Our Pandemic Lessons: Listening to Michael Dowling – a #HIMSS21 Wrap-Up

“We don’t un-learn,” Dr. Amy Abernethy asserted as she shared her pandemic perspectives on a panel with 2 other former U.S. health policy and regulatory leaders. The three spoke about navigating compliance (think: regulations and reimbursement) in an uncertain world. An uncertain world is our workplace in the health/care ecosystem, globally, in this moment. So to give us some comfort in our collective foxhole, my last post for this week of immersion in #HIMSS21 is based on the keynote speech of Michael Dowling, CEO of Northwell Health. Dowling keynoted on the theme of “Leading for the Future,” sharing his lessons
Healthcare Via the Cloud, Across the Enterprise and in the Patient’s Home – a Sustainable View from Philips at HIMSS 2021
The COVID-19 pandemic sparked a reappraisal of value-based care, a shift to remote and virtual care, and acceleration of healthcare stakeholders’ investments in Artificial Intelligence-based solutions, Philips discovered in the 2021 Future Health Index, the company’s latest survey conducted among 2,800 health care leaders working in 14 countries. This week at the 2021 annual HIMSS conference, Philips is “making the case for moving to the cloud,” discussing the Philips HealthSuite, a cloud-based platform for connecting providers and patients, devices (and the data they generate), and care across the health care continuum. That’s a big promise and vision, so to kick
Zoom Became a Household Name in the Pandemic. It’s Working to Do the Same in Healthcare – At #HIMSS21
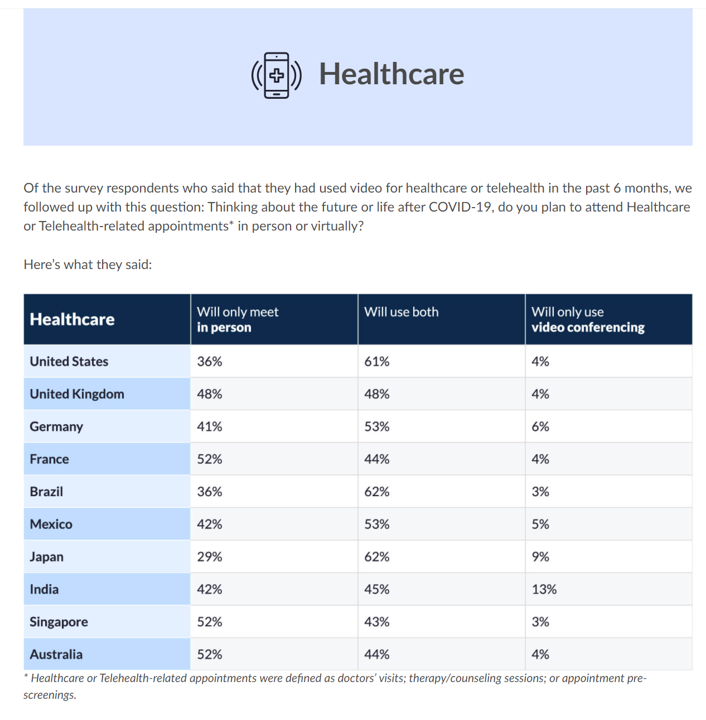
The COVID-19 pandemic digitally transformed most people living in the U.S., re-shaping consumers to work from home when possible, go to school there, and buy all manners of goods and services via ecommerce. In March 2021, Zoom conducted research into the question, “how virtual do we want our future to be?” posing that to thousands of citizens living in 10 countries including the U.S. As the first chart from the study illustrates, most people in America expect hybrid lifestyles, from fitness and retail to entertainment and education. And 7 in 10 U.S. health citizens want their health care to be
Empathy Is As Important as the Medical Treatment – the 2021 Accenture Health Experience As Backdrop to HIMSS 2021
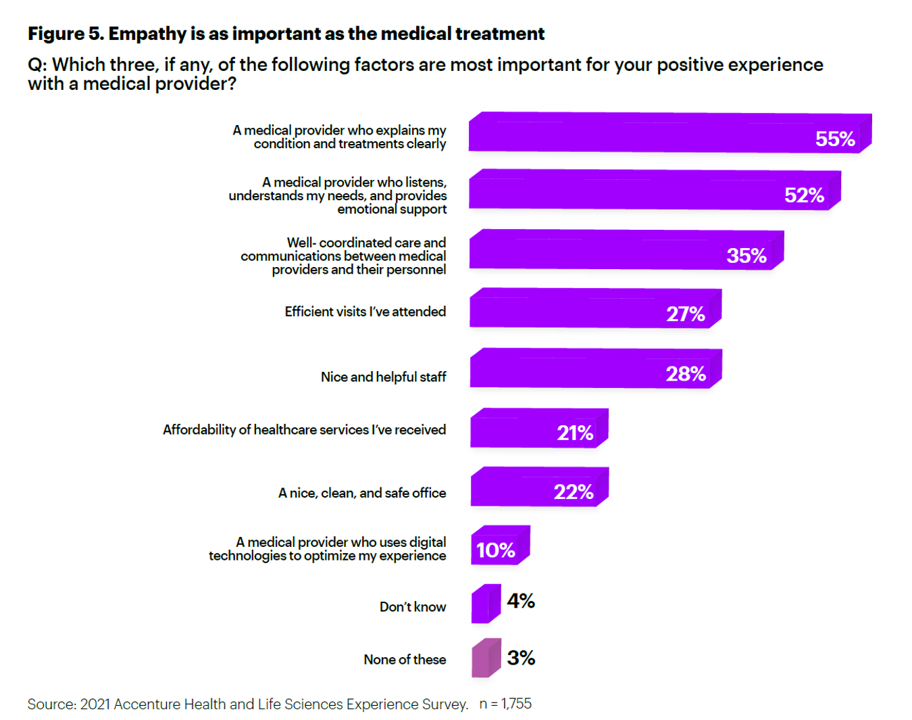
The rise of digital health investment and growing role of technology in health care services only accelerated during the COVID-19 pandemic. At the same time, people took on their own versions of digital transformation at home, for work, for school, for cooking, shopping, and indeed, for health care. But with digital health adoption gains has come some ambivalence and mixed signals, Accenture has discovered in its 2021 Health and life Sciences Experiences Survey released this week during the HIMSS Annual Conference. As the report concludes, “people’s sentiments and behaviors” with respect to technology in health care “provide no clear answer.”
Can the U.S. Improve Health System Performance with Digital Health Tools? Pondering A Big Question for #HIMSS21
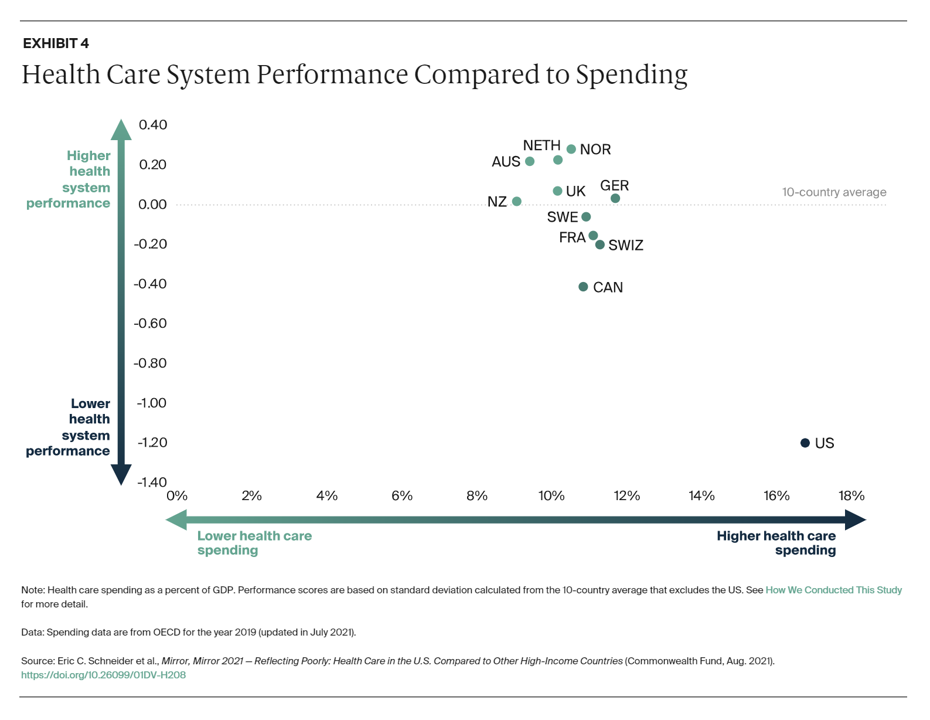
Simply put, is the equation, “Spend more, get less” a sustainable business model? Of course not. But that’s the simple math on U.S. health care spending and what comes from it, according to Mirror, Mirror 2021: Reflecting Poorly, a perennial report from The Commonwealth Fund that compares health system performance across eleven developed countries. The first table details the metrics that the Fund compares across the eleven peer nations, which included Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, the United Kingdom, and the United States. The metrics compared were access to care, care process, administrative efficiency, equity,
Americans Grew Digital Health-Data Muscles in the Pandemic – New Insights from the Pew Charitable Trusts

