AI: Patients Included

“Clinical transformation with AI is easier without patients.” When Dr. Grace Cordovano heard this statement on a panel of physicians convening to share perspectives on the future of AI in health care held in early March 2024, the board-certified patient advocate felt, in her words, “insulted on behalf of the patient communities I know that are working tirelessly to advance AI that works for them.” “The healthcare ecosystem and policy landscape must formally recognize patients as end-users and co-creators of AI,” Cordovano wrote to me in an e-mail exchange. “Patients, their care partners, caregivers, and advocates are already utilizing AI
Access to Technology Is the New Pillar for Well-Being: CES & the UN Partner for Human Security for All

In kicking off #CES2024, CTA’s researchers noted the acceleration of global connectivity, with gaps in peoples’ ability to connect depending where they live: by region, the percent of people connected to the internet today are, according to CTA’s data, 92% in the U.S. 87% in the E.U. 76% in Latin America 73% in China 55% in Nigeria 46% in India. Such gaps in connectivity threaten peoples’ individual well-being, but also social and political stability that impacts the entire world’s security. And not to overlook, as well, the promise of AI to do good at scale at the enterprise-level, globally.
#BeBurnsAware – What To Know on National Burn Awareness Day
Today 11th October is National Burn Awareness Day 2023, and I’m supporting the effort for all of us to #BeBurnsAware. I have become more bullish on Burn Awareness as I’ve come to learn more about the impact burns have on public, family, and children’s health globally. My teacher for better understanding burns and public health has been Krissie Stiles, a long-time burns nurse specialist and Ambassador to the Children’s Burns Trust in the UK. Meet Krissie. Burns are a global public health challenge, which I detailed here in Health Populi earlier this year. Today
Can Artists Help to Remake Medicine? A New Book Asks and Answers (Yes!)
What if we asked an artist to re-imagine what health care could be? How might Van Gogh redesign a patient room akin to his room at Arles, or Michelangelo re-think general surgery? How might Thoreau take us on a nature walk for our mental health, or Basquiat channel his inner Da Vinci for a version of Jean-Michel’s Anatomy? In her new book, Artists Remaking Medicine. Emily Peters confronts health care’s paralyzing complexity (her words in the introduction) to invite a community of artists and artful thinkers to share their visions for remaking health care.
Quick, Accessible, Inexpensive Health Care – A Retail Health Update from Amazon and Dollar General

Two announcements this week add important initiatives to patients’ growing choices that speak to their consumer-sides’ sense of value and personal healthcare cost-containment: Amazon launched RxPass, a generic medicines subscription service; and, Dollar General promoted its mobile health service powered by DocGo on demand for health visits, “right outside the store.” These two programs come from outside of the legacy health care system of so-called incumbents — hospitals, health systems, health insurance — leveraging two brand-names beloved to many consumers for convenience, price transparency, and sheer cost. First, check out Amazon Pharmacy’s RxPass. Amazon
Your State as a Determinant of Health: Sharecare’s 2021 Community Well-Being Index
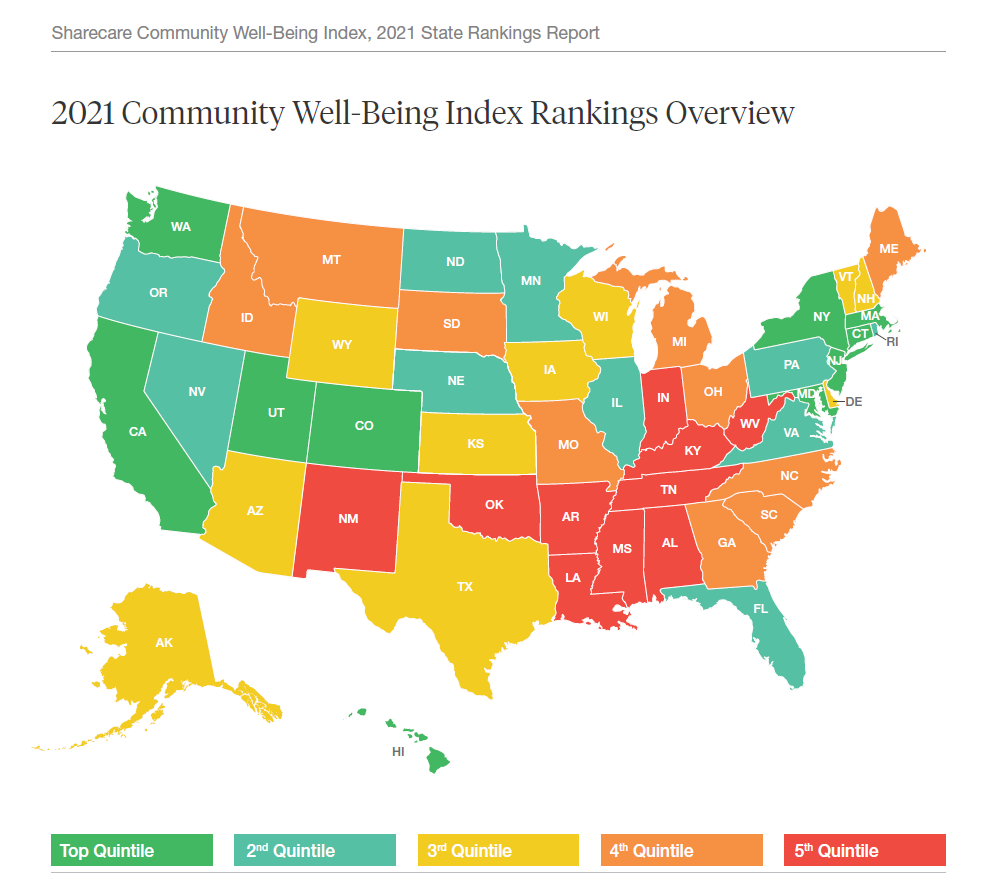
People whose sense of well-being shifted positively in the past two years are finding greater personal purpose and financial health, we see in Sharecare’s Community Well-Being Index – 2021 State Rankings Report. Sharecare has been annually tracking well-being across the 50 U.S. states since 2008. When the study launched, Well-Being Index evaluated five domains: physical, social, community, purpose, and financial. In 2020, Sharecare began a collaboration with the Boston University School of Public Health to expand the Index, including drivers of health such as, Healthcare access (like physician supply per 1,000
How Trust and Geopolitics Will Impact Health and Business – Edelman 2022 Trust Barometer at the World Economic Forum in Davos

When we think about the state of Trust in in mid-2022, there is some good news: Trust is rising (at least in democratic countries, while falling in autocratic ones). The bad news: the gap in Trust has dramatically widened between higher-income people compared with those earning lower-incomes, globally. And that gap is “tinder” that can be quickly sparked into a socio-political fire in countries around the world, Richard Edelman cautioned today when introducing the latest look at the 2022 Edelman Trust Barometer, focusing on geopolitics and business. We have never seen numbers like this
Three in Five People 50+ in the US Will Likely Use Telehealth In the Future – An Update from AARP
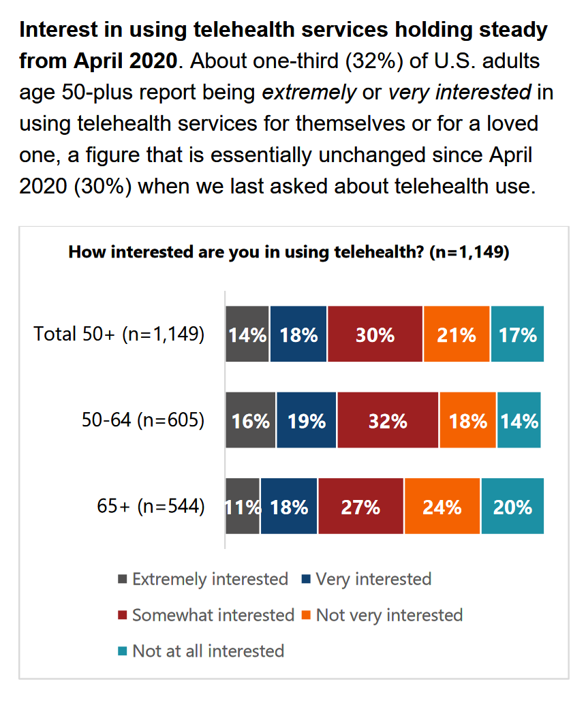
“Telehealth certainly appears to be here to stay,” the AARP forecasts in An Updated Look at Telehealth Use Among U.S. Adults 50-Plus from AARP. Two years after the emergence of the COVID-19 pandemic, one-half of U.S. adults over 50 said they or someone in their family had used telehealth. In early 2022, over half of those over 50 (the AARP core membership base) told the Association they would likely use telehealth in the future. This future expectation varies by race, the implications of which I discuss below in
Primary Care in the U.S. – Still a Weak Backbone for the Health of Health Citizens
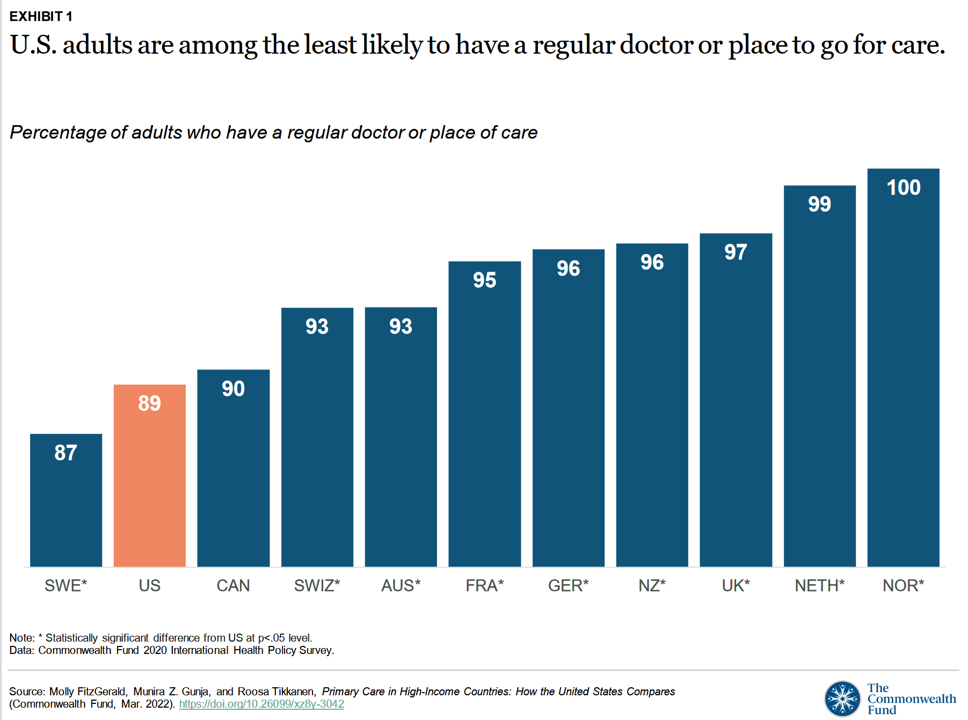
Compared with health citizens living in other wealthy countries, people living in the U.S. are still among the least likely to have a regular doctor or place to go for care. Thus, millions of Americans continue to lack access to primary care compared with peers in other nations, according to a report from The Commonwealth Fund. The Commonwealth Fund has tracked primary care access for many years, and over time has found the United States to lack the kind of primary care “backbone” that many wealthy nations have — whose health citizens also enjoy much better health outcomes that relate
Love and Health: The Education of Abner Mason, SameSky Health
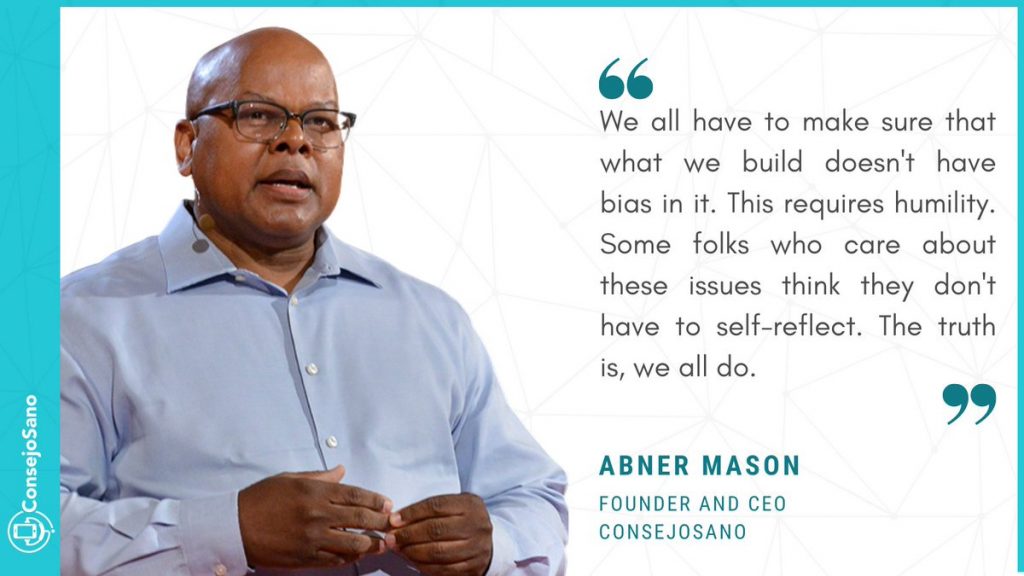
It felt super appropriate that I met up with Abner Mason, Founder of SameSky Health, on Valentine’s Day 2022. While we conversed via Zoom, Abner’s positive energy vibrated over the 5,600 miles between him in LA County and me in Brussels, Belgium – nine hours apart, but in the proverbial same room in the conversation. My initial ask of Abner was to discuss the re-branding of ConsejoSano to SameSky Health, but I first wanted to hear the man’s origin story. And that, you will learn, has everything to do with loving parents, the power of education from a young age,
Health Citizens Link Their Views on Democracy, the Economy and the Pandemic
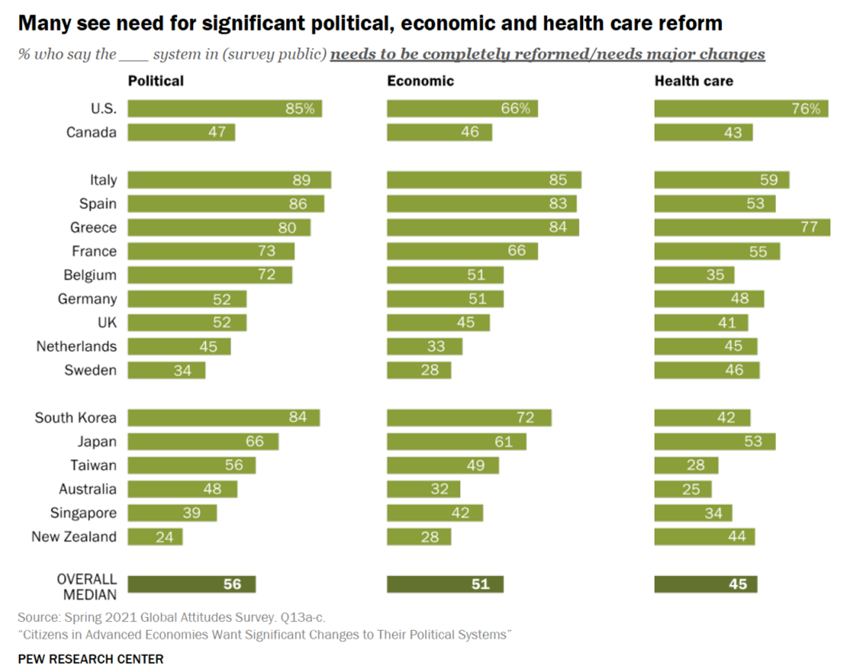
The pandemic has put health care top-of-mind for health citizens the world over. As the public health crisis continues its up-and-downticks around the globe, people are connecting health care to their national economies and politics, based on a global survey from the Pew Research Center, Citizens in Advanced Economies Want Significant Changes to Their Political Systems. For this analysis, the Pew research team assessed the views of some 2,600 health citizens living in 17 developed countries in February 2021. The study report was published in late October 2021. Shown in the first bar chart, the majority of people in at least
Designing Digital Health for Public Health Preparedness and Equity: the Consumer Tech Association Doubles Down
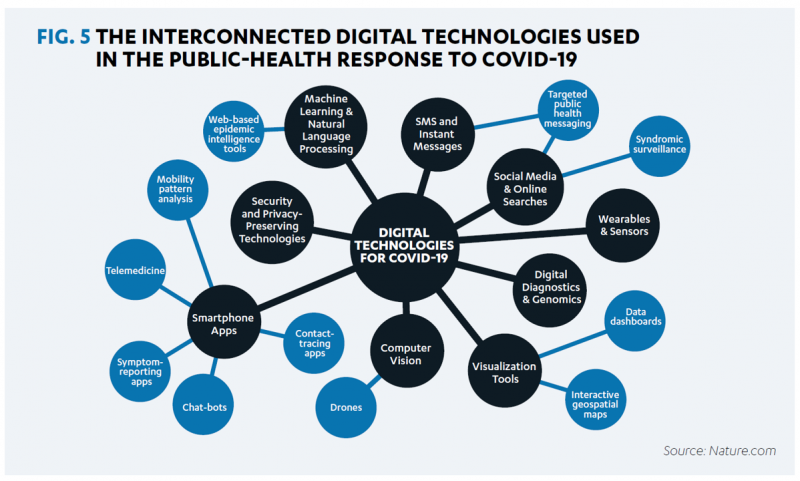
A coalition of health care providers, health plans, technology innovators, NGOs, and medical societies has come together as the Public Health Tech Initiative (PHTI), endorsed by the Consumer Technology Association (CTA) with the goal of advancing the use of trustworthy digital health to proactively meet the challenge of future public health emergencies….like pandemics. At the same time, CTA has published a paper on Advancing Health Equity Through Technology which complements and reinforces the PHTI announcement and objective. The paper that details the PHTI program, Using Heath Technology to Response to Public Health Emergencies, identifies the two focus areas: Digital health
The Biggest Threat to Our Health Isn’t the Next Pandemic or Cancer…It’s Climate Change
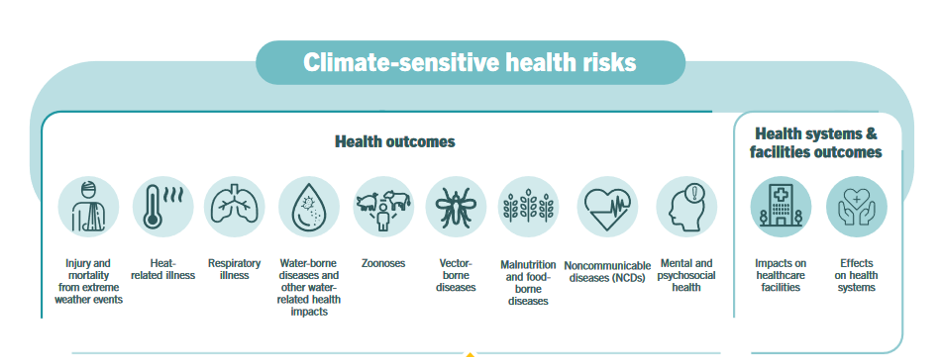
Before the coronavirus emerged, the top causes of death in developed countries were heart disease, cancers, diabetes, and accidents. Then COVID-19 joined the top-10 list of killers in the U.S. and the issue of pandemic preparedness for the next “Disease X” became part of global public health planning. But the biggest health threat to human life is climate change, according to a new report from the World Health Organization titled The Health Argument for Climate Action. It’s WHO’s special report on climate change and health, dedicated to the memory of Ella Kissi-Debrah — a child who died succumbing to impacts
#LoveThyNeighbor – A Faith-Based Call for Vaccination

