care cost curve, drive individual and population health, and solve the nagging challenge of health disparities. Mobile and digital technologies will increase costs to health providers, disrupt work flows and lower clinicians’ productivity, and hit a market bubble. Depending on your lens into mHealth, and what product categories and user segments you’re looking at, all of the above can be true. The plenary session of the 2014 mHeath Summit kicked off with Dr. Harry Leider, Chief Medical Information Officer of Walgreens, who spoke of the pharmacy’s evolving role across the entire continuum of care,
Inflection point for telehealth in 2014
The supply side of telehealth has been readying itself for nearly a decade. The demand side appears to be aligning in 2014 for adoption to grow and sustain (some) solid business models. On the demand side, Towers Watson’s 2014 survey of large employers forecasts growth among companies that will offer telemedicine in 2015. Towers found that 37% of employers planned to offer telemedicine to workers as a lower-cost site of care; 34% more employers were considering telemedicine in 2016 or 2017. The health benefits adviser calculates that employers could save over $6 billion if industry replaces virtual health consultations with
Stress Is US
“Reality is the leading cause of stress among those in touch with it,” Lily Tomlin once quipped. Perhaps in 2014, America is the land of stress because we’re all so in touch with reality. THINK: reality TV, social networks as the new confessional, news channeling 24×7, and a world of too much TMI. So no surprise, then, that one-half of the people in the U.S. have had a major stressful event or experience in the last year. And health tops the list of stressful events in This American Life in the forms of illness and disease (among 27% of people)
The VA is a telehealth leader
“Telehealth isn’t about seeing a provider by video: it’s about decision making,” Dr. Adam Darkins, leader of the U.S. Department of Veterans Affairs National Telehealth Programs, told the audience in his keynote address at the Government Health IT Conference in Washington, DC, on June 17, 2014. Dr. Darkins, trained as a neurosurgeon, realized earlier in his career “time and again,” he said, that he should have seen his patients more frequently in-between face-to-face visits. “A good decision downstream can make a lot of difference to someone’s longevity,” Dr. Darkins recognized. He’s worked with a team at the VA to build
mHealth will join the health ecosystem – prelude to the 2014 Consumer Electronics Show
The rise of digital health at the 2014 Consumer Electronics Show signals the hockey-stick growth of consumer-facing health devices for fitness and, increasingly, more medical applications in the hands of people, patients, and caregivers. This year at #CES2014, while the 40% growth of the CES digital health footprint will get the headlines, the underlying story will go beyond wristbands and step-tracking generating data from an N of 1 to tools that generate data to bolster shared-decision making between people and the health system, and eventually support population health. For example: – Aetna is partnering with J&J to deploy their Care4Today
When health care costs are a side effect
4 in 5 U.S. patients – 81% of them – want an equal say in health care decisions with their care provider, according to a 2013 Institute of Medicine study. At the same time, patients choose to take “drug holidays,” opting out of taking three or more doses of medicines in a row, or adopt “trail mix” approaches to taking prescriptions, casually and inappropriately mixing Rx drugs. Welcome to your world, pharma industry: where people say they want control, but somehow don’t exercise it in the way you — drug companies — define as “compliance” or “adherence.” Customer experience in
Mobile health apps – opportunity for patients and doctors to co-create the evidence
There are thousands of downloadable apps that people can use that touch on health. But among the 40,000+ mobile health apps available in iTunes, which most effectively drive health and efficient care? To answer that question, the IMS Institute for Healthcare Informatics analyzed 43,689 health, fitness and medical apps in the Apple iTunes store as of June 2013. These split into what IMS categorized as 23,682 “genuine” health care apps, and 20,007 falling into miscellaneous categories such as product-specific apps, fashion and beauty, fertility, veterinary, and apps with “gimmicks” (IMS’s word) with no obvious health benefit. Among the 23,682 so-called
7 Women and 1 Man Talking About Life, Health and Sex – Health 2.0 keeping it real
Women and binge drinking…job and financial stress…sleeplessness…caregiving challenges…sex…these were the topics covered in Health 2.0 Conference’s session aptly called “The Unmentionables.” The panel on October 1, 2013, was a rich, sobering and authentic conversation among 7 women and 1 man who kept it very real on the main stage of this mega-meeting that convenes health technology developers, marketers, health providers, insurers, investors, patient advocates, and public sector representatives (who, sadly, had to depart for Washington, DC, much earlier than intended due to the government shutdown). The Unmentionables is the brainchild of Alexandra Drane and her brilliant team at the Eliza
Chief Health Officers, Women, Are In Pain
Women are the Chief Health Officers of their families and in their communities. But stress is on the rise for women. Taking an inventory on several health risks for American women in 2013 paints a picture of pain: of overdosing, caregiver burnout, health disparities, financial stress, and over-drinking. Overdosing on opioids. Opioids are strong drugs prescribed for pain management such as hydrocodone, morphine, and oxycodone. The number of opioid prescriptions grew in the U.S. by over 300% between 1999 and 2010. Deaths from prescription painkiller overdoses among women have increased more than 400% since 1999, compared to 265% among men.