“Most Americans clearly recognize the potential benefits that improved health IT can offer, and they want this transformation of the health care system to continue,” the Pew Charitable Trusts research concludes in Most Americans Want to Share and Access More Digital Health Data. The Pew team surveyed 1,213 adults ages 18 and over in June and July 2020, interviewing in English and Spanish. As digital health industry stakeholders will be convening at the 2021 annual HIMSS conference in Las Vegas and digitally, this report is well-timed to give us a level-set on just “where” U.S. health citizens are with respect to
Women’s Health Re-shaped by COVID-19
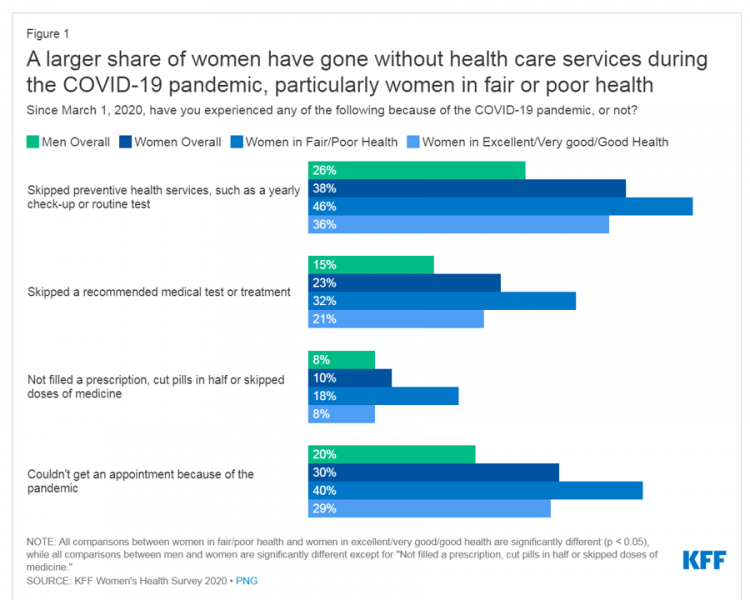
While women continue to outlive men in the U.S. in terms of life expectancy, the COVID-19 pandemic revealed continued healthcare access, physical and mental health disparities, and economic inequities for women in America. I addressed the changing state of post-pandemic women’s health in my latest contribution to the Medecision Liberation blog. This first graphic illustrates how women interacted with the U.S. health system during the pandemic in 2020. These data come from Kaiser Family Foundation’s women’s health survey conducted from the beginning of the pandemic starting March 1, 2020, and discovered that women in poorer or fair more likely went
What Poor Birth and Maternity Outcomes in the U.S. Say About American Healthcare & “Infrastructure”
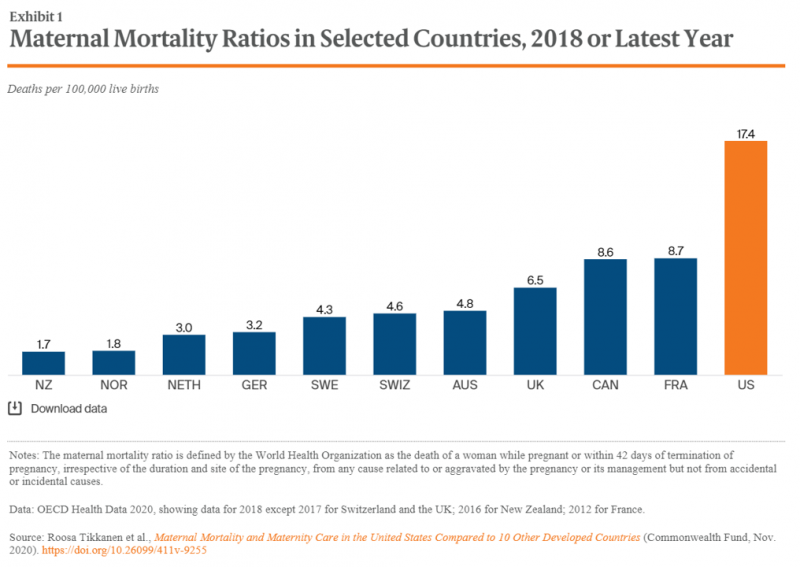
Cain Brothers is a 100+ year old financial services firm with a strong health care experience, now part of KeyBanc. A recent “House Calls” memo and podcast from two company analysts detailed the state of Medicaid, Motherhood and America’s Future: Giving Birth to Better Maternity Outcomes. Christian Pesci and David Johnson’s in-depth discussion detailed their bottom-line that, “maternity care in the U.S. is in crisis but poised for rapid evolution…(recognizing) that an uncoordinated system with misaligned incentives harms too many individuals, families, and communities.” They lay out the crisis as follows: Medicaid funds nearly one-half of births in the U.S.
CVS Finds Differences in Mental and Behavioral Health Among Men Vs. Women in the Pandemic
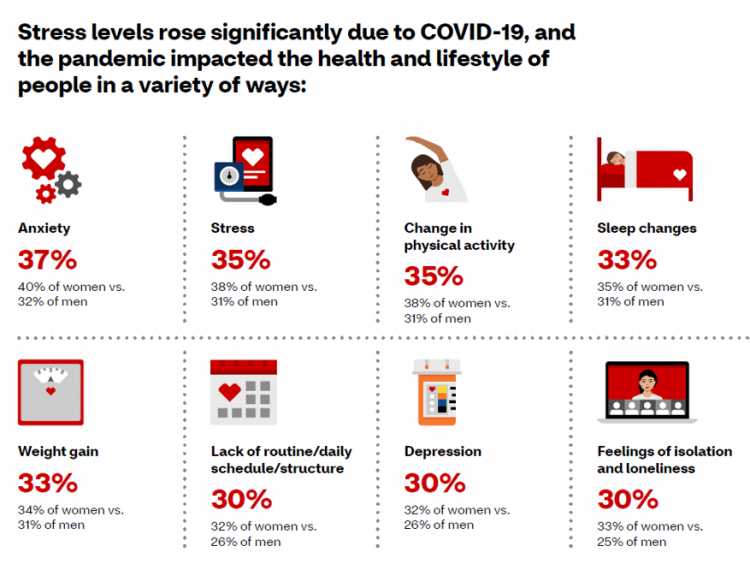
As the COVID-19 pandemic shifts to a more endemic phase — becoming part of peoples’ everyday life for months to come — impacts on peoples’ mental health will persist, according to new research from CVS Health in the company’s annual Health Care Insights Study. CVS conducted the annual Health Care Insights Study among 1,000 U.S. adults in March 2021. To complement the consumer study, an additional survey was undertaken among 400 health care providers including primary care physicians and specialists, nurse practitioners, physician assistants, RNs and pharmacists. CVS has been tracking the growing trend of health care consumerism in the
The Many Factors That Make a Child’s Well-Being Build Our Adult Health – the Aspirational OECD Framework
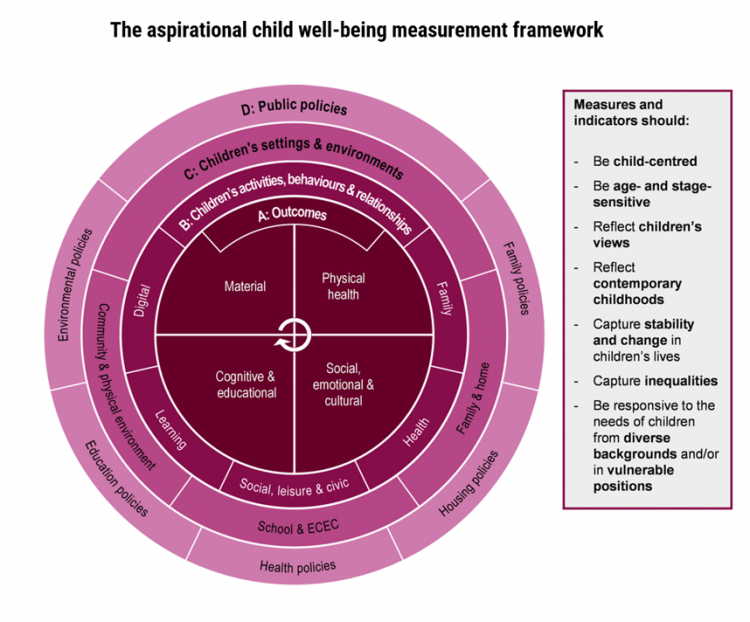
The ultimate health and wellbeing of an adult depends on the factors that shape us when we are children. A new, deep report from the OECD, Measuring What Matters for Child Well-being and Policies, spells out the many domains of experience that, together, bolster our whole health as we grow from child to adult. The first chart presents the OECD’s framework for measuring child well-being, calling out the nature of being “aspirational.” This re-look at children’s health data is aspirational because it is laying out how to best measure child well-being to set the bar higher for doing so. It addresses
Digital Inclusion As Upstream Health Investment
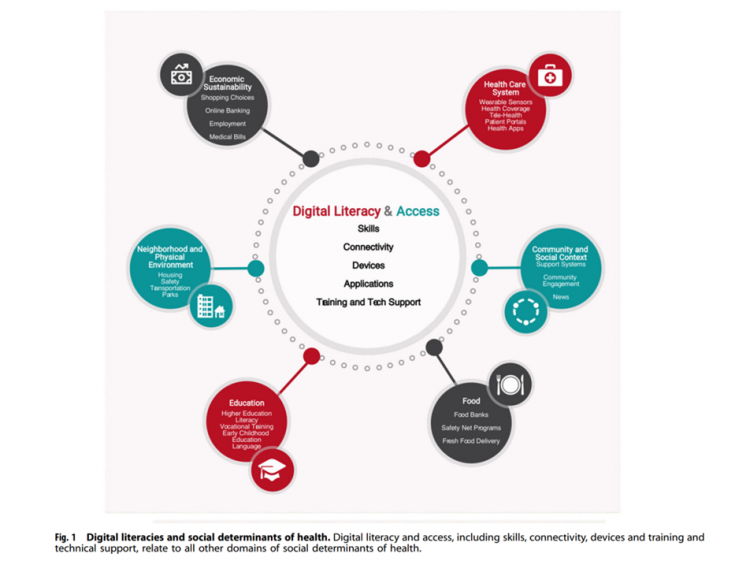
Without access to connectivity during the pandemic, too many people could not work for their living, attend school and learn, connect with loved ones, or get health care. The COVID-19 era has shined a bright light on what some of us have been saying since the advent of the Internet’s emergence in health care: that digital literacies and connectivity are “super social determinants of health” because they underpin other social determinants of health, discussed in Digital inclusion as a social determinant of health, published in Nature’s npj Digital Medicine. On the downside, lack of access to digital tools and literacies
The Healthiest Communities in the U.S. After the Pandemic – U.S. News & Aetna Foundation’s Post-COVID Lists

Some of America’s least-healthy communities are also those that index greater for vaccine hesitancy and other risks for well-being, found in U.S. News & World Report’s 2021 Healthiest Communities Rankings. U.S. News collaborated with the Aetna Foundation, CVS Health’s philanthropic arm, in this fourth annual list of the top geographies for well-being in the U.S. Six of the top ten healthiest towns in America are located in the state of Colorado. But #1 belongs to Los Alamos County, New Mexico, which also ranked first in ___. Beyond Colorado and New Mexico, we find that Virginia fared well for health in
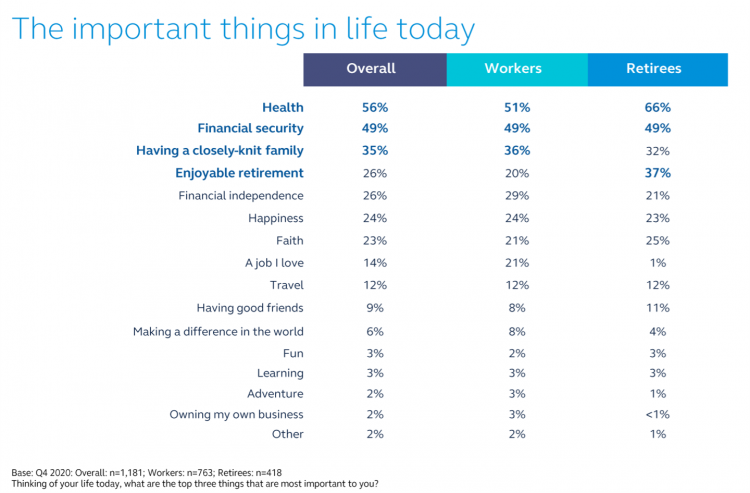
Reimagining Life After the Pandemic – Seeking Health, Safety, Sustainability, and Trust
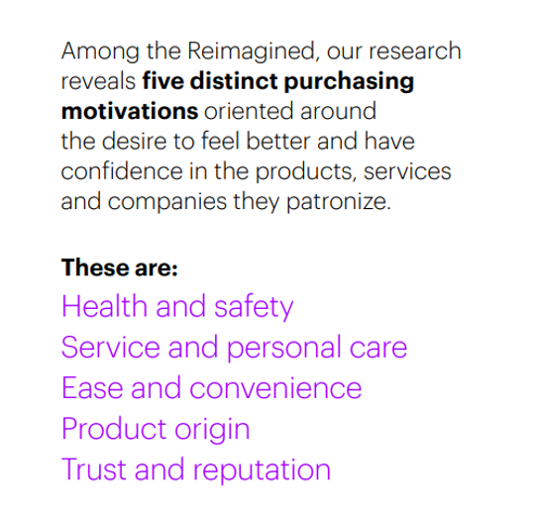
COVID-19 reshaped people around the world, one-half of whom are re-defining their personal purpose and life-goals. This sense of purpose extends to peoples’ willingness to buy or patronize companies who do not meet their needs for health, safety, sustainability and trust. For example, two in three of these people would switch travel brands if they felt health and safety weren’t up to par, discovered in Life Reimagined – Mapping the motivations that matter for today’s consumers, from Accenture’s Voices of Change series. In May 2021, Accenture polled over 25,000 consumers globally, in 22 countries, and found that one-half of people
Color Me Healthy – Pantone’s Forecast on Post-Pandemic Well-Being and Design

Post-pandemic, the consumer’s priority purchases are grocery, nesting, and health, according to David Shah, a leading thinker about social and design trends. David presented the latest Pantone forecast on color and society in NewTopia – A Balance of Color Opposites – Color for a Post-COVID World this week. I had the opportunity to attend the session, and want to share the health and wellness-related insights David shared in his fast-paced view on the role of color in bolstering wellbeing and community looking out to 2022/23. For context, Pantone plays a role in your life you might not realize. In health
5.5 Million Years of Life Will Be Lost Due to COVID-19 in the U.S. in 2020
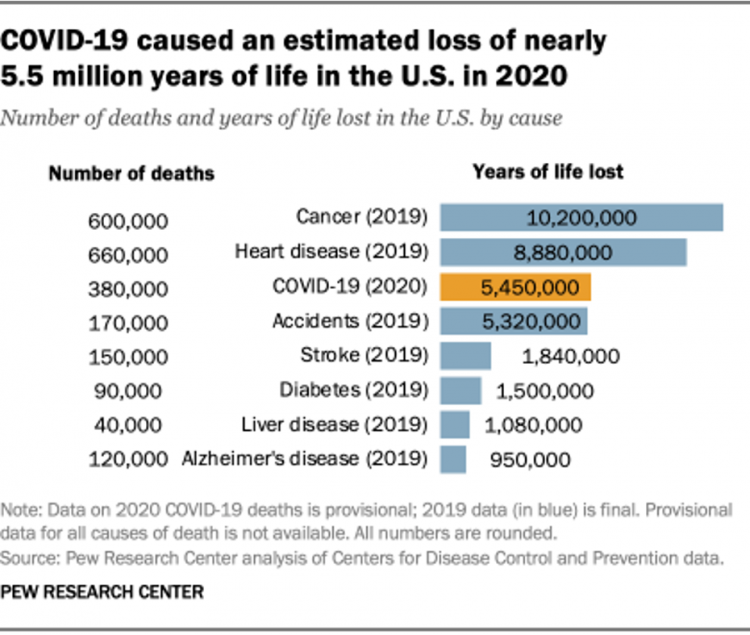
In 2020 in the U.S., 380,000 people are expected to die due to COVID-19. These people lost due to the coronavirus would, collectively, have lived another 5.5 million life-years would they not have succumbed to the virus. COVID-19 has cut lives short relative to their life expectancy, calculated in an analysis by the Pew Research Center based on CDC data from 2019 and 2020, coupled with additional statistics on life expectancy by age and gender. The bottom-line from the Pew Research Center’s analysis, simply stated, is that, “The pandemic…has killed many Americans who otherwise might have expected to live for
The Stress of the Caregiver: The Most Over-Utilized, Unpaid Stakeholder in U.S. Healthcare