The Catholic Health Association (CHA) is urging Americans to “love thy neighbor” by getting the COVID-19 vaccine, Sister Mary Haddad wrote in an editorial published in Modern Healthcare, published on September 3, 2021. Sister Mary is CEO and President of CHA. “Some may suggest that there are moral and religious concerns to receiving the COVID-19 vaccine,” Sister Mary observed. “We strongly affirm the position of the leaders of the Catholic Church: the vaccines are morally acceptable and getting vaccinated is “an act of love.” she asserted. CHA launched a portal on the act of love, featuring lots of science-based articles
Health Disparities in America: JAMA Talks Structural Racism in U.S. Health Care

“Racial and ethnic inequities in the US health care system have been unremitting since the beginning of the country. In the 19th and 20th centuries, segregated black hospitals were emblematic of separate but unequal health care,” begins the editorial introducing an entire issue of JAMA dedicated to racial and ethnic disparities and inequities in medicine and health care, published August 17, 2021. This is not your typical edition of the Journal of the American Medical Association. The coronavirus pandemic has changed so many aspects of American health care for so many people, including doctors. Since the second quarter of 2020,
Virtual Health Tech Enables the Continuum of Health from Hospital to Home

In the COVID-19 pandemic, as peoples’ daily lives shifted closer and closer to home, and for some weeks and months home-all-the-time, health care, too, moved beyond brick-and-mortar hospitals and doctors’ offices. The public health crisis accelerated “what’s next” for health care delivery, detailed in A New Era of Virtual Health, a report published by TripleTree. TripleTree is an investment bank that has advised health care transactions since 1997. As such, the team has been involved in digital health financing and innovation for 24 years, well before the kind of platforms, APIs, and cloud computing now enabling telehealth and care, everywhere. The
The Pandemic’s Death Rate in the U.S.: High Per Capita Income, High Mortality
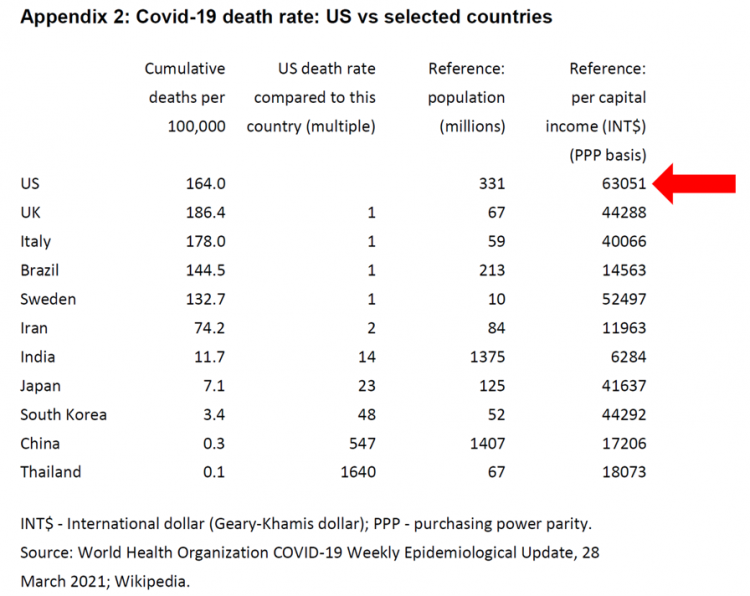
The United States has among the highest per capita incomes in the world. The U.S. also has sustained among the highest death rates per 100,000 people due to COVID-19, based on epidemiological data from the World Health Organization’s March 28, 2021, update. Higher incomes won’t prevent a person from death-by-coronavirus, but risks for the social determinants of health — exacerbated by income inequality — will and do. I have the good fortune of access to a study group paper shared by Paul Sheard, Research Fellow at the Mossaver-Rahmani Center for Business and Government at the Harvard Kennedy School. In reviewing
Emerging with A Stronger Healthcare System Post-COVID: NAM’s Lessons Learned
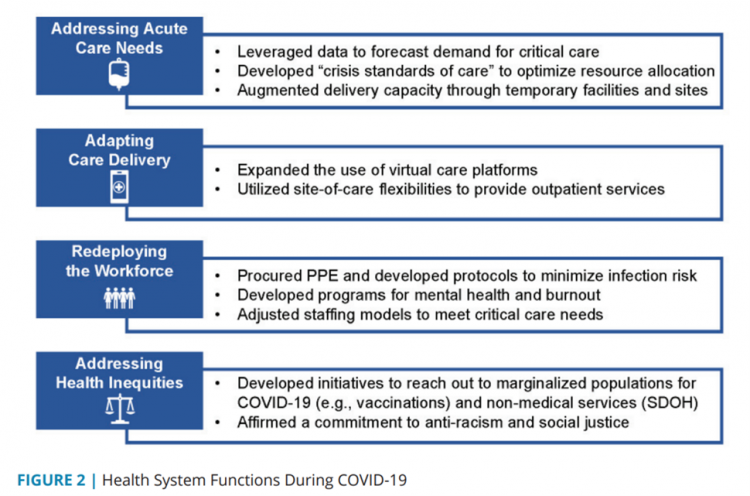
The coronavirus pandemic exposed weaknesses in the U.S. health care system that existed before the public health crisis. What lessons can be learned from the COVID-19 stress-test to build American health care back better? The National Academy of Medicine is publishing nine reports addressing health stakeholder segments impacted and re-shaped by COVID-19 — for public health, quality and safety, health care payers, clinicians, research, patients-families-communities, health product manufacturers, digital health, and care systems. The report on health care systems and providers was released this week: COVID-19 Impact Assessment: Lessons Learned and Compelling Needs was authored by experts on the front-line
The Patient Safety Issue of Racial Disparities and the Opportunity for “Health Equity By Design”