What to expect from health care between now and 2018
Employers who provide health insurance are getting much more aggressive in 2013 and beyond in terms of increasing employees’ responsibilities for staying well and taking our meds, shopping for services based on cost and value, and paying doctors based on their success with patients’ health outcomes and quality of care. Furthermore, nearly one-half expect that technologies like telemedicine, mobile health apps, and health kiosks in the back of grocery stores and pharmacies are expected to change the way people regularly receive health care. What’s behind this? Increasing health care costs, to be sure, explains the 18th annual survey from the National
U.S. Health Costs vs. The World: Is It Still The Prices, and Are We Still Stupid?
Comparing health care prices in the U.S. with those in other developed countries is an exercise in sticker shock. The cost of a hospital day in the U.S. was, on average, $4,287 in 2012. It was $853 in France, a nation often lauded for its excellent health system and patient outcomes but with a health system that’s financially strapped. A routine office visit to a doctor cost an average of $95 in the U.S. in 2012. The same visit was priced at $30 in Canada and $30 in France, as well. A hip replacement cost $40,364 on average in the
The physician time-squeeze and burnout: just-in-time information is part of the solution
One in two doctors is burned out. Physicians are seeing more patients in a day and spend less time with each of them. This leads to job burnout, and greater probability for medical errors and eventual liability challenges, along with feeling pushed toward early retirement. In a study published in August 2012 in the Archives of Internal Medicine, Mayo Clinic researchers learned that physicians are more burned out than workers in any other profession. And those at greatest risk of “being on a hamster wheel,” as Dr. Jeff Cain, president-elect of the American Academy of Family Physicians describes the scenario, are primary
Wired health: living by numbers – a review of the event
Wired magazine, longtime evangelist for all-things-tech, has played a growing role in serving up health-tech content over the past several years, especially through the work of Thomas Goetz. This month, Wired featured an informative section on living by numbers — the theme of a new Wired conference held 15-16 October 2012 in New York City. This feels like the week of digital health on the east coast of the U.S.: several major meetings have convened that highlight the role of technology — especially, the Internet, mobile platforms, and Big Data — on health. Among the meetings were the NYeC Digital Health conference, Digital
Antidepressant Nation – and how computerized CBT can help primary care in America
The antidepressant market is worth $20 billion in the U.S. Antidepressants were the third most common prescription drug taken by Americans of all ages in 2005-2008 and the most frequently used by people age 18-44 (according to the National Center for Health Statistics). About one in 10 Americans age 12 and over takes an antidepressant medication. But there is little evidence that pharmacotherapy should be used as a first line of treatment for mild to moderate depression. Why are anti-depressants the first line of treatment for mild to moderate depression in the U.S.? The answer lies in the fact that
The Online Couch: how “safe Skyping” is changing the relationship for patients and therapists
Skype and videoconferencing have surpassed the tipping point of consumer adoption. Grandparents Skype with grandchildren living far, far away. Soldiers converse daily with families from Afghanistan and Iraq war theatres. Workers streamline telecommuting by videoconferencing with colleagues in geographically distributed offices. In the era of DIY’ing all aspects of life, more health citizens are taking to DIY’ing health — and, increasingly, looking beyond physical health for convenient access to mental and behavioral health services. The Online Couch: Mental Health Care on the Web is my latest paper for the California HealthCare Foundation. Among a range of emerging tech-enabled mental health
The Online Couch: how the Internet and mobile are changing mental and behavioral health care
Therapy is now a click away, whether on a computer, a smartphone or a tablet. Drs. Freud, Ellis and Beck, heads-up: the Internet is the new couch of psychiatry. That is, at least for people with mild to moderate depression and those with anxiety, as I report in my latest paper for the California HealthCare Foundation, The Online Couch: Mental Health Care on the Web. Many factors are aligning that make therapy online an effective extension of face-to-face therapy for the right patients at the right time in the U.S.: An undersupply of psychologists, psychiatrists, and other therapists, especially in rural and





 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.