We’ve long know that “the patient” has been an under-utilized resource in the U.S. healthcare system since Dr. Charles Safran testified with that statement to Congress way back in 2004…an era where bipartisanship for health IT was a real thing. Today, with the insights of Alexandra Drane (Founder of ARCHANGELS) and Dr. Nirav Shah (of Stanford University), we know that caregivers are among the most over-utilized resources in the U.S. healthcare system — overused, over-stressed, under-paid, detailed n How Health Systems Can Care for Caregivers, published in the NEJM Catalyst July 2021 issue. In this study, Drane and Shah analyze
The Digital Home: A Platform for Health, via Deloitte and the COVID-19 “Stress Test”
Wherever you live in the world touched by the coronavirus pandemic, you felt (and were) stress-tested. Both you were, and your home was as well. In this year’s 2021 annual report by Deloitte into Connectivity & Mobile Trends, their report details How the pandemic has stress-tested the crowded digital home. This analysis was done, as it is every year, by the Deloitte Center for Technology, Media & Telecommunications. Deloitte’s Center commissioned an online survey among 2,009 U.S. consumers to gauge five generations of peoples’ perspectives on connected life in the context of COVID. The report covers the various life-flows of
Post-Pandemic, U.S. Healthcare is Entering a “Provide More Care For Less” Era – Pondering PwC’s 2022 Forecast

In the COVID-19 pandemic, health care spending in the U.S. increased by a relatively low 6.0% in 2020. This year, medical cost trend will rise by 7.0%, expected to decline a bit in 2022 according to the annual study from PwC Health Research Institute, Medical Cost Trend: Behind the Numbers 2022. What’s “behind these numbers” are factors that will increase medical spending (the “inflators” in PwC speak) and the “deflators” that lower costs. Looking around the future corner, the inflators are expected to be: A COVID-19 “hangover,” leading to increased health care services utilization Preparations for the next pandemic, and
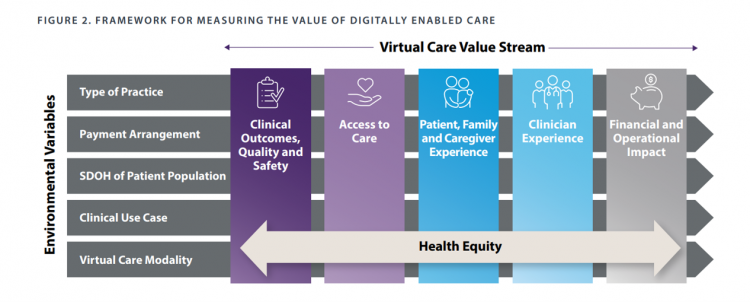
The ROI on Virtual Care – Thinking About Value and Future Prospects With the AMA
When a new technology or product starts to get used in a market, it follows a diffusion curve whose slope depends on the pace of adoption in that market. For telehealth, that S-curve has had a very long and fairly flat front-end of the “S” followed by a hockey stick trajectory in March and April 2020 as the COVID-19 pandemic was an exogenous shock to in-person health care delivery. The first chart from the CDC illustrates that dramatic growth in the use of telehealth ratcheting up since the first case of COVID-19 was diagnosed in the U.S. Virtual care has
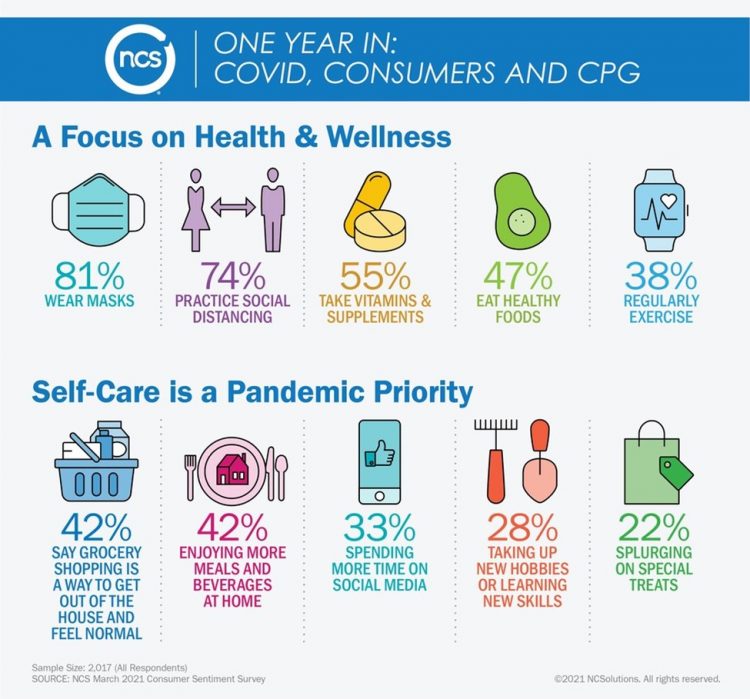
Americans’ Views on Food Have Been Re-Shaped by the Pandemic: Think Security, Immunity, and Sustainability

As vaccinations jabbed into peoples’ arms in the U.S. continue to immunize health citizens from contracting the coronavirus, millions of folks are looking forward to getting back inside restaurants to enjoy meals out, as well as un-masking when grocery shopping. But people in the U.S. love their food both outside and inside the home: about one-half of people in the U.S. are continuing to cook at home more, according to the 2021 Food & Health Survey published today by the International Food Information Council (IFIC). This sixteenth annual report is a go-to for those of us in the health/care ecosystem who
Nurses Hacking for Health and Compassionomics

The hearts and minds of nurses are fertile and inspirational sources and engines for health care innovation. This past weekend, and for the second time, I had the privilege and opportunity to be a panelist for the perennial hackathon meet-up of Nurse Hack 4 Health, sponsored by Microsoft, Johnson & Johnson, Sonsiel, and DevUp. This round, the hackathon attracted hundreds of nurses from at least 20 countries and 30 U.S. states. Even a few students attended, a growing trend as academia recognizes the shortage of workers trained to solve thorny problems of the world. In health care, right here, right
Thinking Mothers’ Health at Mother’s Day 2021…and the Marshall Plan for Moms

To all the Moms I’ve loved and lost and those I still blessed to have in my life…. I’m thinking about our collective and individual health this 2021 Mother’s Day weekend. There are three themes that whirl in the current Moms’ Health Mix: The impact of the COVID-19 pandemic on mothers’ health and life Mom-economics and the She-Cession — the financial roots of health inequity, and The larger context that is the persistence of women’s health disparities. First, the impact of the coronavirus and the economy have been intertwined, hitting women hard in terms of physical health, work, mental health
Consumers’ Health Concerns Grow in the Pandemic Across All Categories – And More Trust Virtual Care
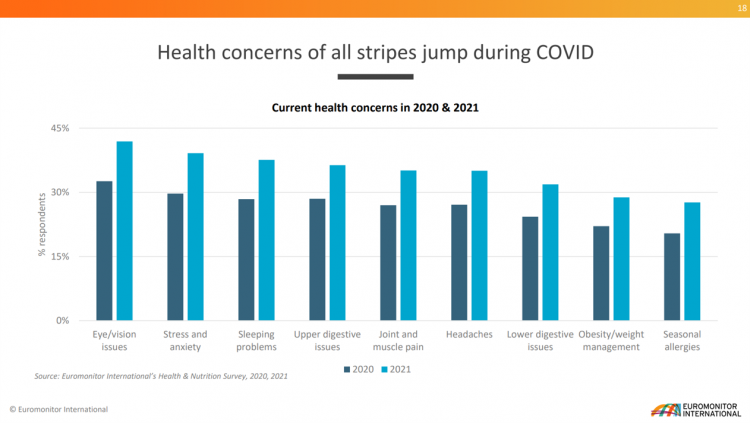
While the “in-person” visit to a doctor or medical professional continues to rank first as consumers’ most-trusted information source, the virtual doc or clinician rose in trust during the COVID-19 pandemic, according to Euromonitor’s latest read on Consumer Health: Changes in Consumer Behaviour during COVID-19 . The first four most-trusted sources for health information in 2021 remained the same short-list from 2020: doctors in-person, pharmacists, nutritionists and dieticians, and government or NGOs. But fifth place slipped from family and friends to the pharma industry, and sixth in line went to virtual doctors or medical professionals rising from 9th place in
And the Oscar Goes To….Power to the Patients!
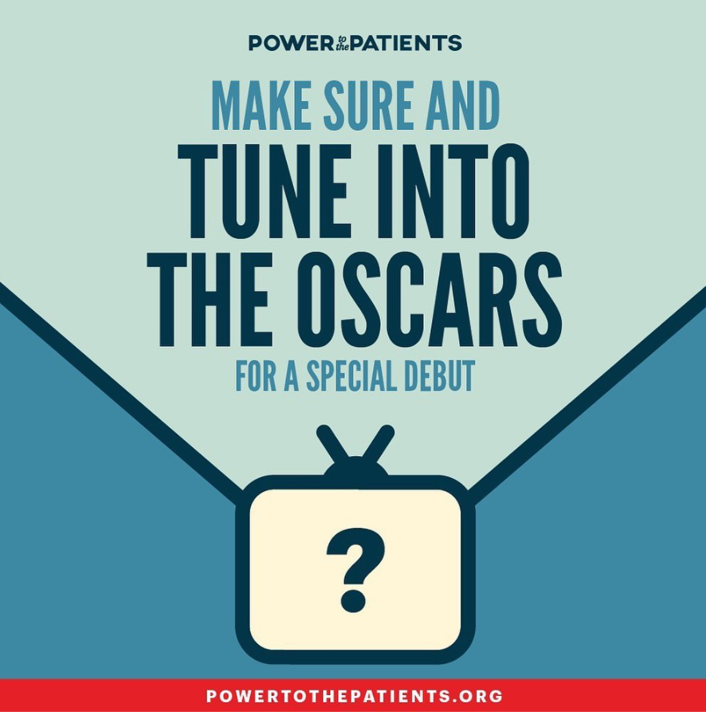
Health care has increased its role in popular culture over the years. In movies in particular, we’ve seen health care costs and hassles play featured in plotlines in As Good as it Gets [theme: health insurance coverage], M*A*S*H [war and its medical impacts are hell], and Philadelphia [HIV/AIDS in the era of The Band Played On], among dozens of others. And this year’s Oscar winner for leading actor, Anthony Hopkins, played The Father, who with his family is dealing with dementia. [The film, by the way, garnered six nominations and won two]. When I say “Oscar” here on the Health
Health Disparities and the Risks of Social Determinants for COVID-19 – 14 Months of Evidence
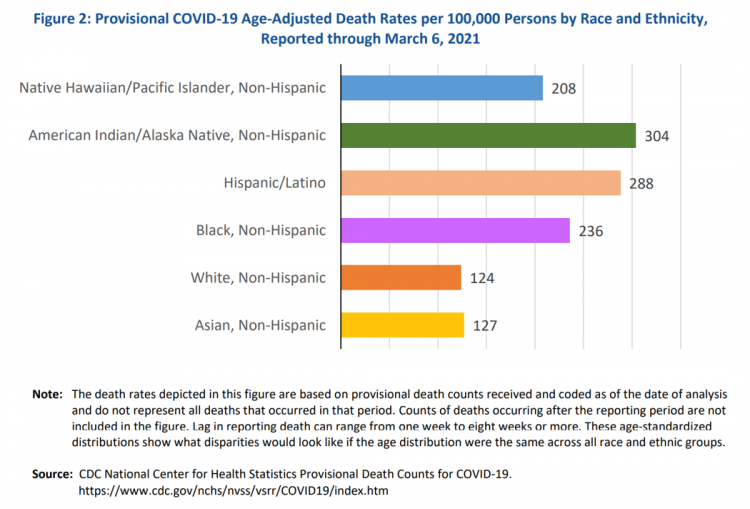
In April 2020, the U.S. Centers for Disease Control issued a report featuring evidence that in the month of March 2020, the coronavirus pandemic was not an equal-opportunity killer. Within just a couple of months of COVID-19 emerging in America, it became clear that health disparities were evident in outcomes due to complications from the coronavirus. An update from that early look at differences in COVID-19 diagnoses and mortality rates was published in Health Disparities by Race and Ethnicity During the COVID-19 Pandemic: Current Evidence and Policy Approaches, In this report, the Assistant Secretary for Planning and Evaluation, part of
Virtual Health Tech Enables the Continuum of Health from Hospital to Home

In the COVID-19 pandemic, as peoples’ daily lives shifted closer and closer to home, and for some weeks and months home-all-the-time, health care, too, moved beyond brick-and-mortar hospitals and doctors’ offices. The public health crisis accelerated “what’s next” for health care delivery, detailed in A New Era of Virtual Health, a report published by TripleTree. TripleTree is an investment bank that has advised health care transactions since 1997. As such, the team has been involved in digital health financing and innovation for 24 years, well before the kind of platforms, APIs, and cloud computing now enabling telehealth and care, everywhere. The
Health, the Great Unifier (For Most)

As the COVID-19 expanded peoples’ consciousness about infectious disease and opportunities to keep a tricky virus at bay, consumers grew new muscles about public and individual wellness…now, “more invested in achieving it,” according to In Health We Trust, a survey report from Healthline Media. To gauge Americans changing perspectives on personal health, HealthLine conducted surveys among 1,533 U.S. consumers age 18 and over in February 2020 (just about the time the coronavirus pandemic was emerging in the U.S.) and 1,577 consumers in December 2020. One of the subtle shifts in health care consumerism concerns cost, which before the pandemic has
The Post-COVID 19 Health Consumer: Ready for DIY Health Care and More Open to Telehealth