In 2021, racial and ethnic disparities in healthcare are a top patient safety issue, according to ECRI’s annual list of major concerns facing healthcare consumers’ risks to adverse events that can harm them. ECRI has published their annual Top 10 list since 2018, when the list featured diagnostic errors, o behavioral health needs in acute care settings, and patient engagement and health literacy — all of which play into this year’s #1 issue, racial and ethnic disparities in health care. In fact, among the risks in this year’s Top Ten list, eight were accelerated and highlighted by the COVID-19 pandemic
Stress in America, One Year into the Pandemic – an APA Update on Parents, Healthcare Workers, and Black Americans
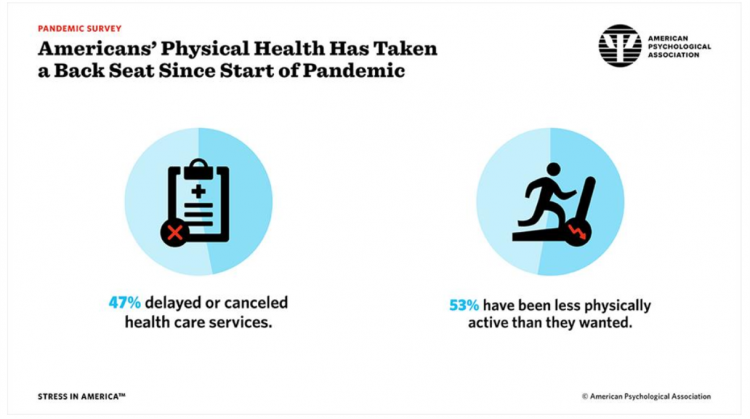
A Year into our collective coronavirus experience, Americans remain stressed, with physical health taking a back seat to our daily grinds based on the 2021 Stress in America survey from the American Psychological Association (APA). The APA has been updating us on U.S.-stress for several years, and more frequently since the start of the COVID-19 pandemic at the start of 2020. In their latest report, APA updates their previous profiles of Americans’ stress looking into different demographic groups and coping mechanisms. The topline, across all adults living in America, is that one-half have delayed or cancelled health care services. One-half has
How Young People Are Using Digital Tools to Help Deal with Mental Health
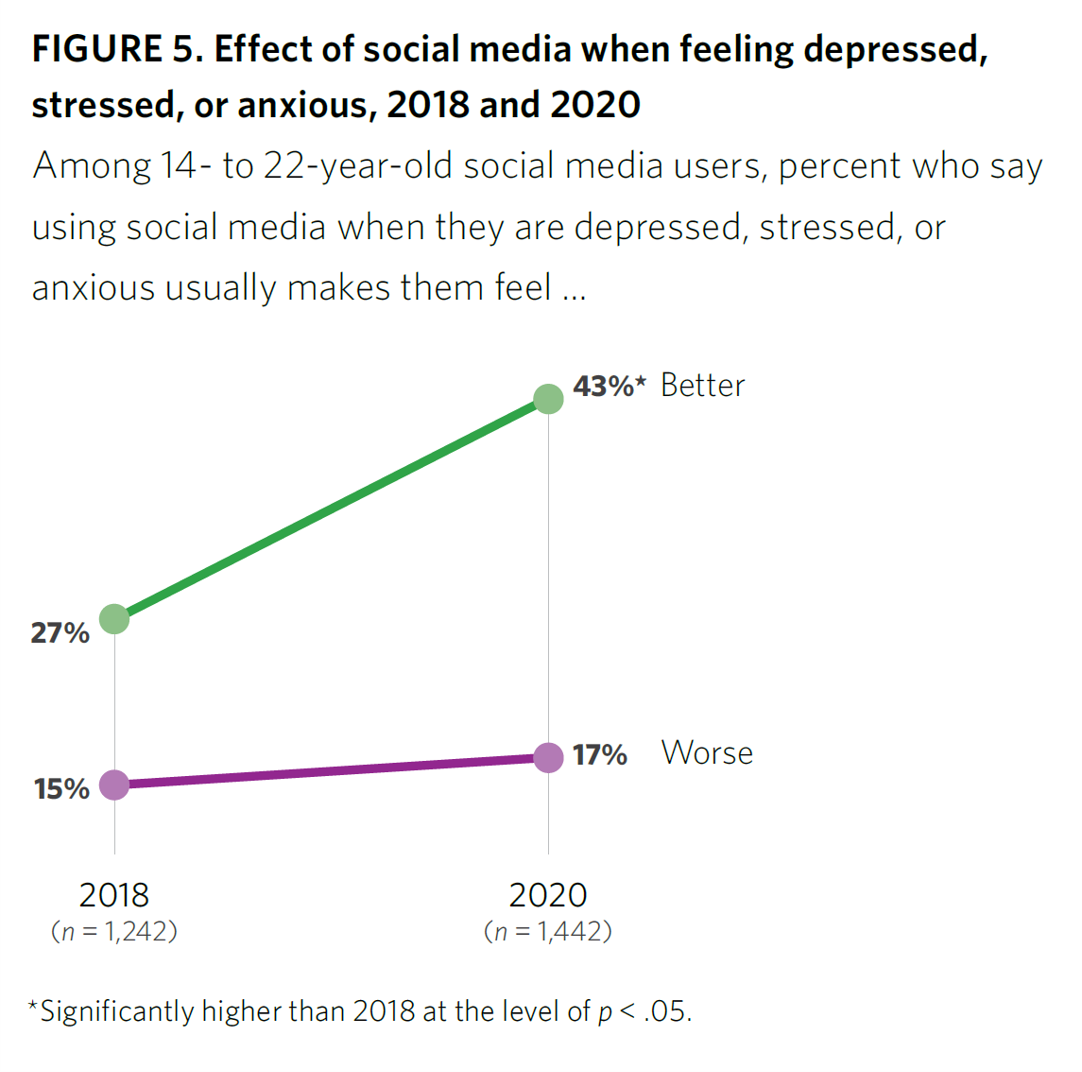
After a year of living with and “in” the coronavirus pandemic, younger people in the U.S. have had to deal with over twelve months of quarantine and lockdown, going to school remotely from home, and distancing from friends. For most young people, the public health crisis has been more about that social distancing from friends, a collective sense of isolation, and mental and behavioral health impacts. These dynamics and these young health citizens’ coping mechanisms are captured in the report, Coping with COVID-19: How Young People Use Digital Media to Manage Their Mental Health. Three organizations collaborated to conduct and
The Ongoing Reality of COVID-19 – My Conversation with Dr. Michael Osterholm at SXSW
“So close and yet so far” feels like the right phrase to use a year after the World Health Organization used the “P-word,” “pandemic,” to describe the coronavirus’s impact on public health, globally. One year and over 550,000 COVID-related deaths in the U.S. later, we face a New Reality that Dr. Michael Osterholm and I are brainstorming today at the 2021 South-by-Southwest Festival. Usually held live and very up-close-and-personally crowded in Austin, Texas, this year we are all virtual — including the film, music, and interactive festivals alike. While I regret to not be in the same room as Dr.
How to Restore Americans’ Confidence in U.S. Health Care: Deal With Access and Cost
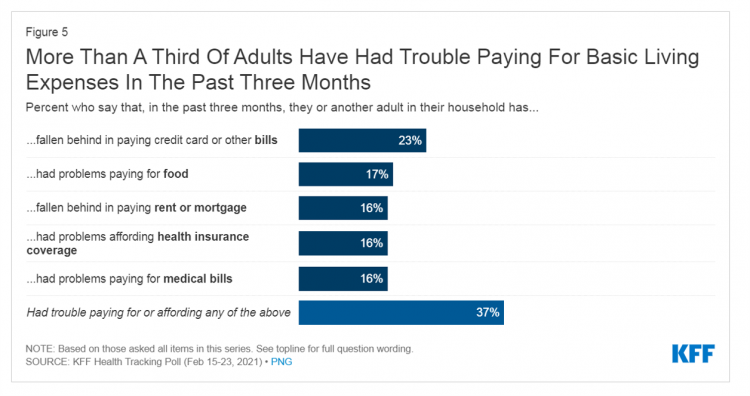
With a vaccine supply proliferating in the U.S. and more health citizens getting their first jabs, there’s growing optimism in America looking to the next-normal by, perhaps, July 4th holiday weekend as President Biden reads the pandemic tea leaves. But that won’t mean Americans will be ready to return to pre-pandemic health care visits to hospital and doctor’s offices. Now that hygiene protocols are well-established in health care providers’ settings, at least two other major consumer barriers to seeking care must be addressed: cost and access. The latest (March 2021) Kaiser Family Foundation Tracking Poll learned that at least one
Value-Based Health Care Needs All Stakeholders at the Table – Especially the Patient

2021 is the 20th anniversary of the University of Michigan Center for Value-Based Insurance Design (V-BID). On March 10th, V-BID held its annual Summit, celebrating the Center’s 20 years of innovation and scholarship. The Center is led by Dr. Mark Fendrick, and has an active and innovative advisory board. [Note: I may be biased as a University of Michigan graduate of both the School of Public Health and Rackham School of Graduate Studies in Economics]. Some of the most important areas of the Center’s impact include initiatives addressing low-value care, waste in U.S. health care, patient assistance programs, Medicare
The Most Relevant Companies in Health Care – Learning from the W2O Group
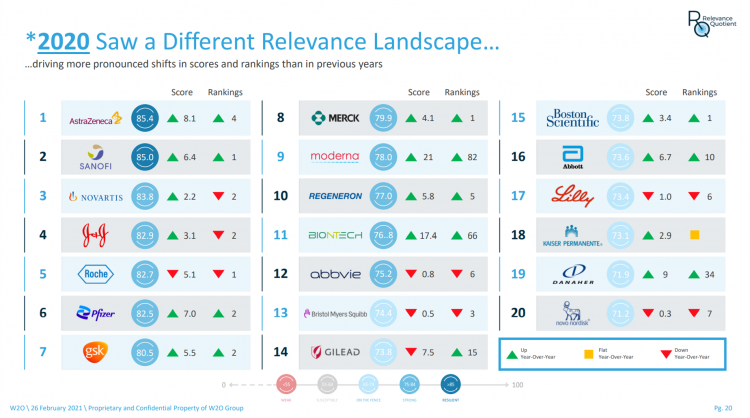
Five years ago, in 2016, the W2O Group said that, “Relevance is reputation.” That year the firm began to study the relevance of, well, relevance for organizations especially operating in the health/care ecosystem. 2020 changed everything, the W2O team asserts, now issuing its latest look into the issue through the Relevance Quotient. Relevance is built on recognizing, meeting and exceeding stakeholder expectations of organizations. In the Relevance Quotient methodology, W2O Group defines key stakeholders as employees, patients (including the sick and the well, caregivers, consumers, et al), health care providers, advocacy groups, analysts and investors, policy makers, journalists and media outlets.
Ten In Ten: Manatt’s Healthcare Priorities to 2031

The coronavirus pandemic has exposed major weaknesses in the U.S. health care system, especially laying bare inequities and inertia in American health care, explained in The Progress We Need: Ten Health Care Imperatives for the Decade Ahead from Manatt Health. The report details the ten objectives that are central to Manatt’s health care practice, a sort of team manifesto call-to-action and North Star for the next decade. Their ten must-do’s for bending the cost curve while driving constructive change for a better health care system are to: Ensure access Achieve health equity Stability the safety net and rebuild public health
Can Telemedicine Increase Health Equity? A Conversation with Antoinette Thomas, Dave Ryan, and Me with the ATA

“Yes,” we concurred on our session convened by the American Telemedicine Association (ATA) EDGE session today. “We” was a trio including Antoinette Thomas (@NurseTechExec1), Chief Patient Experience Officer with Microsoft, David Ryan (@DavidPRyan), former long-time Global Head of Intel’s Health/Life Science business; and, me. Antoinette posed three questions for all of us to brainstorm, addressing various aspects of health equity. We covered, The theory that telemedicine should increase health equity — where are we and what are the barriers to getting there? The role of social determinants of health in creating equitable opportunities for health citizens; and, Entering a post-pandemic world,
Food Trends and Hunger in the Pandemic – the Importance of Food Security in Health and Economic Security
In 2020, the COVID-19 pandemic changed all kinds of aspects of our daily lives, not the least of which were our food habits — how we shopped for food, how we bought food, how we cooked and baked from scratch, and how our tastes and nutritional choices changed with our #StayHome and #WorkFromHome lifestyles. People who could keep their jobs and work from home connected by broadband learned how to build up pandemic pantries, shop online, and stay well-fed. But for people in the U.S. who lost employment, had hours cut, or were compelled to stay home to teach kids
Addressing Lives and Livelihoods with a Whole-of-Government Approach – The First Wave of Biden Health Policy
President Biden’s first few days on the job gave us a very clear view on how he sees conquering COVID: through a whole-of-government approach to public policies that bolster directly addressing the virus, along with the many forces shaping how we got here and how to come out of the pandemic era stronger. I cover this first wave of Biden health policy in my latest post for the Medecision Liberation blog titled, “Top Priorities for President Biden: COVID-19, Then Everything Else.” The plotline goes… On the day of inauguration, January 20, 2021, Joseph R. Biden was installed as the 46th
The Biden Administration’s Whole-of-Government Approach to Equity – in Health and Beyond
In the U.S., the COVID-19 pandemic has revealed disparities in housing, food, and job security, and the role that one’s ZIP code and social determinants play in health outcomes. Overall, America has done poorly in light of being 4% of the world’s population but having one-fifth of the planet’s deaths due to the coronavirus. But these have disproportionately hit non-white people, who are nearly three times as likely to die from COVID-19 than white Americans. I’ve been head-down reviewing the first two days of President Biden’s signing Executive Orders, reading the National Strategy for COVID-19 Response, and inventorying line items
Our Homes Are Health Delivery Platforms – The New Home Health/Care at CES 2021

The coronavirus pandemic disrupted and re-shaped the annual CES across so many respects — the meeting of thousands making up the global consumer tech community “met” virtually, both keynote and education sessions were pre-recorded, and the lovely serendipity of learning and meeting new concepts and contacts wasn’t so straightforward. But for those of us working with and innovating solutions for health and health care, #CES2021 was baked with health goodness, in and beyond “digital health” categories. In my consumer-facing health care work, I’ve adopted the mantra that our homes are our health hubs. Reflecting on my many conversations during CES
Vaccine Hesitancy Is Greatest Among Those at Highest Risk of Dying from COVID-19: Black People
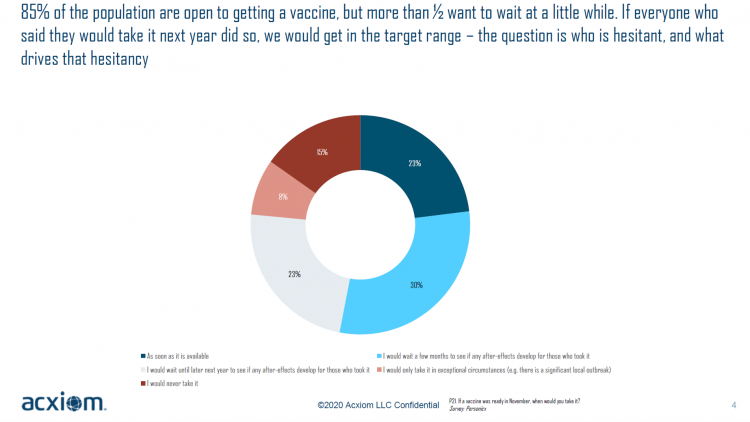
While 85% of people are open to receiving a COVID-19 vaccine, over one-half of them would want to wait some time to observe if after-effects developed in people who took the jab, according to a new study from Acxiom, the data analytics-marketing company. Not all people are as enthused about getting a coronavirus vaccine at all, Acxiom discovered: in fact, those hardest hit by the virus — Black people — would be the least-likely to want to get a COVID-19 vaccine, discussed in in Vaccine Hesitancy in the U.S., a survey the company conducted among 10,000 people in the U.S.
Voting for Health in 2020

In the 2018 mid-term elections, U.S. voters were driven to polls with health care on their minds. The key issues for health care voters were costs (for care and prescription drugs) and access (read: protecting pre-existing conditions and expanding Medicaid). Issue #2 for 2018 voters was the economy. In 2020, as voting commences in-person tomorrow on 3rd November, U.S. voters have lives and livelihoods on their minds. It’s the pandemic – our physical lives looming largest in the polls – coupled with our fiscal and financial lives. Health is translating across all definitions for U.S. voters in November 2020: for
Redefining PPE As Primary Care, Public Health, and Health Equity – The Community PPE Index
In May 2020, the Oxford English Dictionary (OED) re-visited the acronym, “PPE.” As OED evolves the definition of PPE, the wordsmiths could borrow from OSHA’s website, noting that PPE, “is equipment worn to minimize exposure to hazards that cause serious workplace injuries and illnesses. These injuries and illnesses may result from contact with chemical, radiological, physical, electrical, mechanical, or other workplace hazards. Personal protective equipment may include items such as gloves, safety glasses and shoes, earplugs or muffs, hard hats, respirators, or coveralls, vests and full body suits.” Perhaps Definition 3 in the OED could be updated by a blog
Behavioral Health Side-Effects in the COVID Era
“This surge of people experiencing acute behavioral health problems…has the potential to further impact the healthcare system for years to come,” a report from McKinsey expects looking at the hidden costs of COVID-19’s impact on U.S. health care. The coronavirus pandemic has taken a toll on Americans’ mental health, with anxiety and depression growing as a side-effect to worries about the virus itself, the long Great Lockdown in much of the country, and the economic recession that has particularly impacted women and people of color. I covered depression impacts due to COVID-19 here in Health Populi yesterday, and wanted to
The Unbearable Heaviness of Healthcare in America – the Change Healthcare/Harris Poll
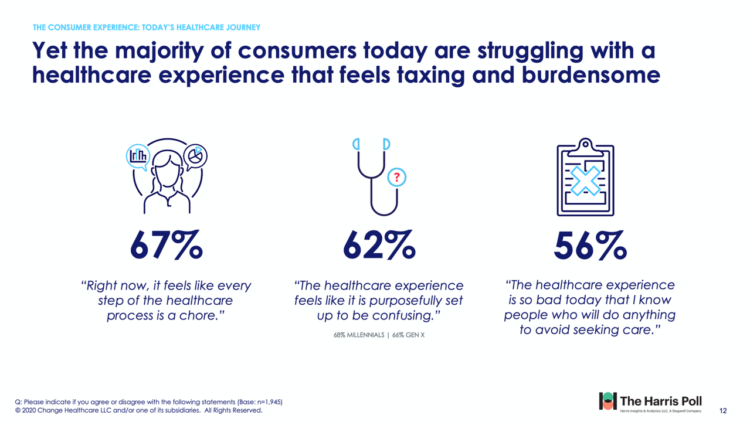
The phrase, “burden of health care,” has two usual meanings: one, to do with the massive chronic care burden, and the other, involving costs. There’s a third area of burden in U.S. health care — the onerous patient experience in finding and accessing care, assessed in the 2020 Change Healthcare – Harris Poll Consumer Experience Index. Two in three U.S. consumers feel like “every step of the healthcare process is a chore.” That burdensome patient experience leads to one in two people in America avoiding seeking care, the poll found. That’s not just self-rationing health care due to costs, but due
Return-To-School Is Stressing Out U.S. Parents Across Income, Race and Political Party
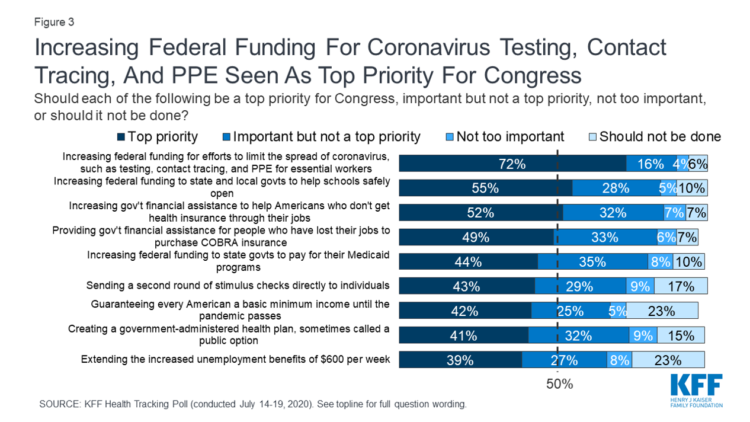
The worse of the coronavirus pandemic is yet to come, most Americans felt in July 2020. That foreboding feeling is shaping U.S. parents’ concerns about their children returning to school, with the calendar just weeks away from educators opening their classrooms to students, from kindergarten to the oldest cohort entering senior year of high school. The Kaiser Family Foundation’s July 2020 Health Tracking Poll focuses on the COVID-19 pandemic, return-to-school, and the governments’ response. KFF polled 1,313 U.S. adults 18 and older between July 14 to 19, 2020. The first line chart illustrates Americans’ growing concerns about the coronavirus, shifting
The Median Hospital Charge In the U.S. for COVID-19 Care Ranges From $34-45K
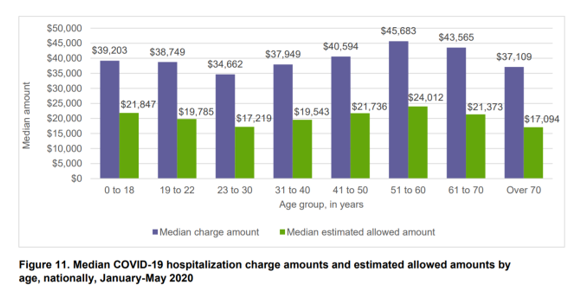
The median charge for hospitalizing a patient with COVID-19 ranged from $34,662 for people 23 to 30, and $45,683 for people between 51 and 60 years of age, according to FAIR Health’s research brief, Key Characteristics of COVID-19 Patients published July 14th, 2020. FAIR Health based these numbers on private insurance claims associated with COVID-19 diagnoses, evaluating patient demographics (age, gender, geography), hospital charges and estimated allowed amounts, and patient comorbidities. They used two ICD-10-CM diagnostic codes for this research: U07.1, 2019-nCoV acute respiratory disease; and, B97.29, other coronavirus as the cause of disease classified elsewhere which was the original code
Juneteenth 2020: Inequality and Injustice in Health Care in America
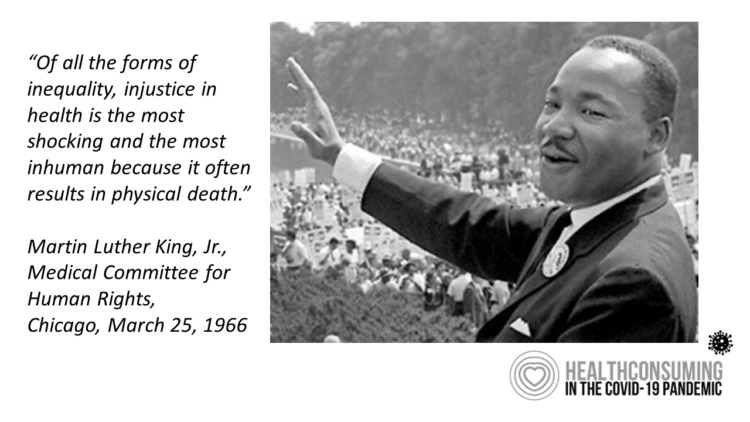
“Of all the forms of inequality, injustice in health is the most shocking and the most inhuman because it often results in physical death,” Martin Luther King, Jr., asserted at the second meeting of the Medical Committee for Human Rights in Chicago on March 25, 1966. This quote has been shortened over the five+ decades since Dr. King told this truth, to the short-hand, “Of all the forms of inequality, injustice in health care is the most shocking and inhumane.” Professor Charlene Galarneau recently enlightened me on Dr. King’s original statement in her seminal essay, “Getting King’s Words Right.” Among
Addressing Health Equity Must Include Digital Equity Beyond Access To Medical Services and Insurance
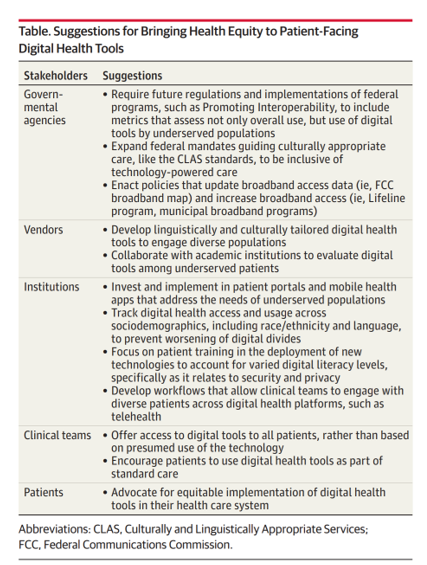
The 21st Century Cures Act emphasizes patients’ control of personal health information. ONC rules issues in March 2020 called for more patient-facing health tools and apps to bolster health consumer engagement and empowerment. But the emergence of the coronavirus in the U.S. revealed many weakness in the American health care system, one of which has been health inequities faced by millions of people — especially black Americans, who have sustained higher rates morbidity and mortality for COVID-19. There have also been digital health divides found in the COVID-19 pandemic, discussed in a timely essay in JAMA, Digital Health Equity as
Financial Insecurity Among U.S. Workers Will Worsen in the Pandemic — Especially for Women
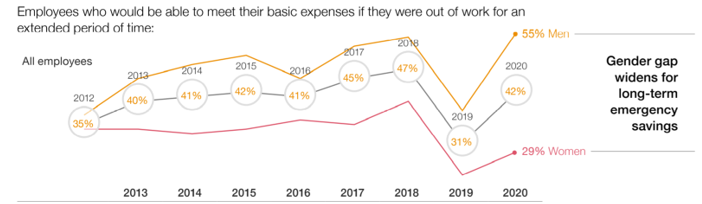
Millions of mainstream, Main Street Americans entered 2020 feeling income inequality and financial insecurity in the U.S. The coronavirus pandemic is exacerbating financial stress in America, hitting women especially hard, based on PwC’s 9th annual Employee Financial Wellness Survey COVID-19 Update. For this report, PwC polled 1,683 full-time employed adults between 18 and 75 years of age in January 2020. While the survey was conducted just as the pandemic began to emerge in the U.S., PwC believes, “the areas of concern back in January will only be more pronounced today,” reflecting, “the realities of the changing employee circumstances we are
The Book on Deaths of Despair – Deaton & Case On Education, Pain, Work and the Future of Capitalism
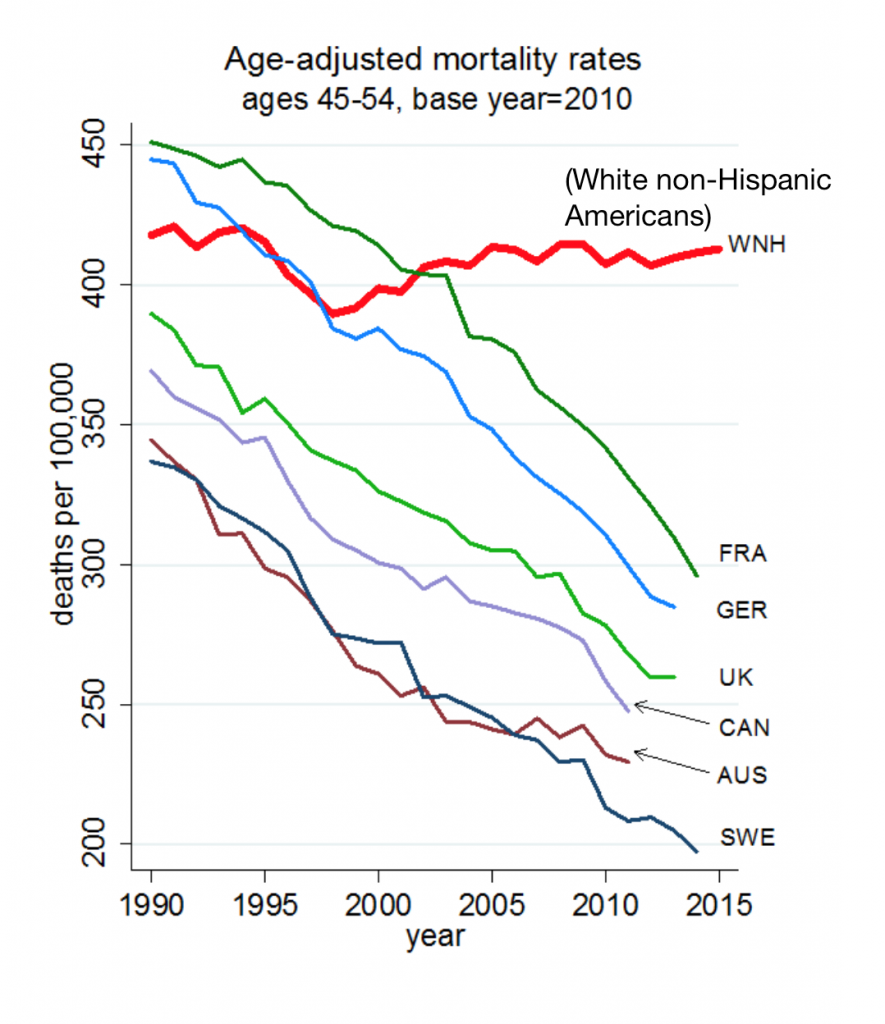
Anne Case and Angus Deaton were working in a cabin in Montana the summer of 2014. Upon analyzing mortality data from the U.S. Centers for Disease Control, they noticed that death rates were rising among middle-aged white people. “We must have hit a wrong key,” they note in the introduction of their book, Deaths of Despair and the Future of Capitalism. This reversal of life span in America ran counter to a decades-long trend of lower mortality in the U.S., a 20th century accomplishment, Case and Deaton recount. In the 300 pages that follow, the researchers deeply dive into and
Longevity Stalls Around the World And Wealth, More Concentrated

Two separate and new OECD reports, updating health and the global economic outlook, raise two issues that are inter-related: that gains in longevity are stalling, with chronic illnesses and mental ill health affecting more people; and, as wealth grows more concentrated among the wealthy, the economic outlook around most of the world is also slowing. First, we’ll mine the Health at a Glance 2019 annual report covering data on population health, health system performance, and medical spending across OECD countries. The first chart arrays the x-y data points of life expectancy versus health spending for each of the OECD countries
Social Determinants of Health – My Early Childhood Education and Recent Learnings, Shared at the HealthXL Global Gathering
My cousin Arlene got married in Detroit at the classic Book Cadillac Hotel on July 23, 1967, a Sunday afternoon wedding. When Daddy drove us back out to our suburban home about 30 minutes from the fancy hotel, the car radio was tuned to WWJ Newsradio 950, all news all the time. As soon as Daddy switched on the radio, we were shocked by the news of a riot breaking out in the city, fires and looting and gunshots and chaos in the Motor City. Two days later, my father, who did business with Mom-and-Pop retail store owners in the
Art As Medicine – WHO Weaves the Evidence for Arts’ Role in Improving Health

“What’s the evidence on the role of the arts in improving health and well-being?” asks a report from the World Health Organization‘s Europe region team (WHO-Europe). There’s a lot of proof supporting arts-as-medicine, WHO details in this paper, which synthesizes research published in over 3,000 studies. The first chart illustrates the logic model that bridges arts to health in three segments: “Components” of arts programs, including but not limited to cognitive stimulation (e.g., learning a new arts skill such as painting, drawing or journaling), social interaction (e.g., participating in theatre), physical activity (e.g., dance), and evocation of emotion (e.g., listening
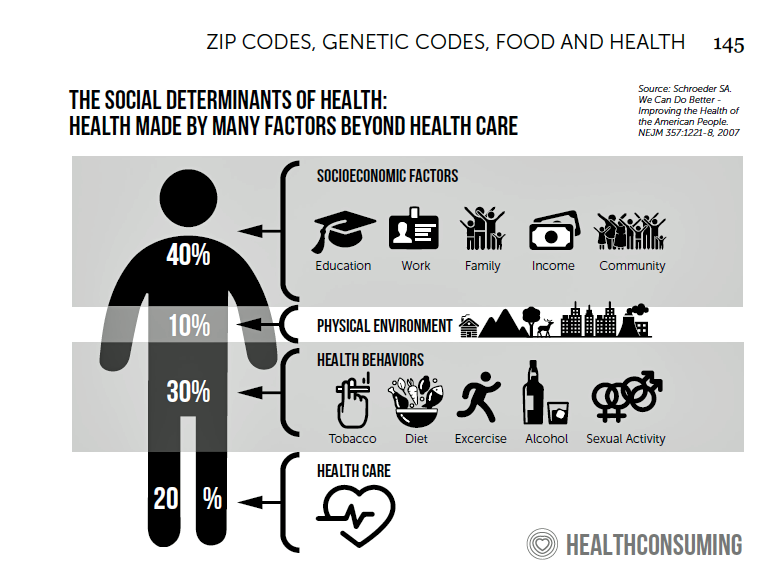
The Rise of Social Determinants of Health in Healthcare is Just Real Life Stuff for People, Patients, Consumers