The COVID-19 pandemic has re-shaped consumers for work, school, fitness, cooking, and certainly for health care. PwC’s Health Research Institute has combed through their consumer survey data and developed insights on health consumers, shared in a summary titled Consumer health behavior and the COVID-19 pandemic: What we’ve learned. Most U.S. consumers would be likely to have a clinician visit their homes for several kinds of medical care, including: “DIY care,” as PwC exemplifies as a home strep or flu test, or remote monitoring, likely among 85% of people A chronic care visit, likely for 78% of consumers A visit for
The Pandemic’s Death Rate in the U.S.: High Per Capita Income, High Mortality
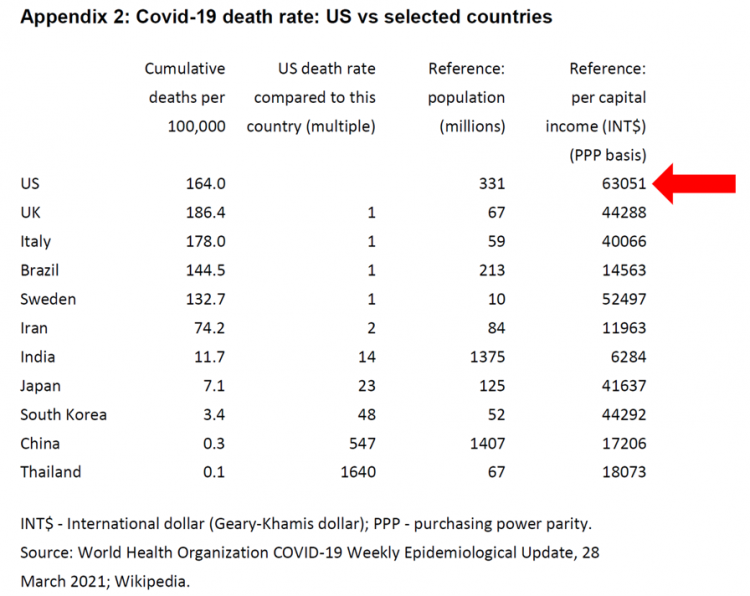
The United States has among the highest per capita incomes in the world. The U.S. also has sustained among the highest death rates per 100,000 people due to COVID-19, based on epidemiological data from the World Health Organization’s March 28, 2021, update. Higher incomes won’t prevent a person from death-by-coronavirus, but risks for the social determinants of health — exacerbated by income inequality — will and do. I have the good fortune of access to a study group paper shared by Paul Sheard, Research Fellow at the Mossaver-Rahmani Center for Business and Government at the Harvard Kennedy School. In reviewing
Emerging with A Stronger Healthcare System Post-COVID: NAM’s Lessons Learned
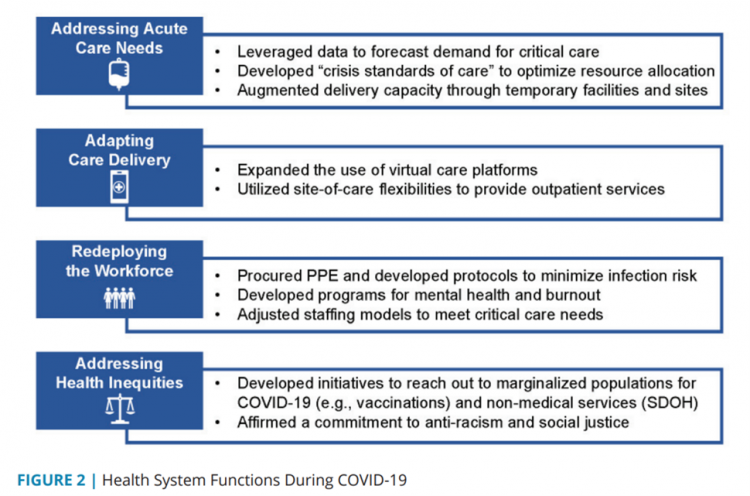
The coronavirus pandemic exposed weaknesses in the U.S. health care system that existed before the public health crisis. What lessons can be learned from the COVID-19 stress-test to build American health care back better? The National Academy of Medicine is publishing nine reports addressing health stakeholder segments impacted and re-shaped by COVID-19 — for public health, quality and safety, health care payers, clinicians, research, patients-families-communities, health product manufacturers, digital health, and care systems. The report on health care systems and providers was released this week: COVID-19 Impact Assessment: Lessons Learned and Compelling Needs was authored by experts on the front-line
Housing as Prescription for Health/Care – in Medecision Liberation

COVID-19 ushered in the era of our homes as safe havens for work, shopping, education, fitness-awaking, bread-baking, and health-making. In my latest essay written for Medecision, I weave together new and important data and evidence supporting the basic social determinant of health — shelter, housing, home — and some innovations supporting housing-as-medicine from CVS Health, UnitedHealth Group, AHIP, Brookings Institution, the Urban Land Institute, and other stakeholders learning how housing underpins our health — physical, mental, financial. Read about a wonderful development from Communidad Partners, working with the Veritas Impact Partners group, channeling telehealth to housing programs serving residents with
How Fruits and Veg Can Make Health and Lower Costs – Calling Chef José Andrés to the White House
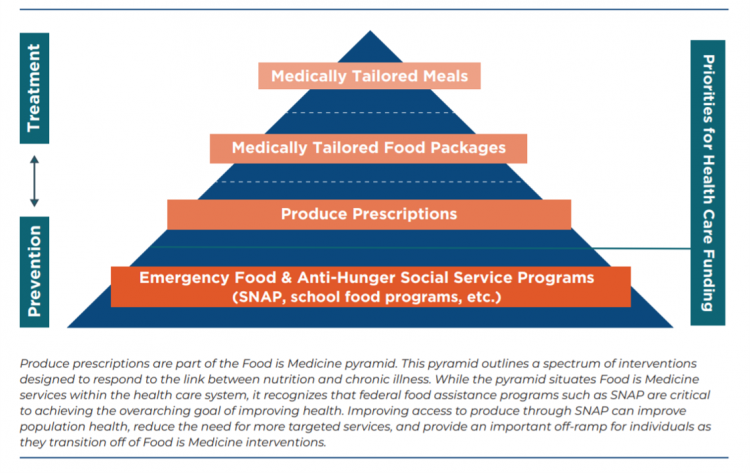
Springtime is finally emerging on the east coast of the U.S. and my local CSA farm is on my mind. It’s timely, then, to re-visit a research paper on subsidizing fruits and vegetables from a March 2019 issue of PLOS as an introduction to a new initiative growing out of The Center for Health Law and Policy Innovation of Harvard Law School (CHLPI) on produce prescriptions. Timely, too, that Chef José Andrés has been called to President Biden’s White House to help address food security in America. First, let’s look at the research in PLOS: Cost-effectiveness of financial incentives for
How Grocery and Retail Companies Are Delivering Health and Healthcare
The Wall Street Journal featured the grocery chain Kroger in an article yesterday titled, COVID-19 Vaccinations, Tests Give Boost to Kroger’s Health Ambitions. “With 2,250 pharmacies and 220 clinics largely in the Midwest and the southern U.S., Kroger is the fourth-largest pharmacy operator by script count,” the Journal noted, adding details about Walmart, CVS Health, and Walgreens all fast-expanding their respective health care footprints. As more consumers view their homes as personal and safe health havens, there is no shortage of suppliers in the food, retail, and mobility sectors working fast to meet that demand for convenient and accessible services.
The Patient Safety Issue of Racial Disparities and the Opportunity for “Health Equity By Design”

In 2021, racial and ethnic disparities in healthcare are a top patient safety issue, according to ECRI’s annual list of major concerns facing healthcare consumers’ risks to adverse events that can harm them. ECRI has published their annual Top 10 list since 2018, when the list featured diagnostic errors, o behavioral health needs in acute care settings, and patient engagement and health literacy — all of which play into this year’s #1 issue, racial and ethnic disparities in health care. In fact, among the risks in this year’s Top Ten list, eight were accelerated and highlighted by the COVID-19 pandemic
Stress in America, One Year into the Pandemic – an APA Update on Parents, Healthcare Workers, and Black Americans
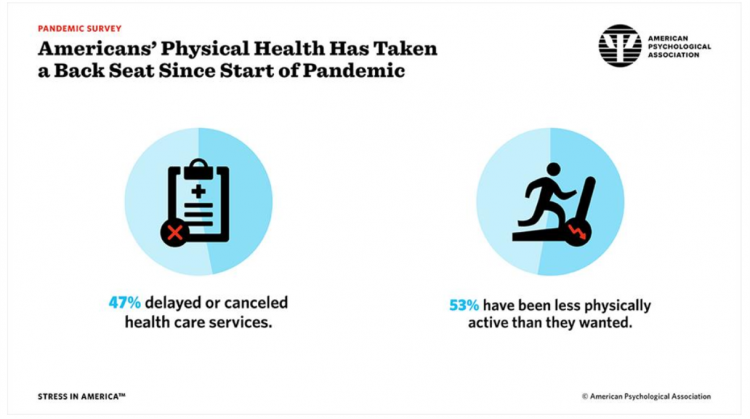
A Year into our collective coronavirus experience, Americans remain stressed, with physical health taking a back seat to our daily grinds based on the 2021 Stress in America survey from the American Psychological Association (APA). The APA has been updating us on U.S.-stress for several years, and more frequently since the start of the COVID-19 pandemic at the start of 2020. In their latest report, APA updates their previous profiles of Americans’ stress looking into different demographic groups and coping mechanisms. The topline, across all adults living in America, is that one-half have delayed or cancelled health care services. One-half has
The Ongoing Reality of COVID-19 – My Conversation with Dr. Michael Osterholm at SXSW
“So close and yet so far” feels like the right phrase to use a year after the World Health Organization used the “P-word,” “pandemic,” to describe the coronavirus’s impact on public health, globally. One year and over 550,000 COVID-related deaths in the U.S. later, we face a New Reality that Dr. Michael Osterholm and I are brainstorming today at the 2021 South-by-Southwest Festival. Usually held live and very up-close-and-personally crowded in Austin, Texas, this year we are all virtual — including the film, music, and interactive festivals alike. While I regret to not be in the same room as Dr.
A BA Degree as Prescription for a Longer Life – Update on Deaths of Despair from Deaton and Case
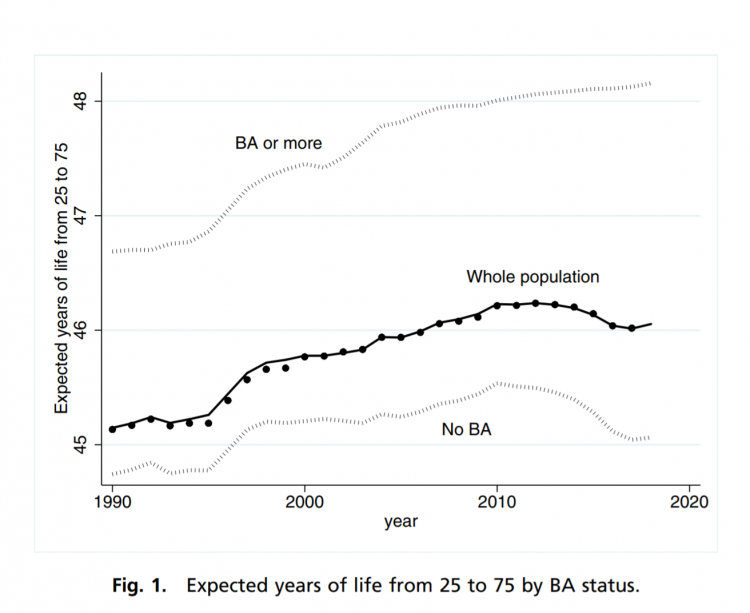
“Without a four-year college diploma, it is increasingly difficult to build a meaningful and successful life in the United States,” according to an essay in PNAS, Life expectancy in adulthood is falling for those without a BA degree, but as educational gaps have widened, racial gaps have narrowed by Anne Case and Angus Deaton. Case and Deaton have done extensive research on the phenomenon of Deaths of Despair, the growing epidemic of mortality among people due to accidents, drug overdoses, and suicide. Case and Deaton wrote the book on Deaths of Despair (detailed here in Health Populi), Case and Deaton
How to Restore Americans’ Confidence in U.S. Health Care: Deal With Access and Cost
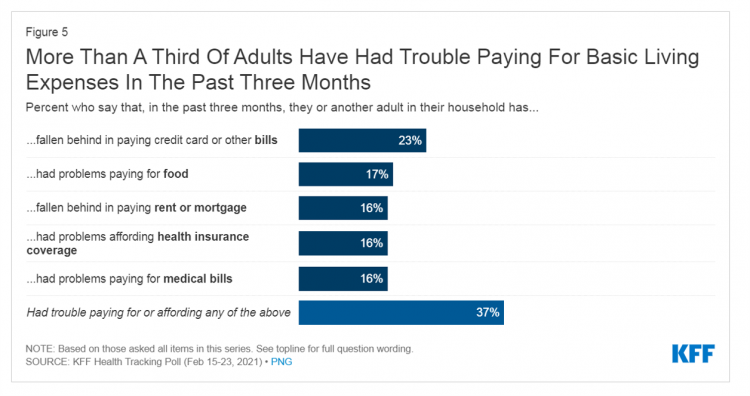
With a vaccine supply proliferating in the U.S. and more health citizens getting their first jabs, there’s growing optimism in America looking to the next-normal by, perhaps, July 4th holiday weekend as President Biden reads the pandemic tea leaves. But that won’t mean Americans will be ready to return to pre-pandemic health care visits to hospital and doctor’s offices. Now that hygiene protocols are well-established in health care providers’ settings, at least two other major consumer barriers to seeking care must be addressed: cost and access. The latest (March 2021) Kaiser Family Foundation Tracking Poll learned that at least one
“Hope Springs Eternal” With the COVID Vaccine for Both Joe Biden and Most People in the U.S.
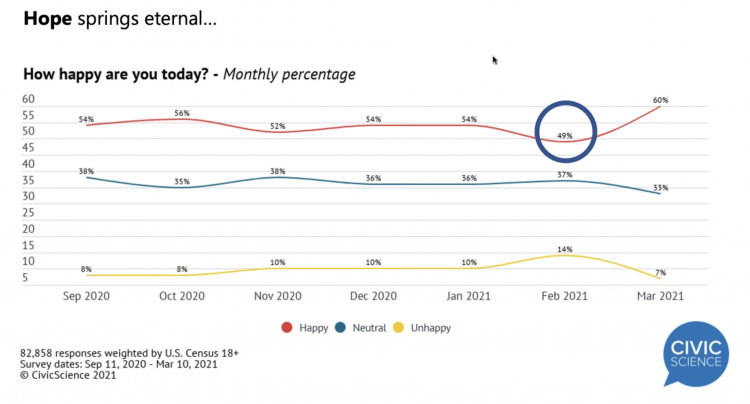
More Americans are happier in March 2021 than they’ve been for a year, based on consumer research from Civic Science polling U.S. adults in early March 2021. For the first time, a larger percent of Americans said they were better off financially since the start of the pandemic. This week, Civic Science shared their latest data on what they’re seeing beyond the coronavirus quarantine era to forecast trends that will shape a post-COVID America. Buoying peoples’ growing optimism was the expectation of the passage of the American Cares Act, which President Biden signed into effect yesterday. The HPA-CS Economic Sentiment Index
Value-Based Health Care Needs All Stakeholders at the Table – Especially the Patient