Based on the influx of research studies and position papers on social determinants of health flowing into my email box and Google Alerts, I can say we’re past the inflection point where SDoH is embraced by hospitals, professional societies, health plans and even a couple of pioneering pharma companies. PwC published a well-researched global-reaching report this week appropriately titled, Action required: The urgency of addressing social determinants of health. The “wheel of determinants” illustrates potential partners for collaborating in communities to address SDoH factors. The collaborators include governments, health care providers, payors, life science and pharma, tech and telecomms, policy
Prelude to Health 2.0 2019: Thinking Consumers At the Center of Digital Health Transformation

“Digital transformation” is the corporate strategy flavor of the moment across industries, and the health are sector isn’t immune from the trend. As this 13th year of the annual Health 2.0 Conference kicks off this week, I’m focused on finding digital health innovations that engage people — consumers, caregivers, patients, health citizens all. This year’s conference will convene thought leaders across a range of themes, and as is the Health 2.0 modus operandi, live demo’s of new-new things. As Health 2.0 kicks off today in pre-conference sessions, there is useful context described in a new report from the American Hospital
100 Million People in America Lack Broadband — an On-Ramp to Health and Safety

One in three Americans does not have a broadband connection, according to a new report from the NPD Group. This means that about 100 million people in the U.S. can’t benefit from telehealth and other digital health connections that can bolster self-care, home care, and lower cost care. Most of these folks in the broadband-digital divide live in rural America/ “The so-called digital divide, between those that can or cannot make the best use of the Internet, can be clearly felt in rural markets where the lack of broadband impacts everything from entertainment to the educational system,” Eddie Hold, President
Gaps in Health Equity in America Are Growing

There’s been a “clear lack of progress on health equity during the past 25 years in the United States,” asserts a data-rich analysis of trends conducted by two professors/researchers from UCLA’s School of Public Health. The study was published this week in JAMA Network Open. The research mashed up several measures of health equity covering the 25 years from 1993 through 2017. The data came out of the Centers for Disease Control and Prevention’s Behavioral Risk Factor Surveillance System looking at trends by race/ethnicity, sex and income across three categories for U.S. adults between 18 and 64 years of age.
Are Robots Coming to Healthcare? Consumers Say Not-So-Fast

Samsung introduced BotCare, a caring robot, at CES 2019. BotCare is part of the company’s Bixby, an AI platform that supports Samsung’s robotic offerings for environmental health (air), retail, and healthcare. Think: medication reminders and around-the-house services that a human homecare aid might perform, among other medical support tasks. But visions of Rosie-the-Robot serving up healthcare at home is beyond most consumers’ desires at this moment, according to a new survey published by the Consumer Technology Association (CTA), Robotics: Current Landscape & Consumer Perceptions. Most U.S. adults have positive views toward robotics in general, CTA found. There’s optimism for use
Scaling the Social Determinants of Health – McKinsey and Kaiser’s Bold Move

People who are in poor health or use more health care services are more likely to report multiple unmet social needs, such as food insecurity, unsafe neighborhoods, lack of good housing, social isolation, and poor transportation access, found through a survey conducted by McKinsey. The results are summarized in Addressing the Social Determinants of Health. The growing recognition of the influence of social determinants reached a tipping point last week with the news that Kaiser-Permanente would work with Unite US to scale services to people who need them. The mainstreaming of SDoH speaks to the awareness that health is made
Radicalizing Kindness for Health: Learning from Bhutan

“Happiness is within, but not within you alone as it is among us. If we can create happiness in a community, then we will be able to attain happiness as individuals,” observed Saamdu Chetri speaking at the International Psychological Congress last week. Chetri is head of Bhutan’s Gross National Happiness Centre, which developed the Gross National Happiness Index. The phrase “Gross National Happiness” was first mentioned in 1972 by the 4th King of Bhutan, King Jigme Singye Wangchuck in an interview with the Financial Times. King Wangchuck said that, “Gross National Happiness is more important than Gross Domestic Product.” The GNH
Design, Empathy and Ethics Come to Healthcare: HXD

Design-thinking has come to health/care, finally, and Amy Cueva has been beating this drum for a very long time. I’m delighted to be in her collegial circle, speaking at the conference about the evolving healthcare consumer who’s financially strapped, stressed-out, and Amazon Primed for customer service. I’m blogging live while attending HXD 2018 in Cambridge, MA, the health/care design conference convened by Mad*Pow, 26th and 27th June 2018. Today was Day 1 and I want to recap my learnings and share with you. Amy, Founder and Chief Experience Office of Mad*Pow, kicked off the conference with context-setting and inspiration. Design
Pope Francis is a Public Health Advocate

“The world today is mostly deaf,” the Pontiff observes in Pope Francis: A Man of His Word, Wim Wenders’ documentary on this religious leader who likes to quote Dostoevsky, joke about mothers-in-law, and advocate for the sick, the poor, the disenfranchised, and Planet Earth. He is, I realized while watching this film and hearing this man of words, a public health advocate. Throughout the film, we see clips of Pope Francis washing the feet of prisoners in Philadelphia, comforting dying children in a pediatric clinic in central Africa, and speaking out to the U.S. Congress about the dangers of climate
The Health of A Nation – Being Healthy In America Depends on Where You Live

In the US, when it comes to life and death, it’s good to live in Hawaii, Utah, Minnesota, North Dakota, and Iowa — the top five states with the greatest life expectancy and healthy life expectancy at birth in 2016. For health and longevity, sorry to see the lowest five ranked states are Washington DC which ranks last, along with Mississippi, Louisiana, South Carolina, and Alabama. This sober geography-is-health-destiny update was published this week in JAMA, The State of US Health, 1990-2016: Burden of Diseases, Injuries, and Risk Factors Among US States. The first chart illustrates states down the left
Will People Enrolled in Medicaid Want to Be Amazon Prime’d?

Amazon is planning to extend Prime subscriptions to people enrolled in Medicaid for the discount price of $5.99 a month instead of the recent price increase to $12.99/month or $99 a year. The $5.99 a month calculates to a 27% break on the annual Prime membership cost. Medicaid enrollees who want to take advantage of the deal must provide Amazon with a scan or image of the card they use for their benefit (either Medicaid or EBT). These consumers can enroll annually, for a maximum of four years. Here’s what the Seattle Times, Amazon’s hometown newspaper, said about the program.
Tweets at Lunch with Paul Krugman – Health IT Meets Economics

I greatly appreciated the opportunity today to attend a luncheon at the HX360 meeting which convened as part of the 2018 HIMSS Conference. The speaker at this event was Paul Krugman, who won the Nobel Prize for Economics 10 years ago and today is an iconic op-ed columnist at the New York Times And Distinguished Professor of Economics at the City University of New York (CUNY). I admit to being a bit of a groupie for Paul Krugman’s work. It tickles me to look at Rise Global’s list of the Top 100 Influential Economists:
The $4 Trillion Health Economy of 2020
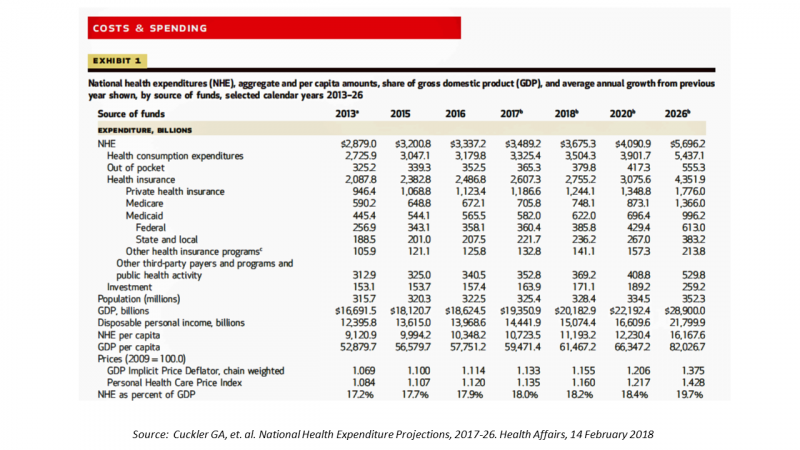
In 2020, national health expenditures (NHE) in the United States will exceed $4 trillion to cover 334.5 million Americans. That equates to 18.4% of the Gross Domestic Product (GDP) and $12,230.40 of health spending per person. I sat in on a press call today with researchers from the Office of the Actuary working in the Centers for Medicare and Medicaid Services (CMS) to review the annual forecast of the NHE, published in Health Affairs in a statistically-dense eleven page article titled, National Health Expenditure Projections, 2017-2026: Despite Uncertainty, Fundamentals Primarily Drive Spending Growth. What are those “fundamentals” pushing up healthcare spending?
Six Healthcare News Stories to Keep Hospital CFOs Up At Night
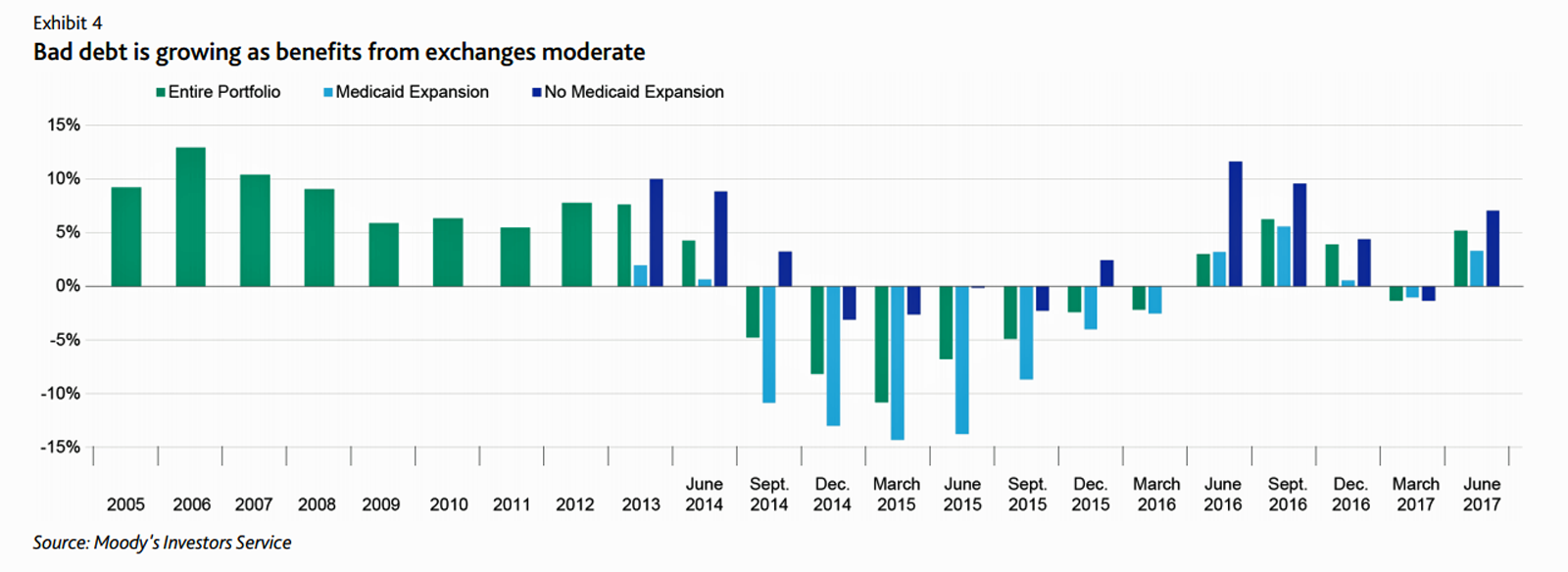
At this moment, the healthcare job I’d least like to have is that of a non-profit hospital Chief Financial Officer (CFO). Five news stories, published in the past 24 hours, tell the tale: First, Moody’s forecast for non-profit hospitals and healthcare in 2018 is negative due to reimbursement and expense pressures. The investors report cited an expected contraction in cash flow, lower reimbursement rates, and rising expense pressures in the midst of rising bad debt. Second, three-quarters of Federally Qualified Health Centers plan to lay off staff given lack of budget allocations resulting from Congressional inaction. Furthermore, if the $3.6
Most Consumers Would Trust a Health Info Site “Prescribed” by Their Doctor
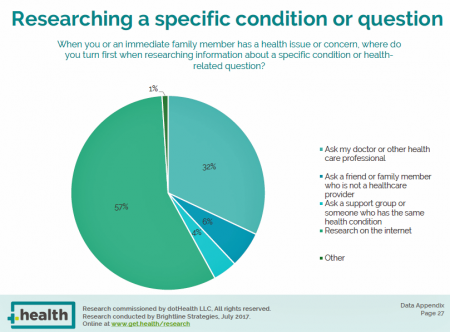
Most consumers access the Internet for health information before they ask their doctor for the same information. But virtually everyone who goes online for health information would trust a website recommended to them by their doctor, according to the dotHealth Consumer Health Online – 2017 Research Report. This survey was conducted on behalf of dotHealth, an internet registry company channeling “.health” domains to organizations in the broad health and healthcare landscape. [FYI, both Health Populi and JaneSarasohnKahn are also registered with .health domains, having availed ourselves of this service at launch]. Six in 10 consumers who have used the internet in the
Most Americans, Including Republicans, Want President Trump’s Administration to Make the ACA Work – Not Fail
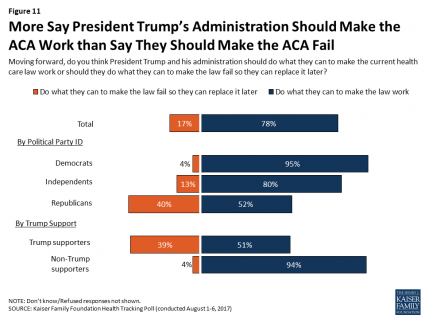
8 in 10 Americans want President Trump and his administration to do what they can to make the Affordable Care Act work, according to the latest August 2017 health tracking poll from Kaiser Family Foundation (KFF). By political party affiliation, this includes 95% of Democrats, 80% of Independents, and 52% of Republicans (that is, to emphasize the point, just over half, a majority, of Republicans). More Americans are also relieved and happy, versus disappointed and angry, that the ACA repeal did not occur (thus far), the second chart illustrates. To be sure, a majority of Republicans register anger and disappointment,
Note to Mooch: The ER is Not Universal Health Care
I quote directly from the Twitter feed of Anthony Scaramucci, @scaramucci: “@dhank2525 agree. We already have Univ Health Care, we made decision long ago to treat everyone that enters an emergency room.” Mr. Scaramucci is President Trump’s Communications Chief, replacing Sean Spicer. Mr. Scaramucci is neither veteran journalist nor healthcare policy wonk. He’s a successful businessman, which I respect for his savvy and ability to build a fund, attract investors, and create a media persona which he has telegenically broadcast on CNBC and elsewhere over the past decade. He’s got a engaging public personality, and goes by the moniker, “Mooch.” But
The Pursuit of Health Equity and the State of U.S. Health Care
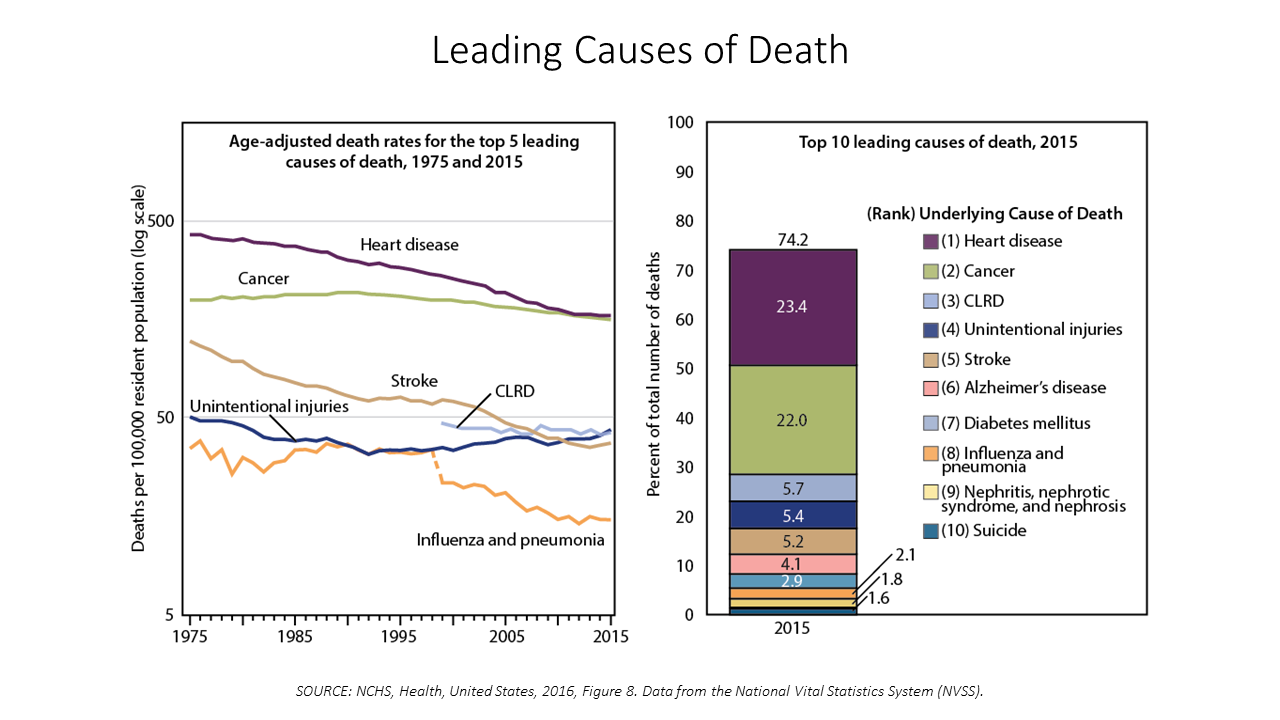
Between 2014 and 2015, death rates increased for eight of the ten leading causes; only death rates caused by cancer fell, and mortality rates for influenza and pneumonia stayed flat. The first chart paints this sobering portrait of Americans’ health outcomes, presented in the CDC’s data-rich 488-page primer, Health, United States, 2016. Think of this publication as America’s annual report on health. Every year, it is prepared and submitted to the President and Congress by the Secretary of the Department of Health and Human Services. This year’s report was delivered by DHHS Secretary Tom Price to President Trump and the
Shopping Food for Health: the 2017 U.S. Grocery Shopper Trends
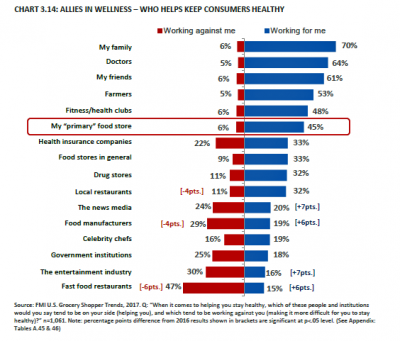
Wellness is at the grocery store, the vast majority of U.S. health citizens say. 8 in 10 U.S. shoppers are concerned about the nutritional content in the food they eat. As grocery shoppers look for more fresh and less processed foods, grocery stores are seen as trusted allies for meeting wellness needs. Grocers are coupling the growth of more healthy packaged foods in the middle of the store with more fresh and prepared food options that consumers see as healthier than restaurant meals, according to U.S. Grocery Shopper Trends 2017 from FMI (the Food Marketing Institute) and Hartman Group. While
The Power of Joy in Health and Medicine – Learning From Dr. Regina Benjamin