2021 is the 20th anniversary of the University of Michigan Center for Value-Based Insurance Design (V-BID). On March 10th, V-BID held its annual Summit, celebrating the Center’s 20 years of innovation and scholarship. The Center is led by Dr. Mark Fendrick, and has an active and innovative advisory board. [Note: I may be biased as a University of Michigan graduate of both the School of Public Health and Rackham School of Graduate Studies in Economics]. Some of the most important areas of the Center’s impact include initiatives addressing low-value care, waste in U.S. health care, patient assistance programs, Medicare
Ten Forces Shaping Health Care in 2021: A View from CVS Health

Expanding omni-channel, data-driven, cost-effective health care in the community, tailoring that care, and attending to mental health paint the picture of health through the lens of CVS Health. The company published the Health Trends Report 2021 today, calling out ten forces shaping health care this year. Those themes are, The Year of the Pharmacist The Next Step Forward in Cardiac Care Cancer Needs a Better Roadmap The EHR Hits Its Stride The Mental Health Shadow of COVID-19 Tailor Care to the Older Patient More Agents that Predict Disease Paying for the New Medical Miracle Virtual Care Goes Mainstream, and Diabetes
The Most Relevant Companies in Health Care – Learning from the W2O Group
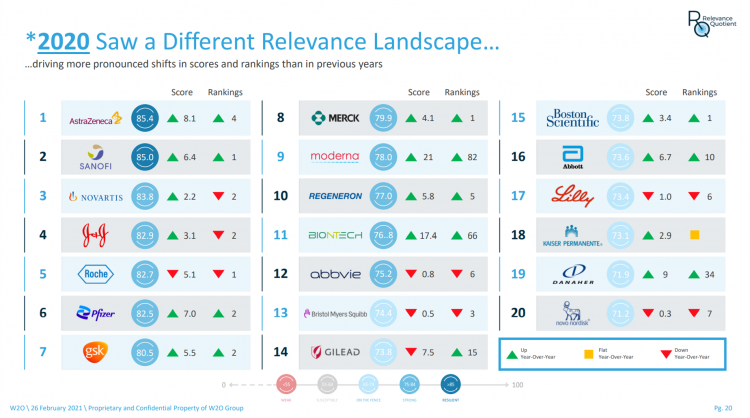
Five years ago, in 2016, the W2O Group said that, “Relevance is reputation.” That year the firm began to study the relevance of, well, relevance for organizations especially operating in the health/care ecosystem. 2020 changed everything, the W2O team asserts, now issuing its latest look into the issue through the Relevance Quotient. Relevance is built on recognizing, meeting and exceeding stakeholder expectations of organizations. In the Relevance Quotient methodology, W2O Group defines key stakeholders as employees, patients (including the sick and the well, caregivers, consumers, et al), health care providers, advocacy groups, analysts and investors, policy makers, journalists and media outlets.
Americans Lost Future Life-Years in 2020: How Much Life Was Lost Depends on the Color of One’s Skin
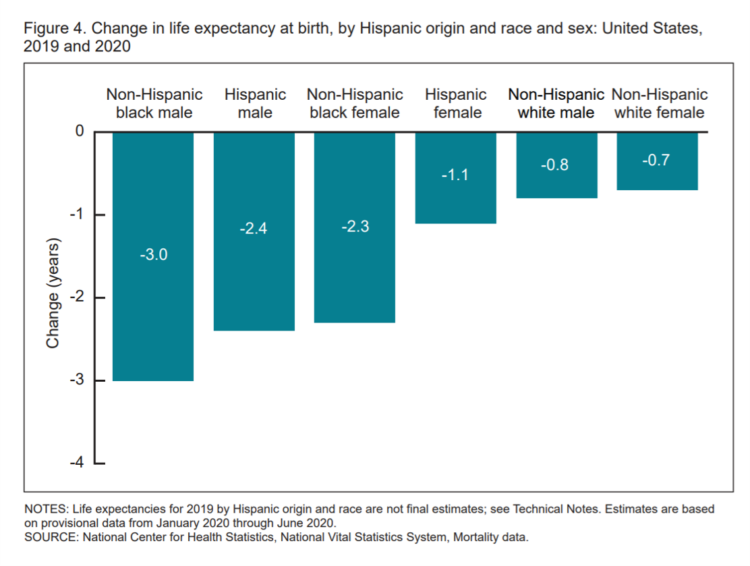
Some people remark about 2020 being a “lost year” in the wake of the coronavirus pandemic. That happens to be a true statement, sadly not in jest: in the U.S., life expectancy at birth fell by one full year over the first half of 2020 compared with 2019, to 77.8 years. In 2019, life expectancy at birth was 78.8 years, according to data shared by the National Center for Health Statistics (NCHS), part of the Centers for Disease Control and Prevention (CDC). Life expectancy at birth declined for both females and males, shown in the first chart. The differences between
The Social Determinants of Prescription Drugs – A View From CoverMyMeds
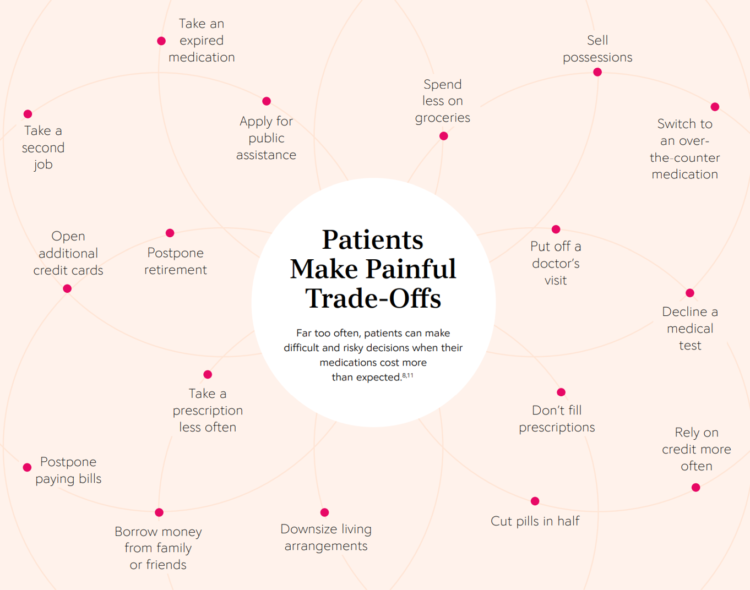
The COVID-19 pandemic forced consumers to define what were basic or essential needs to them; for most people, those items have been hygiene products, food, and connectivity to the Internet. There’s another good that’s essential to people who are patients: prescription drugs. A new report from CoverMyMeds details the current state of medication access weaving together key health care industry and consumer data. The reality even before the coronavirus crisis emerged in early 2020 was that U.S. patients were already making painful trade-offs, some of which are illustrated in the first chart from the report. These include self-rationing prescription drug
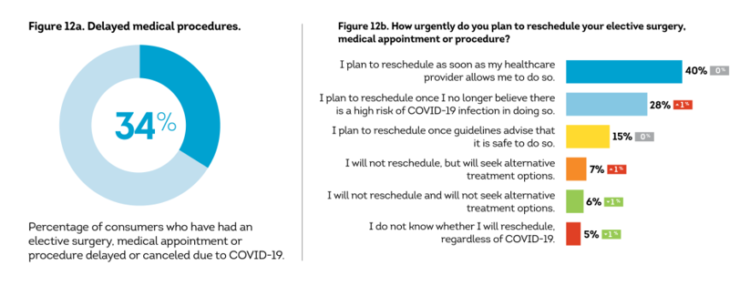
Three in Four People Avoiding Health Care in the Pandemic Have Had Chronic Conditions
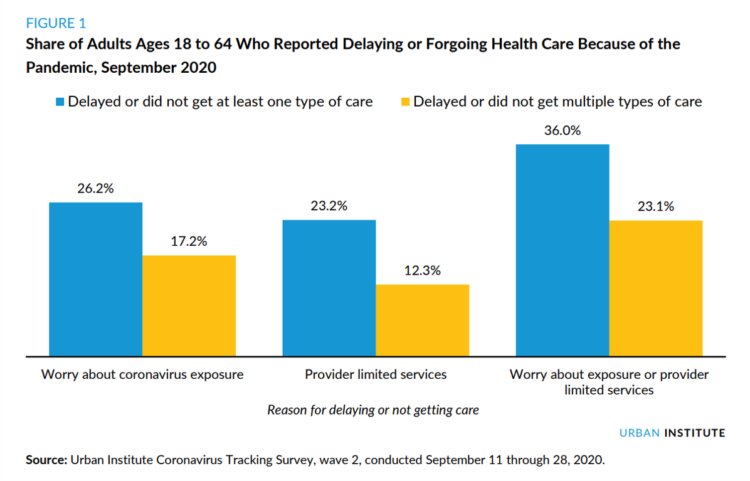
By the autumn of 2020, U.S. physicians grew concerned that patients who were avoiding visits to doctor’s offices were missing care for chronic conditions, discussed in in Delayed and Forgone Health Care for Nonelderly Adults during the COVID-19 Pandemic from the Urban Institute. More than three-fourths of people who delayed or forewent care had at least one chronic health condition. The pandemic may have led to excess deaths from diabetes, dementia, hypertension, heart disease, and stroke, as well as record drug overdoses in the 12 months ending in May 2020. In their JAMA editorial on these data, Dr. Bauchner and
The Health Care Cost Curve is Bending Down – A New View from Deloitte
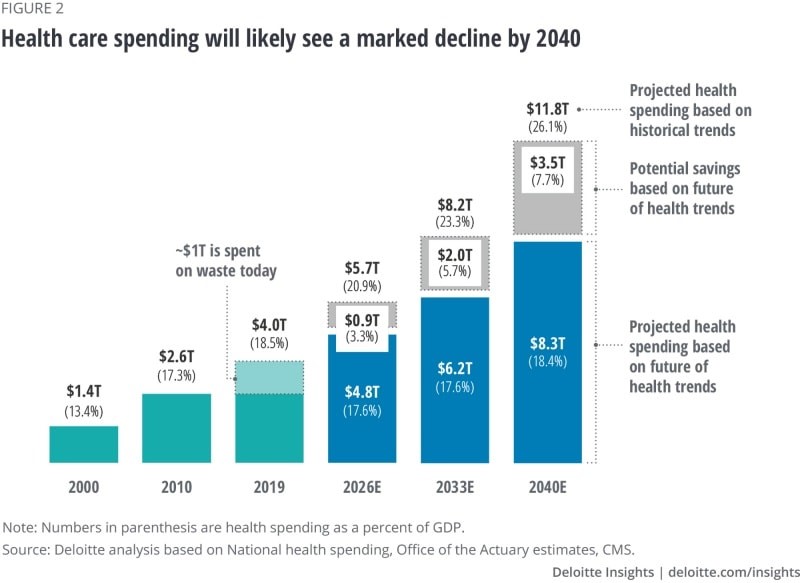
Over the next 20 years, health care spending in the U.S. will migrate toward well-being and the early detection of disease, away from the funding of America’s sick-care system, according to Breaking the cost curve, a forecast of U.S. health economics in the year 2040 from Deloitte. Current spending on health care in America is roughly $4 trillion (with a “t”) dollars, approaching 20% of the nation’s economy. By 2040, spending is projected to be $8.3 trillion based on future health trends — not historic workflows and delivery mechanisms which would consume an additional $3.5 trillion — close to what we
Ten In Ten: Manatt’s Healthcare Priorities to 2031