Former Surgeon General Dr. Regina Benjamin was the first person who quoted to me, “Health isn’t in the doctor’s office. It’s where people live, work, play and pray,” imparting that transformational mantra to me in her 2011 interview with the Los Angeles Times. I wrote about that lightbulb moment here in Health Populi. Dr. Benjamin was the 18th Surgeon General, appointed by President Obama in 2009. As “America’s Doctor,” she served a four-year term, her mission focused on health disparities, prevention, rual health, and children’s health. Today, Dr. Benjamin wears many hats: she’s the Times Picayune/NOLA.com professor of medicine at
Valuing Children = Valuing Health: Learning From Florence, Italy

This week I celebrate two spring holy holidays in one city that embraces spirituality, civility, and culture: Florence, Italy. Today, I had the special opportunity to tour Ospedale degli Innocenti: the Hospital of the Innocents. The hospital is now an institute for studying the culture and economics of children, and a museum telling a unique story of Florentine babies born in the early 15th century, spanning our contemporary era. The founding and root history of this beautiful place has lessons to teach us even today. It is key to realize, first, that Florentine humanism exalted the ideal virtues of the
Americans Are Not Sold On the American Health Care Act
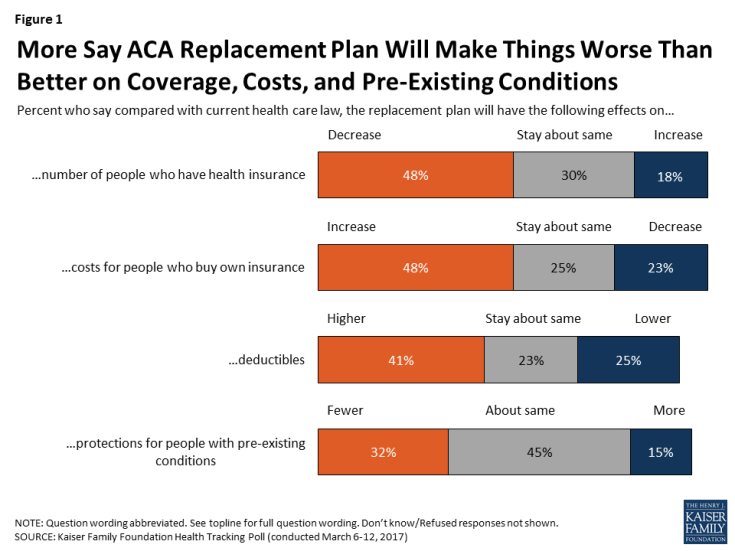
Most Americans do not believe that TrumpCare, the GOP plan to replace the Affordable Care Act (the ACA, aka ObamaCare), will make things better for U.S. health citizens when it comes to peoples’ health insurance coverage, the premium costs charged for those health plans, and protections for people with pre-existing medical conditions. The March 2017 Kaiser Family Foundation Health Tracking Poll examined U.S. adults’ initial perceptions of AHCA, the American Health Care Act, which is the GOP’s replacement plan for the ACA. There are deep partisan differences in perceptions about TrumpCare, with more Republicans favorable to the plan — although not
The Health Disparity of Information Access
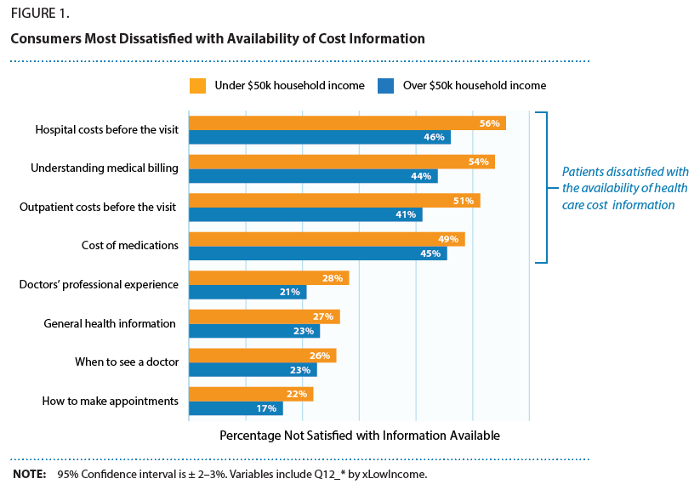
Among many health disparities which mar healthcare quality in the United States, there’s another one to add to the list: health and healthcare information access. Access to health care is underpinned in large part on a health consumer’s access to information about available health care services, their location, price, and if the patient is very fortunate to glean, quality. As people take on more responsibility for managing their health care utilization and financing in America, their access to information that is easy-to-find, clear, comprehensive and current is critical to personal and public health outcomes. But consumers are dissatisfied with the
The Digital Health Gap For High-Cost, High-Need Patients
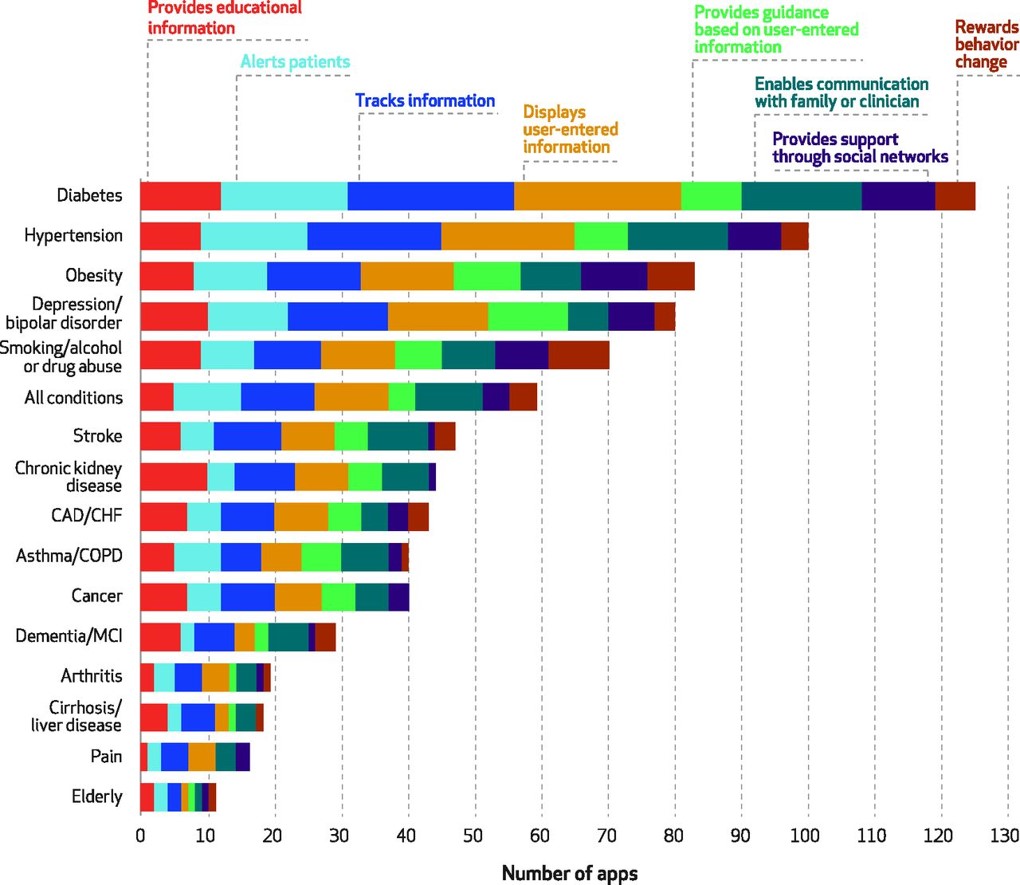
Several market forces are converging that boost patients’ ability to engage in their health and self-care, including peoples’ growing adoption of smartphones, demand for self-service and DIY lifestyles, and Americans’ growing responsibility as health consumers. Health consumers are using a growing array of self-health tools, enabled through digital technologies. However, these tools aren’t yet engaging some of the very people who need them the most: high-need, high-cost patients. Research into this situation is discussed in the December 2016 Health Affairs article, Many Mobile Heaath Apps Target High-Need, High-Cost Populations, But Gaps Remain, published in the December 2016 issue of Health Affairs. For
1 in 3 Americans Still Self-Rations Healthcare
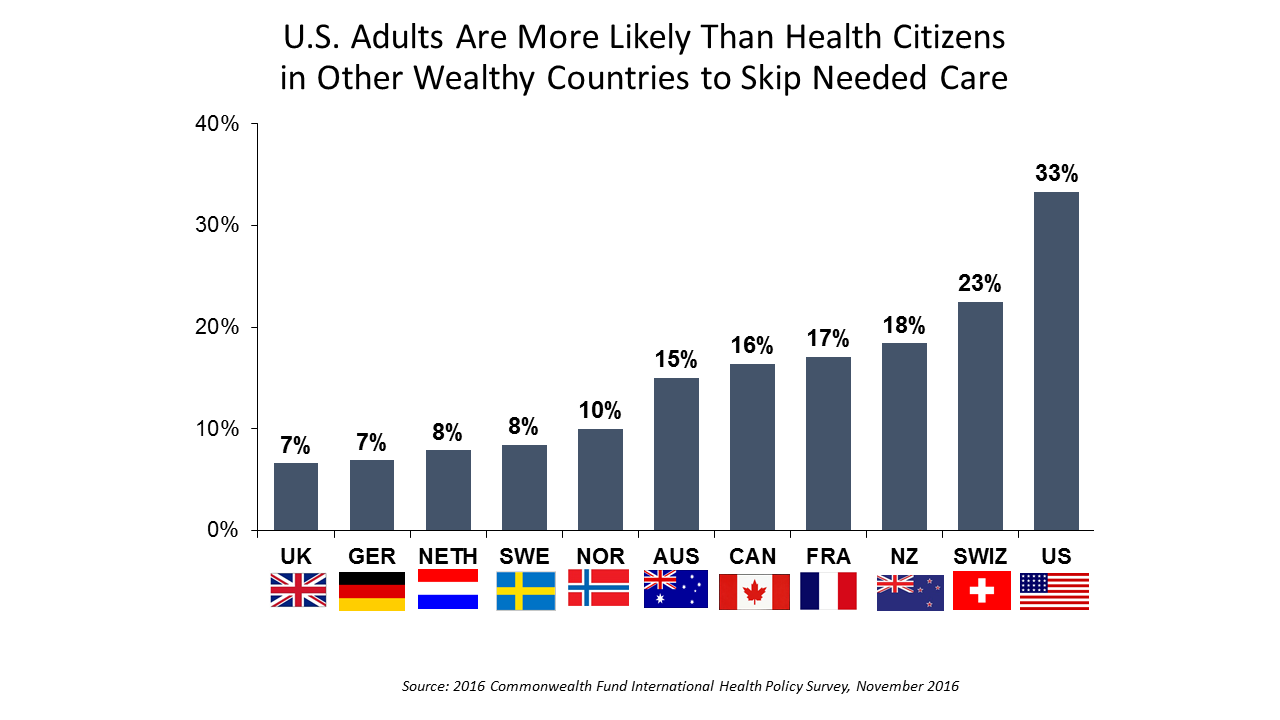
People in the U.S. are much more likely to go without health care they need compared with health citizens in 10 other wealthy countries, according to the Commonwealth Fund’s 2016 international survey. One-third of Americans did not seek care due to costs, including going without recommended care, failing to fill a prescription drug, and/or not seeing a doctor when sick. While this self-rationing proportion of Americans dropped from 37% in 2013, the U.S. still ranks #1 in foregoing necessary healthcare due to cost. “In comparison to adults in the other 10 countries, adult sin the U.S. are sicker and more
Naloxone in Retail Health – Helping The Opioid Epidemic at Pharmacies and Grocery Stores
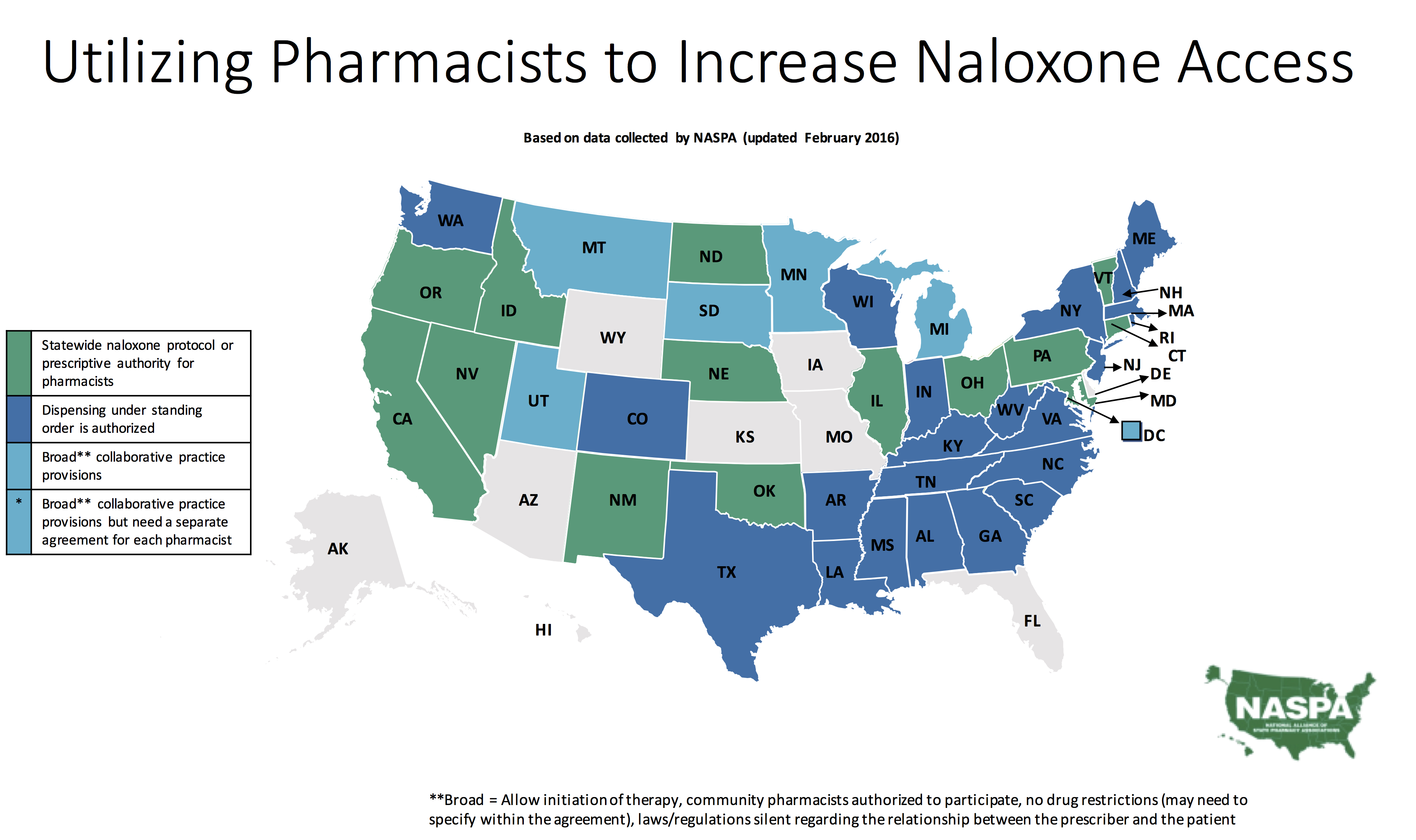
The ranks of pharmacies making available the overdose reversal medication naloxone without a prescription or seeing a doctor, is fast-growing. These announcements from retail pharmacy chains and grocery stores is a collective retail health-response to the opioid epidemic, a mainstream public health challenge across America. Naloxone is used in the event of an overdose. It can reverse the impacts of opioids, administered by injection or nasal spray. The statistics on opioid overdoses in the U.S. are chilling. Mortality (death rate) from opioid overdose in the U.S. grew 200% since 2000. Deaths have been higher among people between 25 and 44 years of
Health Care Reform: President Obama Pens Progress in JAMA
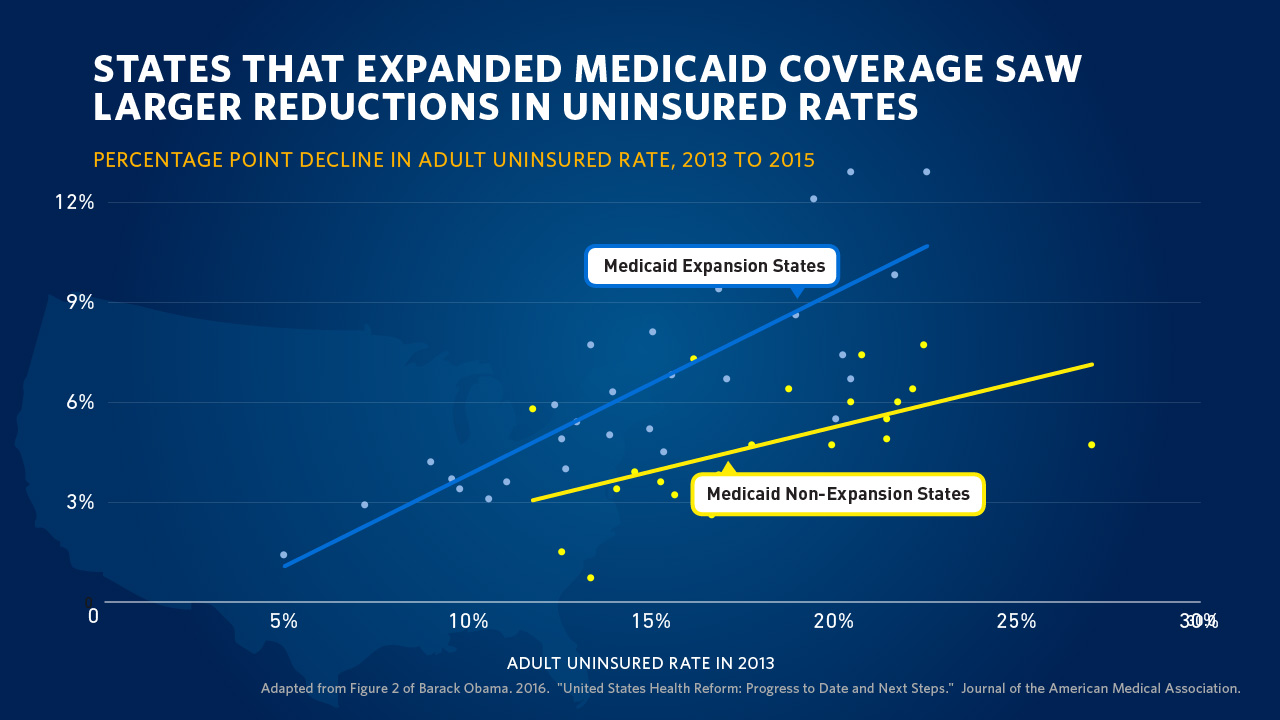
“Take Governor John Kasich’s explanation for expanding Medicaid: ‘For those that live in the shadows of life, those who are the least among us, I will not accept the fact that the most vulnerable in our state should be ignored. We can help them.’” So quotes President Barack Obama in the Journal of the American Medical Association, JAMA, in today’s online issue. #POTUS penned, United States Health Care Reform: Progress to Date and Next Steps. The author is named as “Barack Obama, JD,” a nod to the President’s legal credentials. Governor Kasich, a Republican, was one of 31 Governors who
The Health Disparities of Being Gay
#PrayForOrlando The club Pulse, site of the biggest mass gun shooting in U.S. history, was named to honor one of the co-owner’s brothers, who succumbed to AIDS in 1991. In today’s Health Populi, I soberly ponder the lost lives in the Orlando massacre of people who joyfully convened in a safe haven to celebrate life, liberty, and their pursuits of happiness. Over fifty people ended up dead, and there will be more mortalities as the health workers at Orlando Regional Medical Center continue to fight the post-trauma battle to save gunned-down lives. We define “health” broadly in Health Populi and
The New-New Health Fair – Care Goes Shopping

As consumers’ growing financial skin in the health care game compels them to seek care in lower-cost settings, the pharmacy business recognizes the opportunity to provide healthcare services beyond the core business of filling prescriptions. This month, Drug Store News (DSN) published a special section called which profiles several pharmacy companies’ expanding reach into retail health – in particular, re-defining the concept of the “health fair.” A health fair is “an educational and interactive event designed for outreach to provide basic prevention and medical screening to people in the community,” according to the latest Wikipedia definition. But the health fairs described
Building Health Bridges — Health:Further Goes Beyond the Disruptive