The coronavirus pandemic has exposed major weaknesses in the U.S. health care system, especially laying bare inequities and inertia in American health care, explained in The Progress We Need: Ten Health Care Imperatives for the Decade Ahead from Manatt Health. The report details the ten objectives that are central to Manatt’s health care practice, a sort of team manifesto call-to-action and North Star for the next decade. Their ten must-do’s for bending the cost curve while driving constructive change for a better health care system are to: Ensure access Achieve health equity Stability the safety net and rebuild public health
Call It Deferring Services or Self-Rationing, U.S. Consumers Are Still Avoiding Medical Care
Patients in the U.S. have been self-rationing medical care for many years, well before any of us knew what “PPE” meant or how to spell “coronavirus.” Nearly a decade ago, I cited the Kaiser Family Foundation Health Security Watch of May 2012 here in Health Populi. The first chart here shows that one in four U.S. adults had problems paying medical bills, largely delaying care due to cost for a visit or for prescription drugs. Fast-forward to 2020, a few months into the pandemic in the U.S.: PwC found consumers were delaying treatment for chronic conditions. In October 2020, The American Cancer
Can Telemedicine Increase Health Equity? A Conversation with Antoinette Thomas, Dave Ryan, and Me with the ATA

“Yes,” we concurred on our session convened by the American Telemedicine Association (ATA) EDGE session today. “We” was a trio including Antoinette Thomas (@NurseTechExec1), Chief Patient Experience Officer with Microsoft, David Ryan (@DavidPRyan), former long-time Global Head of Intel’s Health/Life Science business; and, me. Antoinette posed three questions for all of us to brainstorm, addressing various aspects of health equity. We covered, The theory that telemedicine should increase health equity — where are we and what are the barriers to getting there? The role of social determinants of health in creating equitable opportunities for health citizens; and, Entering a post-pandemic world,
Food Trends and Hunger in the Pandemic – the Importance of Food Security in Health and Economic Security
In 2020, the COVID-19 pandemic changed all kinds of aspects of our daily lives, not the least of which were our food habits — how we shopped for food, how we bought food, how we cooked and baked from scratch, and how our tastes and nutritional choices changed with our #StayHome and #WorkFromHome lifestyles. People who could keep their jobs and work from home connected by broadband learned how to build up pandemic pantries, shop online, and stay well-fed. But for people in the U.S. who lost employment, had hours cut, or were compelled to stay home to teach kids
Addressing Lives and Livelihoods with a Whole-of-Government Approach – The First Wave of Biden Health Policy
President Biden’s first few days on the job gave us a very clear view on how he sees conquering COVID: through a whole-of-government approach to public policies that bolster directly addressing the virus, along with the many forces shaping how we got here and how to come out of the pandemic era stronger. I cover this first wave of Biden health policy in my latest post for the Medecision Liberation blog titled, “Top Priorities for President Biden: COVID-19, Then Everything Else.” The plotline goes… On the day of inauguration, January 20, 2021, Joseph R. Biden was installed as the 46th
Ensuring That Humanity Retains Control of Connected Things: A Message from Microsoft at CES 2021

Artificial intelligence (AI) has begun to play a role in health care for predictive analytics, personalization, and public health. On 26th January, I’ll moderate a tweetchat at 1 pm Eastern time, brainstorming the current and future state of and opportunities for AI in health care. I’ll be co-chatting with Microsoft’s AI leader, Tom Lawry (@TCLawry on Twitter). In advance of that discussion, I wanted to feature remarks shared by Brad Smith, Microsoft President, that I recently heard at CES 2021, the annual (this year, virtual) meeting convening the largest community of consumer electronics stakeholders globally Smith wove a crucial, impactful
The Biden Administration’s Whole-of-Government Approach to Equity – in Health and Beyond
In the U.S., the COVID-19 pandemic has revealed disparities in housing, food, and job security, and the role that one’s ZIP code and social determinants play in health outcomes. Overall, America has done poorly in light of being 4% of the world’s population but having one-fifth of the planet’s deaths due to the coronavirus. But these have disproportionately hit non-white people, who are nearly three times as likely to die from COVID-19 than white Americans. I’ve been head-down reviewing the first two days of President Biden’s signing Executive Orders, reading the National Strategy for COVID-19 Response, and inventorying line items
Our Homes Are Health Delivery Platforms – The New Home Health/Care at CES 2021

The coronavirus pandemic disrupted and re-shaped the annual CES across so many respects — the meeting of thousands making up the global consumer tech community “met” virtually, both keynote and education sessions were pre-recorded, and the lovely serendipity of learning and meeting new concepts and contacts wasn’t so straightforward. But for those of us working with and innovating solutions for health and health care, #CES2021 was baked with health goodness, in and beyond “digital health” categories. In my consumer-facing health care work, I’ve adopted the mantra that our homes are our health hubs. Reflecting on my many conversations during CES
Preaching Health Equity in the Era of COVID on Martin Luther King, Jr. Day
Today as we appreciate the legacy of Martin Luther King, Jr., I post a photo of him in my hometown of Detroit in 1963, giving a preliminary version of the “I Have a Dream” speech he would deliver two months later in Washington, DC. Wisdom from the speech: “But now more than ever before, America is forced to grapple with this problem, for the shape of the world today does not afford us the luxury of an anemic democracy. The price that this nation must pay for the continued oppression and exploitation of the Negro or any other minority group is
The Digital Consumer, Increasingly Connected to Health Devices; Parks Associates Kicking Off #CES2021

In 2020, the COVID-19 pandemic drove U.S. consumers to increase spending on electronics, notably laptops, smartphones, and desktop computers. But the coronavirus era also saw broadband households spending more on connecting health devices, with 42% of U.S. consumers owning digital health tech compared with 33% in 2015, according to research discussed in Supporting Today’s Connected Consumer from Parks Associates. developed for Sutherland, the digital transformation company. Consumer electronics purchase growth was, “likely driven by new social distancing guidelines brought on by COVID-19, which requires many individuals to work and attend school from home. Among the 26% of US broadband households
“The virus is the boss” — U.S. lives and livelihoods at the beginning of 2021
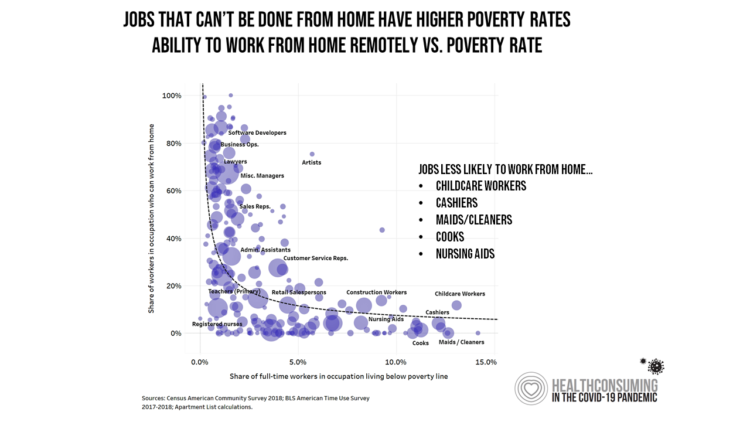
“The virus is the boss,” Austan Goolsbee, former Chair of the Council of Economic Advisers under President Obama, told Stephanie Ruhle this morning on MSNBC. Goolsbee and Jason Furman, former Chair of Obama’s Council of Economic Advisers, tag-teamed the U.S. economic outlook following today’s news that the U.S. economy lost 140,000 jobs — the greatest job loss since April 2020 in the second month of the pandemic. The 2020-21 economic recession is the first time in U.S. history that a downturn had nothing to do with the economy per se. As Uwe Reinhardt, health economist guru, is whispering in my
The 2021 Health Populi TrendCast – Health Care, Self-Care, and the Rebirth of Love in Public Health

In numerology, the symbolic meaning behind the number “21” is death and re-birth. In tarot cards, 21 is a promise of fulfillment, triumph, and victory. How apropos that feels right now as we say goodbye and good riddance to 2020 and turn the page for a kinder, gentler, healthier New Year. It would be sinful to enter a New Year as challenging as 2021 promises to be without taking the many lessons of our 2020 pandemic life and pain into account. For health care in America, it is a time to re-build and re-imagine a better, more equitable landscape for
The Fastest-Growing Brands of 2020 Are All About the Pandemic and Health
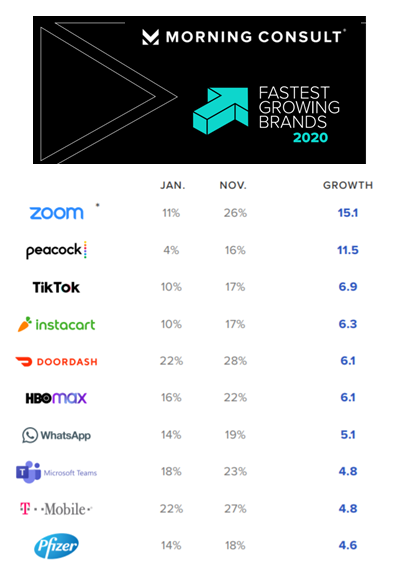
Staying home, being clean, staying entertained, eating well, and self-caring for healthcare….these are the major factors underpinning the twenty fastest-growing brands of 2020, based on Morning Consult’s annual look at the topic. Let’s look into these categories by brand, and connect the dots for health, medical care, and well-being… Connectivity as a social determinant of health. Zoom was the fastest-growing brand of the year, with 26% of U.S. consumers saying they would consider purchasing the service in November compared with 11% in January. Zoom morphed from a business meeting platform to a consumer and family-connecting service spiking on holidays like
The Comforts of Home Drive Demand for Healthcare There
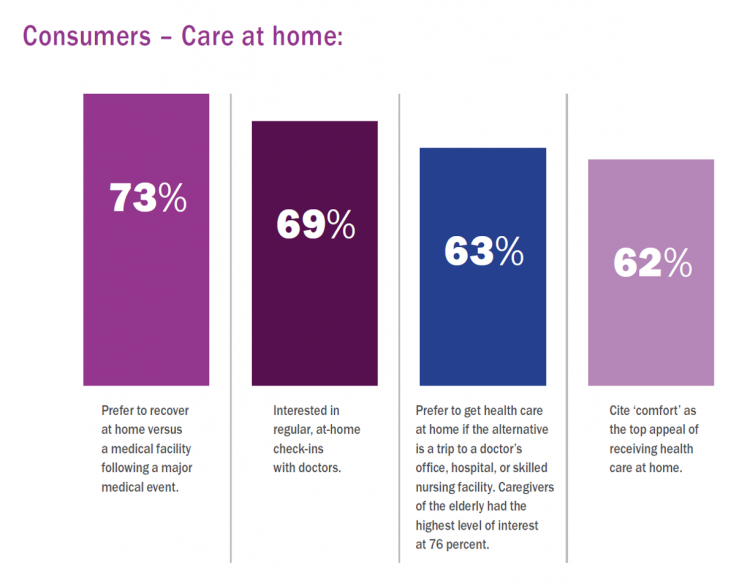
Two in three U.S. consumers skipped or delayed getting in-person medical care in 2020. One in 2 people had a telehealth visit int he last year. Most would use virtual care again. The coronavirus pandemic has mind-shifted how patients envision a health care visit. Today, most consumers prefer the idea of getting health care at home compared with going to a doctor’s office. Most Americans also like the idea of recovering at home instead of at a medical facility after a major medical event, according to the report, Health-at-Home 2020: The New Standard of Care Delivery from CareCentrix. COVID-19 has
Vaccine Hesitancy Is Greatest Among Those at Highest Risk of Dying from COVID-19: Black People
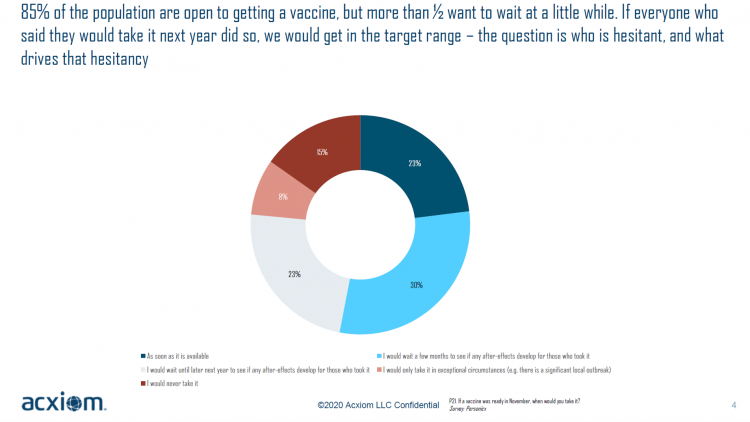
While 85% of people are open to receiving a COVID-19 vaccine, over one-half of them would want to wait some time to observe if after-effects developed in people who took the jab, according to a new study from Acxiom, the data analytics-marketing company. Not all people are as enthused about getting a coronavirus vaccine at all, Acxiom discovered: in fact, those hardest hit by the virus — Black people — would be the least-likely to want to get a COVID-19 vaccine, discussed in in Vaccine Hesitancy in the U.S., a survey the company conducted among 10,000 people in the U.S.
The COVID Healthcare Consumer – 5 Trends Via The Medecision Liberation Blog
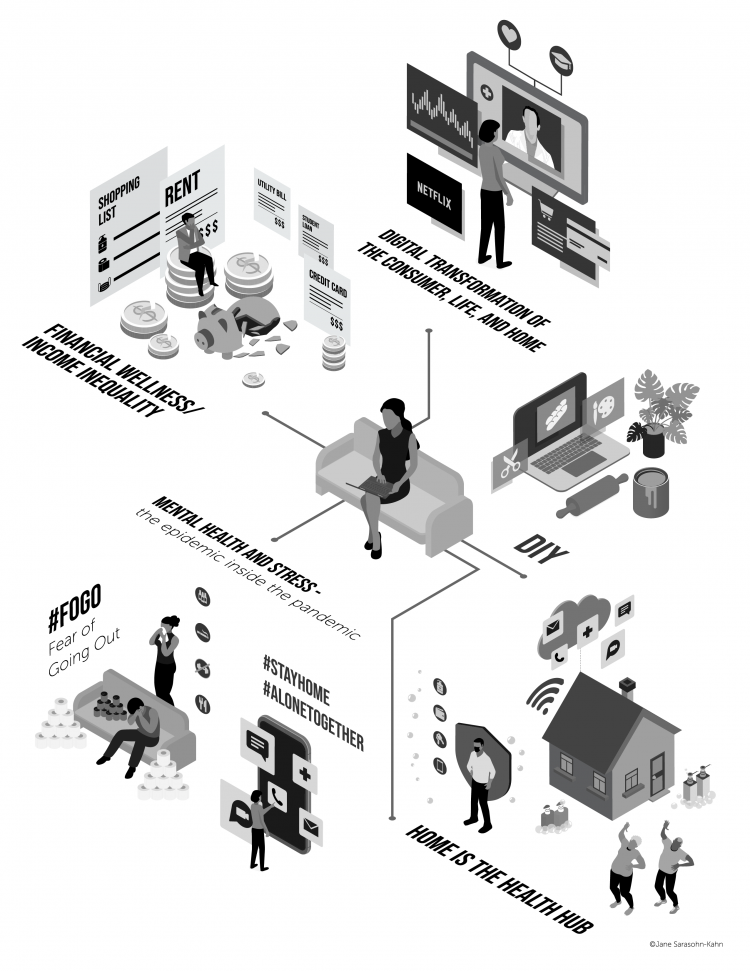
The first six months into the coronavirus pandemic shocked the collective system of U.S. consumers for living, learning, laboring, and loving. I absorbed all kinds of data about consumers in the wake of COVID-19 between March and mid-August 2020, culminating in my book, Health Citizenship: How a virus opened hearts and minds, published in September on Kindle and in print in October. In this little primer, I covered the five trends I woven based on all that data-immersion, following up the question I asked at the end of my previous book, HealthConsuming: when and how would Americans claim their health
The Pandemic Has Been a Shock to Our System – Learning from Known
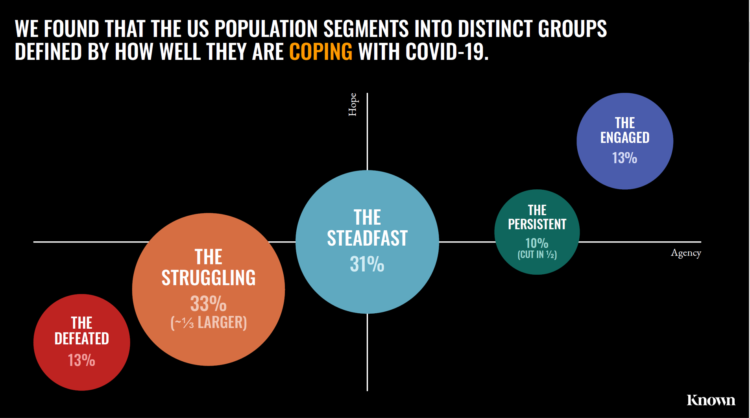
The coronavirus pandemic has been a shock to people across all aspects of everyday living, for older and younger people, for work and school, for entertainment and travel — all impacting our hearts, minds, and wallets. “As the bedrock of daily life was shaken, uncertainty predictably emerged as the prevailing emotion of our time but this universal problem was eliciting a highly differentiated reaction in different people,” Kern Schireson, CEO of Known, observed. His company has conducted a large quantitative and qualitative research program culminating in a first report, The Human Condition 2020: A Shock To The System. Known’s team of
Rebuilding Resilience, Trust, and Health – Deloitte’s Latest on Health Care and Sustainability
The COVID-19 pandemic has accelerated health care providers’ and plans’ investment in digital technologies while reducing capital spending on new physical assets, we learn in Building resilience during the COVID-19 pandemic and beyond from the Deloitte Center for Health Solutions. What must be built (or truly re-built), health care leaders believe, is first and foremost trust, followed by financial viability to ensure long-term resilience and sustainability — for the workforce, the organization, the community, and leaders themselves. For this report, Deloitte interviewed 60 health care chief financial officers to gauge their perspectives during the pandemic looking at the future of
Voting for Health in 2020

In the 2018 mid-term elections, U.S. voters were driven to polls with health care on their minds. The key issues for health care voters were costs (for care and prescription drugs) and access (read: protecting pre-existing conditions and expanding Medicaid). Issue #2 for 2018 voters was the economy. In 2020, as voting commences in-person tomorrow on 3rd November, U.S. voters have lives and livelihoods on their minds. It’s the pandemic – our physical lives looming largest in the polls – coupled with our fiscal and financial lives. Health is translating across all definitions for U.S. voters in November 2020: for
How Grocery Stores Are Part of the Health/Care Ecosystem – the Case of ALDI and Instacart
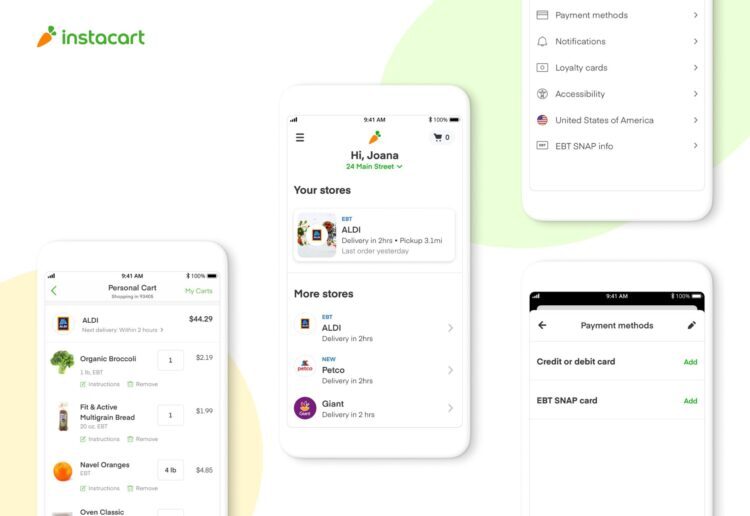
As humans in the Age of the Coronavirus focus on physiological needs, people have intensely focused on hunting-and-gathering food and hygiene products. We will remember memes about toilet tissue stockpiling and re-visiting canned and shelf-stable comfort foods from childhood long after the pandemic. Some people, though, haven’t had easy access to nutritious food in their communities or the ability to engage with ecommerce platforms to order food for delivery. An alliance between ALDI, the value-priced grocer, and Instacart, was forged to address that gap as a key social determinant of health. Food-is-medicine when it comes to managing chronic conditions like
Health Care Providers Are More Politically Engaged in the 2020 Elections
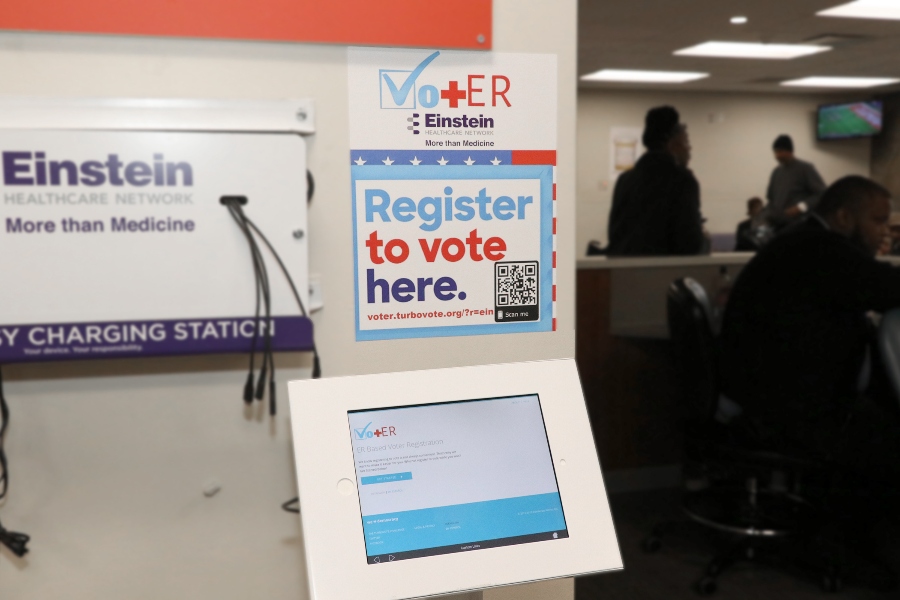
Until 2016, physicians’ voting rates in U.S. elections had not changed since the late 1970s. Then in 2018, two years into President Donald Trump’s four-year term, the mid-term elections drove U.S. voters to the election polls…including health care providers. Based on the volume and intensity of medical professional societies’ editorials on the 2020 Presidential Election, we may be in an inflection-curve moment for greater clinician engagement in politics as doctors and nurses take claim of their health citizenship. A good current example of this is an essay published in the AMA’s website asserting, “Why it’s okay for doctors to ask
Women’s Health Policy Advice for the Next Occupant of the White House: Deal With Mental Health, the Pandemic, and Health Care Costs
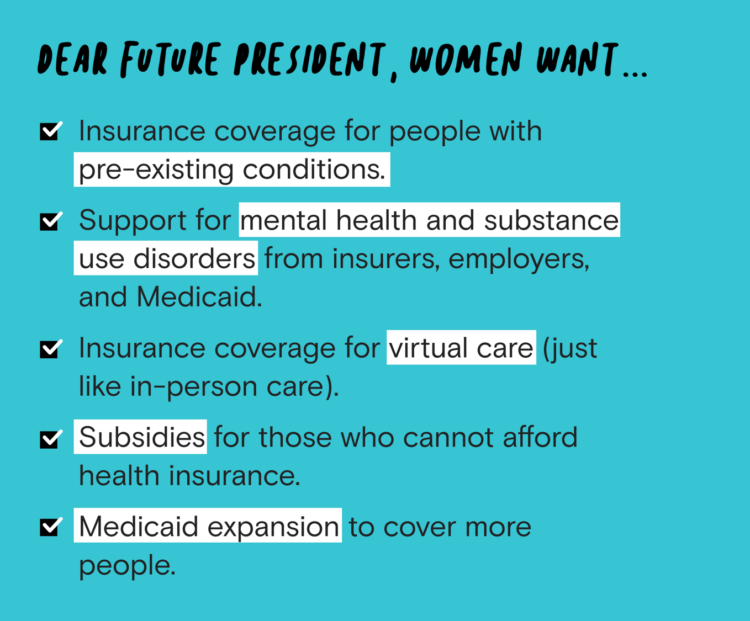
2020 marked the centennial anniversary of the 19th Amendment to the U.S. Constitution, giving women the right to vote. In this auspicious year for women’s voting rights, as COVID-19 emerged in the U.S. in February, women’s labor force participation rate was 58%. Ironic timing indeed: the coronavirus pandemic has been especially harmful to working women’s lives, the Brookings Institution asserted last week in their report in 19A: The Brookings Gender Equality Series. A new study from Tia, the women’s health services platform, looks deeply into COVID-19’s negative impacts on working-age women and how they would advise the next occupant of
Black Health Should Matter More in America: The Undefeated Survey on Race and Health
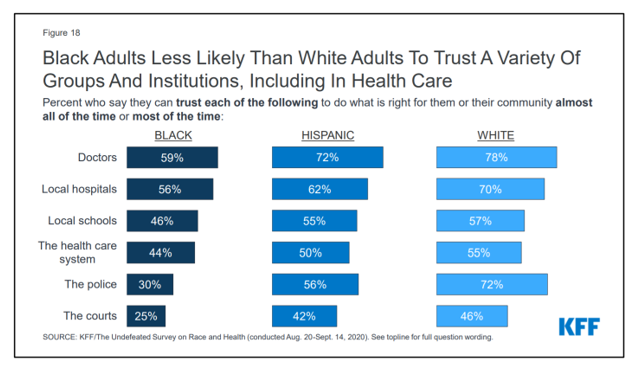
In 2020, most Black people, men and women alike, feel it is a bad time to be Black in America. More than twice as many Black men believed that in 2020 compared with 2006. More than four times as many Black women believed that it’s a bad time to be Black in America in 2020 versus 2011, we learn in The Undefeated Survey on Race and Health from Kaiser Family Foundation (KFF). KFF collaborated with The Undefeated, ESPN’s project that focuses on sports, race, and culture. The Undefeated program was started in May 2016, and has become a thought leader
Social Determinants of Health Travel in Groups – At the Root Is Household Income
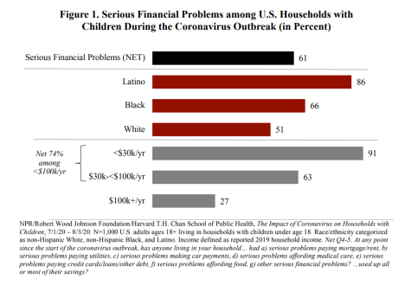
The U.S. health care community is collectively embracing the concept of social determinants of health that have become so obvious in understanding the disparities of health outcomes wrought by the coronavirus pandemic. Research from the Harvard Chan School of Public Health conducted with the Robert Wood Johnson Foundation and NPR illustrates the fact that people who are at risk for one social determinant of health tend to be challenged by a bucket of them. The survey research reported in The Impact of Coronavirus on Households With Children, published on 30th September, found that 61% of U.S. households with children had
Our Home Is Our Health Hub: CTA and CHI Align to Address Digital and Health Equity