Most people in the U.S. acknowledge that their richest country in the world has a broken healthcare system, especially when it comes to costs. A handful of think tanks and lawmakers offer fixes for American healthcare. Now there’s a new problem-solver in healthcare town, Health:Further, and they aim to move U.S. health forward by building bridges between stakeholders in the U.S. health ecosystem. My longtime colleague and friend, Andre Blackman of Pulse+Signal, has joined the organization as “Producer.” Here, we’ll learn more from my (JSK) interview with Andre (AB) about the organization, their mission, and plans to go beyond “disruption”
Connectivity Is A Social Determinant of Health
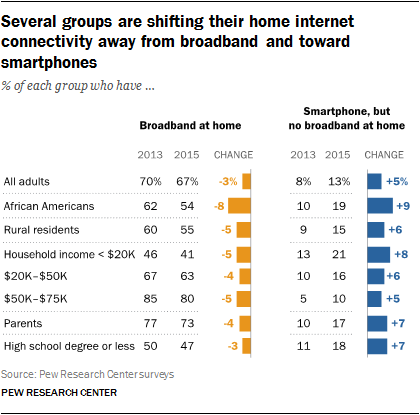
It’s Christmastime, so I’m thinking about connections. “Connectivity” can be social (offline and online), which is indeed a health factor (see Christakis and Fowler on being Connected). But the kind of connectivity to which I’m referring is broadband, WiFi, the kind most often associated with data plans, cable to the home, and free WiFi at your favorite coffee or fast food joint. That kind of connectivity is also a social determinant of health, and is increasingly becoming so for all people. Yet as peoples’ need for internet connectivity is fast growing, especially for health, home broadband connectivity has reached a
Retail Health Landscape Expanding Through Clinic Growth, Accenture Forecasts
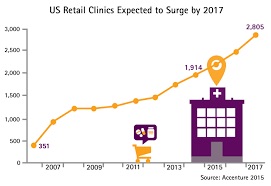
The Old School retail clinic is going beyond checking your child’s ear infection and sore throat, giving immunizations and filling out back-to-school forms just-in-time over LaborDay weekend. The new-new retail clinic is supporting patients’ chronic disease management, partnering with academic medical centers, and bolstering medication management. Accenture’s bullish forecast is titled “US Retail Health Clinics Expected to Surge by 2017,” making the case that these brick-and-mortar providers are shifting from a relatively limited retail scope to a broader and deeper clinical focus. The so-called surge in the number of retail clinics is projected to be nearly 50% growth between 2014 and 2017,
The rise and rise of noncommunicable diseases
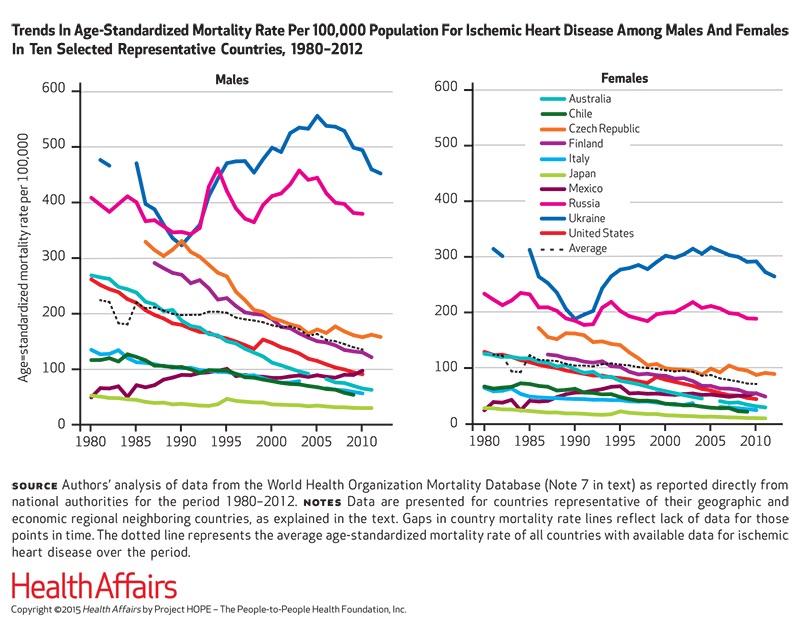
Noncommunicable diseases (NCDs) are the #1 cause of death in the world. NCDs are the yin to the yang of infectious diseases. Mortality from infectious disease has fallen as national economies have developed, while NCDs such as heart disease, respiratory disease, cancer, diabetes, and other NCDs are a growing burden. Health Affairs devotes its September 2015 issue to The Growing Burden of Noncommunicable Diseases, featuring research focusing both on global trends and U.S.-specific challenges. In their look into the relationships between NCDs, unhealthy lifestyles and country wealth, Thomas Bollyky et. al. note that NCDs aren’t only the “diseases of affluence,”
Health is where we live, work, and shop…at Walgreens
Alex Gourley, President of The Walgreen Company, addressed the capacity crowd at HIMSS15 in Chicago on 13th April 2015, saying his company’s goal is to “make good health easier.” Remember that HIMSS is the “Health Information and Management Systems Society” — in short, the mammoth health IT conference that this year has attracted over 41,000 health computerfolk from around the world. So what’s a nice pharmacy like you, Walgreens, doing in a Place like McCormick amidst 1,200+ health/tech vendors? If you believe that health is a product of lifstyle behaviors at least as much as health “care” services (what our
Stress Is US
“Reality is the leading cause of stress among those in touch with it,” Lily Tomlin once quipped. Perhaps in 2014, America is the land of stress because we’re all so in touch with reality. THINK: reality TV, social networks as the new confessional, news channeling 24×7, and a world of too much TMI. So no surprise, then, that one-half of the people in the U.S. have had a major stressful event or experience in the last year. And health tops the list of stressful events in This American Life in the forms of illness and disease (among 27% of people)
The business case for getting more social in health
While the U.S. spends more per person on health care than any other country in the world, we get a very low return on that investment. Other countries whose health citizens enjoy significantly better health outcomes spend less on health “care” (beds, technology, doctors’ salaries) and more per capita on social services and supports. There’s growing evidence that social factors impact health, and a business case to be made for spending more on social. The evidence and argument for providers spending more on social needs is explained in the research paper, Addressing Patients’ Social Needs: An Emerging Business Case for
Online is to go-to place for health insurance info, but lots of uninsured people live offline
A vast majority of people shopping for a health plan on a Health Insurance Exchange for coverage in 2014 obtained information online via websites. One-half of these shoppers used only online information, and 29% combined both websites and other sources like direct assistance, informal assistance, and via (offline) media. In the Health Reform Monitoring Survey from the Urban Institute Health Policy Center, a research team, funded by the Robert Wood Johnson Foundation and the Ford Foundation, looked into data collected from the Health Reform Monitoring Survey in March 2014 at the end of the 2014 open enrollment period for the
mHealth will join the health ecosystem – prelude to the 2014 Consumer Electronics Show
The rise of digital health at the 2014 Consumer Electronics Show signals the hockey-stick growth of consumer-facing health devices for fitness and, increasingly, more medical applications in the hands of people, patients, and caregivers. This year at #CES2014, while the 40% growth of the CES digital health footprint will get the headlines, the underlying story will go beyond wristbands and step-tracking generating data from an N of 1 to tools that generate data to bolster shared-decision making between people and the health system, and eventually support population health. For example: – Aetna is partnering with J&J to deploy their Care4Today
Chief Health Officers, Women, Are In Pain
Women are the Chief Health Officers of their families and in their communities. But stress is on the rise for women. Taking an inventory on several health risks for American women in 2013 paints a picture of pain: of overdosing, caregiver burnout, health disparities, financial stress, and over-drinking. Overdosing on opioids. Opioids are strong drugs prescribed for pain management such as hydrocodone, morphine, and oxycodone. The number of opioid prescriptions grew in the U.S. by over 300% between 1999 and 2010. Deaths from prescription painkiller overdoses among women have increased more than 400% since 1999, compared to 265% among men.
Eat fruits and vegetables: it’s worth $11 trillion to you and the U.S. economy
More than 127,000 people die every year in America from cardiovascular disease, accruing $17 billion in medical spending. Heart disease is a “costly killer,” according to the Union of Concerned Scientists, who has calculated The $11 trillion reward: how simple dietary changes can save lives and money, and how we get there, published in August 2013. That $11 trillion opportunity is equal to the present value of lives saved. The solution to bolstering heart (and overall health) and saving money (medical spending and personal productivity) is in food. We’re not talking about genetically engineering anything special or out-of-the-ordinary. We are talking
Americans’ health insurance illiteracy epidemic – simpler is better
Consumers misunderstand health insurance, according to new research published in the Journal of Health Economics this week. The study was done by a multidisciplinary, diverse team of researchers led by one of my favorite health economists, George Loewenstein from Carnegie Mellon, complemented by colleagues from Humana, University of Pennsylvania, Stanford, and Yale, among other research institutions. Most people do not understand how traditional health plans work: the kind that have been available on the market for over a decade. See the chart, which summarizes top-line findings: nearly all consumers believe they understand what maximum out-of-pocket costs are, but only one-half do.
The health care automat – Help Yourself to healthcare via online marketplaces
Imagine walking into a storefront where you can shop for an arthroscopy procedure, mammogram, or appointment with a primary care doctor based on price, availability, quality, and other consumers’ opinions? Welcome to the “health care automat,” the online healthcare marketplace. This is a separate concept from the new Health Insurance Marketplace, or Exchange. This emerging way to shop for and access health care services is explored in my latest paper for the California HealthCare Foundation (CHCF), Help Yourself: The Rise of Online Healthcare Marketplaces. What’s driving this new wrinkle in retail health care are: U.S. health citizens morphing into consumers,
The health and wellness gap between insured and uninsured people
If you have health insurance, chances are you take several actions to bolster your health such as take vitamins and supplements (which 2 in 3 American adults do), take medications as prescribed (done by 58% of insured people), and tried to improve your eating habits in the past two years (56%). Most people with insurance also say they exercise at least 3 times a week. Fewer people who are uninsured undertake these kinds of health behaviors: across-the-board, uninsured people tend toward healthy behaviors less than those with insurance. This is The Prevention Problem, gleaned from a survey conducted by TeleVox
Most employers will provide health insurance benefits in 2014…with more costs for employees
Nearly 100% of employers are likely to continue to provide health insurance benefits to workers in 2014, moving beyond a “wait and see” approach to the Affordable Care Act (ACA). As firms strategize tactics for a post-ACA world, nearly 40% will increase emphasis on high-deductible health plans with a health savings account, 43% will increase participants’ share of premium costs, and 33% will increase in-network deductibles for plan members. Two-thirds of U.S. companies have analyzed the ACA’s cost impact on their businesses but need to know more, according to the 2013 survey from the International Foundation of Employee Benefit Plans (IFEBP).
Dietitians provide a health bridge between food and pharmacy
The registered dietitian is an in-demand labor resource for grocery stores around the U.S. Advertising Age covered the phenomenon of the growing clout of dietitians in food chains (April 14, 2013). Let’s dig further into this phenomenon through the Health Populi lens on healthcareDIY and peoples’ ability to bend their personal health care cost curves. Stores such as Giant Eagle, Hy-Vee, Safeway and Wegmans are morphing into wellness destinations, with pharmacies and natural food aisles taking up valuable square footage to meet consumers’ growing demands for healthy choices. Some stores are formalizing their approach to food = health by formulating a
U.S. Health Costs vs. The World: Is It Still The Prices, and Are We Still Stupid?
Comparing health care prices in the U.S. with those in other developed countries is an exercise in sticker shock. The cost of a hospital day in the U.S. was, on average, $4,287 in 2012. It was $853 in France, a nation often lauded for its excellent health system and patient outcomes but with a health system that’s financially strapped. A routine office visit to a doctor cost an average of $95 in the U.S. in 2012. The same visit was priced at $30 in Canada and $30 in France, as well. A hip replacement cost $40,364 on average in the
The Not-So-Affordable Care Act? Cost-squeezed Americans still confused and need to know more
While health care cost growth has slowed nationally, most Americans feel they’re going up faster than usual. 1 in 3 people believe their own health costs have gone up faster than usual, and 1 in 4 feel they’re going out about “the same amount” as usual. For only one-third, health costs feel like they’re staying even. As the second quarter of 2013 begins and the implementation of the Affordable Care Act (ACA, aka “health reform” and “Obamacare”) looms nearer, most Americans still don’t understand how the ACA will impact them. Most Americans (57%) believe the law will create a government-run health plan,
Gettin’ higi with it: Lupe Fiasco’s foray into public health
The latest in SoLoMo (Social, Local, Mobile) Health is a gamified tool coupled with a hardware kiosk, known as higi. The brainchild of Michael Ferro, a successful dotcom entrepreneur who now owns the Chicago Sun-Times, higi’s mission is to help people – particularly younger peeps – to take better care of themselves by scoring points and, as a result, social connections. Higi’s an African word for origin, so the health tool has some aspects relating to being in a tribe — a kind of health tribe. It also has a fun sound to it, Ferro noted, which sets the vibe
Bill Clinton’s public health, cost-bending message thrills health IT folks at HIMSS
In 2010, the folks who supported health care reform were massacred by the polls, Bill Clinton told a rapt audience of thousands at HIMSS13 yesterday. In 2012, the folks who were against health care reform were similarly rejected. President Clinton gave the keynote speech at the annual HIMSS conference on March 6, 2013, and by the spillover, standing-room-only crowd in the largest hall at the New Orleans Convention Center, Clinton was a rock star. Proof: with still nearly an hour to go before his 1 pm speech, the auditorium was already full with only a few seats left in the
Butter over guns in the minds of Americans when it comes to deficit cutting
Americans have a clear message for the 113th Congress: I want my MTV, but I want my Medicare, Medicaid, Social Security, health insurance subsidies, and public schools. These budget-saving priorities are detailed in The Public’s Health Care Agenda for the 113th Congress, conducted by the Kaiser Family Foundation, Robert Wood Johnson Foundation, and the Harvard School of Public Health, published in January 2013. The poll found that a majority of Americans placed creating health insurance exchanges/marketplaces at top priority, compared with other health priorities at the state level. More people support rather than oppose Medicaid expansion, heavily weighted toward 75%
Think about health disparities on Martin Luther King Day 2013
On this day celebrating Martin Luther King, Jr., I post a photo of him in Detroit in 1963, giving a preliminary version of his “I Have a Dream” speech he would give two months later in Washington, DC. As I meditate on MLK, I think about health equity. By now, most rational Americans know the score on the nation’s collective health status compared to other developed countries: suffice it to say, We’re Not #1. But underneath that statistic is a further sad state of health affairs: that people of color in the U.S. have lower quality of health than white
Consumers blame insurance and pharma for health costs, but love their primary care doctors
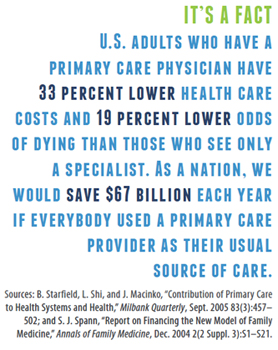
The 78% of U.S. adults with primary care physicians (think: medical homes) are very satisfied with their doctors’ visits. The main reasons for this high level of satisfaction include communication (listening, talking), customer service (caring, personable), and clinical (good diagnosis and treatment). More women than men have a primary care physician relationship, more college grads do, and more people with incomes of $75,000 a year or more do, as well. 90% of those 55 and over have a primary care doctor – a stat heavily influenced by the fact that Medicare coverage kicks in for older people. This consumer profile
Consumerism growing in health care, says Altarum
Patients are morphing into health care consumers with growing use of technology for medical shopping and health engagement, according to a survey conducted by Altarum, the health services research organization. Virtually all (99%) of U.S. health citizens want to play a role in medical decisions about their care. However, consumers vary in just how much of that responsibility they want to assume: – 35% want to make the final decision with some input from doctors and other experts – 29% want to be completely in charge of their decisions – 28% want to make a joint decision with equal input
Improving health care through Big Data: a meeting of the minds at SAS
Some 500 data analytics gurus representing the health care ecosystem including hospitals, physician practices, life science companies, academia and consulting came together on the lush campus of SAS in Cary, North Carolina, this week to discuss how Big Data could solve health care’s Triple Aim, as coined by keynote speaker Dr. Donald Berwick: improve the care experience, improve health outcomes, and reduce costs. Before Dr. Berwick, appointed as President Obama’s first head of the Centers for Medicare & Medicaid Services, Clayton Christensen of the Harvard Business School, godfather of the theory of disruptive innovation in business, spokee about his journey
It’s the prices and the technology, stupid: why U.S. health costs are higher than anywhere in the world
The price of physician services, proliferation of clinical technology and the cost of obesity are the key drivers of higher health spending in the U.S., according to The Commonwealth Fund‘s latest analysis in their Issues of International Health Policy titled, Explaining High Health Care Spending in the United States: An International Comparison of Supply, Utilization, Prices, and Quality, published in May 2012. The U.S. devotes 17.4% of the national economy to health spending, amounting to about $8,000 per person. The UK devotes about 10%, Germany 11.6%, France, 11.8%, Australia 8.7%, and Japan, 8.5%. On the physician pay front, primary care




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.