In the pandemic, I’ve been weaving together data to better understand how people as consumers are being re-shaped in daily life across their Maslow Hierarchies of Needs. One of those basic needs has been digital connectivity. People of color have faced many disparities in the wake of the pandemic: the virus itself, exacting greater rates of mortality and morbidity being the most obvious, dramatic inequity. Another has been digital inequity. Black people have had a more difficult time paying for phone and Internet connections during the COVID-19 crisis, we learned in a Morning Consult poll fielded in June 2020. In
Redefining PPE As Primary Care, Public Health, and Health Equity – The Community PPE Index
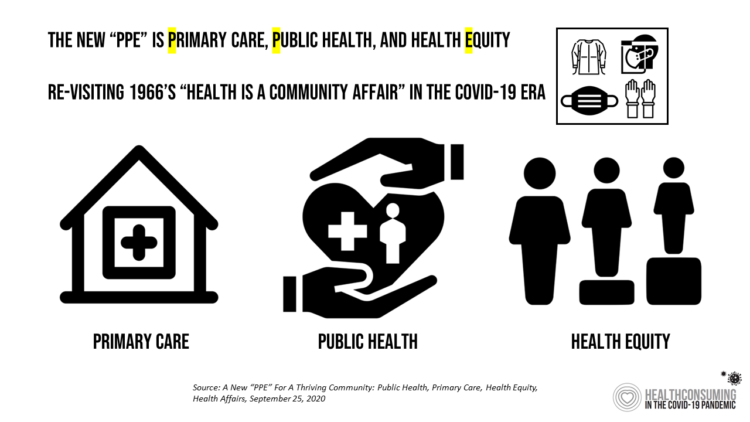
In May 2020, the Oxford English Dictionary (OED) re-visited the acronym, “PPE.” As OED evolves the definition of PPE, the wordsmiths could borrow from OSHA’s website, noting that PPE, “is equipment worn to minimize exposure to hazards that cause serious workplace injuries and illnesses. These injuries and illnesses may result from contact with chemical, radiological, physical, electrical, mechanical, or other workplace hazards. Personal protective equipment may include items such as gloves, safety glasses and shoes, earplugs or muffs, hard hats, respirators, or coveralls, vests and full body suits.” Perhaps Definition 3 in the OED could be updated by a blog
Older People Are Digital Immigrants, and Best Buy Health Is Paving the Road for the Journey

The coronavirus pandemic has revealed the importance of connectivity, WiFi, broadband, as a social determinant of health and living. Connecting from our homes — now our health hubs, workplaces, schools, entertainment centers, and gyms — is necessary like air and water for survival across daily life flows. Digital connectivity can ameliorate social isolation and anxiety, bolster mental health, and access needed medical care via telehealth channels. As a result of the pandemic, staying connected is more important than ever for older people, Best Buy Health learned in a survey of U.S. adults. Insights from this study have informed the launch
Health Citizenship in America. If Not Now, When?
On February 4th, 2020, in a hospital in northern California, the first known inpatient diagnosed with COVID-19 died. On March 11th, the World Health Organization called the growing prevalence of the coronavirus a “pandemic.” On May 25th, George Floyd, a 46-year-old Black man, died at the hands of police in Minneapolis. This summer, the Dixie Chicks dropped the “Dixie” from their name, and NASCAR cancelled the confederate flag from their tracks. Today, nearly 200,000 Americans have died due to the novel coronavirus. My new book, Health Citizenship: How a virus opened hearts and minds, launched this week. In it, I
Only in America: The Loss of Health Insurance as a Toxic Financial Side Effect of the COVID-19 Pandemic

In terms of income, U.S. households entered 2020 in the best financial shape they’d been in years, based on new Census data released earlier this week. However, the U.S. Census Bureau found that the level of health insurance enrollment fell by 1 million people in 2019, with about 30 million Americans not covered by health insurance. In fact, the number of uninsured Americans rose by 2 million people in 2018, and by 1.9 million people in 2017. The coronavirus pandemic has only exacerbated the erosion of the health insured population. What havoc a pandemic can do to minds, bodies, souls, and wallets. By September 2020,
Behavioral Health Side-Effects in the COVID Era
“This surge of people experiencing acute behavioral health problems…has the potential to further impact the healthcare system for years to come,” a report from McKinsey expects looking at the hidden costs of COVID-19’s impact on U.S. health care. The coronavirus pandemic has taken a toll on Americans’ mental health, with anxiety and depression growing as a side-effect to worries about the virus itself, the long Great Lockdown in much of the country, and the economic recession that has particularly impacted women and people of color. I covered depression impacts due to COVID-19 here in Health Populi yesterday, and wanted to
The Burden of Depression in the Pandemic – Greater Among People With Fewer Resources
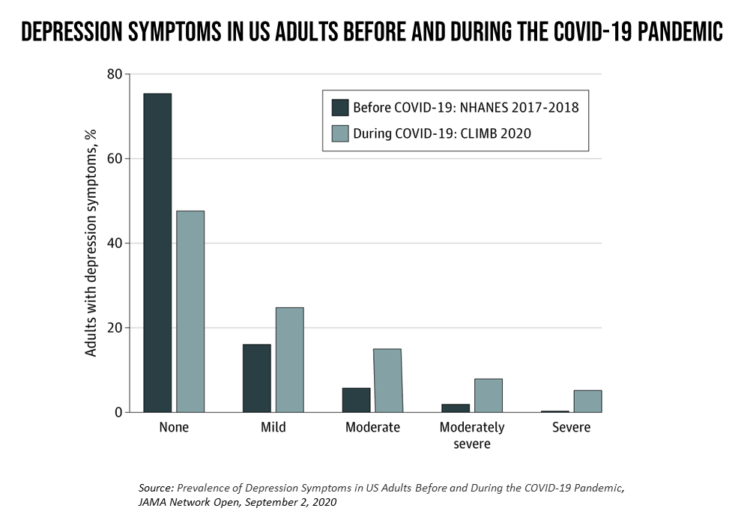
In the U.S., symptoms of depression were three-times greater in April 2020 in the COVID-19 pandemic than in 2017-2018. And rates for depression were even higher among women versus men, along with people earning lower incomes, losing jobs, and having fewer “social resources” — that is, at greater risk of isolation and loneliness. America’s health system should be prepared to deal with a “probable increase” in mental illness after the pandemic, researchers recommend in Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic in JAMA Network Open. A multidisciplinary team knowledgeable in medicine, epidemiology, public health,
Health Happens at Home: Lessons from the Parks Connected Health Summit

Home is where the health is, we know in the wake of the COVID-19 pandemic. To be sure, many of us who have been preaching that our ZIP codes are more impactful to our health than our genetic codes have known the evidence backing the social and behavioral determinants of health for a long time. This week, Parks Associates convened the Connected Health Summit, focused on the theme of consumer engagement and innovation. I attended all three days’ worth of sessions in this well-planned and -executed virtual meeting. In this post, I’ll weave my favorite themes of consumer health engagement
My ABCovid-19 Journal – Day 4 of 5, Letters “P” through “T”
While I’m on holiday this week, restoring and re-setting, I’ve been sharing pages from my ABCovid-19 Journal with readers of Health Populi. I created this journal during the early phase of the pandemic in the U.S., as a form of art therapy, creative outlet, and learning. Today is Day 4 of sharing: we consider the letters “P” through “T,” and what I saw in the early coronavirus era. P is for pandemic This “P” was self-evidence in our collective early COVID-19 lexicon. The “P” word was uttered by the Secretary General of the World Health Organization on March 11, confirming
The She-Cession – a Financially Toxic Side-Effect of the Coronavirus Pandemic
Along with the life-threatening impact of the coronavirus on physical health, and the accompanying mental health distress activated by self-distancing comes a third unintended consequence with the pandemic: a hard hit on women’s personal economies. The recession of the pandemic is considered by many economists as a “She-Cession,” a downturn in the economy that’s negatively impacting women more acutely than men. This is markedly different than the Great Recession of 2008, the last major financial crisis: that financial decline was coined a “ManCession,” taking a more significant toll out of more typically men’s jobs like construction and manufacturing where fewer
The Racial Divide Due to COVID-19 Also Applies to Healthcare and Pharma Costs
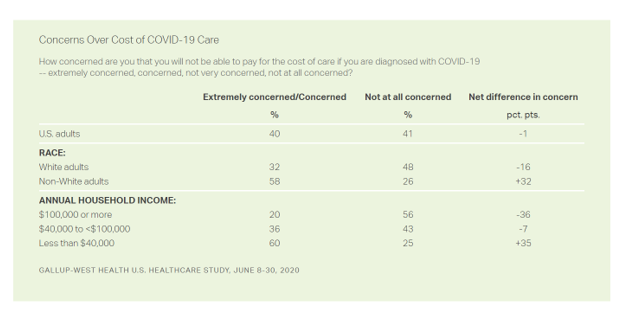
Into the sixth month of the coronavirus pandemic in the U.S., it’s clear that COVID-19 has wreaked a greater mortality and morbidity impact on people of color than on white adults. A new Gallup-West Health poll found that the coronavirus also concerns more non-white Americans than whites when it comes to the cost of health care and medicines to deal with the effects of COVID-19. Considering the cost of COVID-19 treatment, across all U.S. adults, 40% of people are concerned (extremely/concerned), and 41% are “not at all concerned.” Broken down by race, there is a stark difference in levels of
We Are All About Hygiene, Groceries, and Personal Care in the Midst of the Coronavirus Pandemic
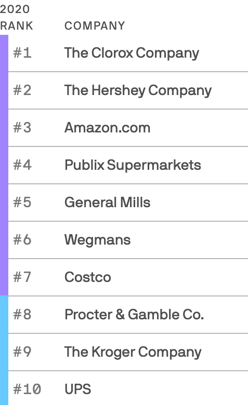
Pass me the Clorox…tip the UPS driver…love thy grocer. These are our daily life-flows in the Age of COVID-19. Our basic needs are reflected in the new 2020 Axios-Harris Poll, released today. For the past several years, I’ve covered the Harris Poll of companies’ reputation rankings here in Health Populi. Last year, Wegmans, the grocer, ranked #1; Amazon, #2. In the wake of the COVID-19 pandemic, U.S. consumers’ basic needs are emerging as health and hygiene, food, and technology, based on the new Axios-Harris Poll on the top 100 companies. This year’s study was conducted in four waves, with the
The Unbearable Heaviness of Healthcare in America – the Change Healthcare/Harris Poll
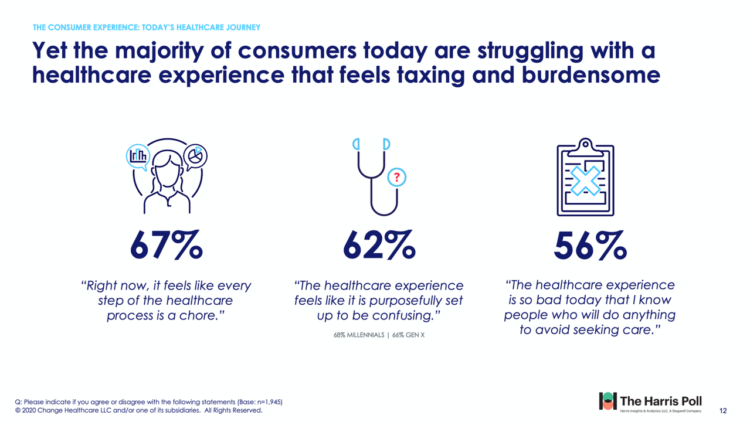
The phrase, “burden of health care,” has two usual meanings: one, to do with the massive chronic care burden, and the other, involving costs. There’s a third area of burden in U.S. health care — the onerous patient experience in finding and accessing care, assessed in the 2020 Change Healthcare – Harris Poll Consumer Experience Index. Two in three U.S. consumers feel like “every step of the healthcare process is a chore.” That burdensome patient experience leads to one in two people in America avoiding seeking care, the poll found. That’s not just self-rationing health care due to costs, but due
Return-To-School Is Stressing Out U.S. Parents Across Income, Race and Political Party
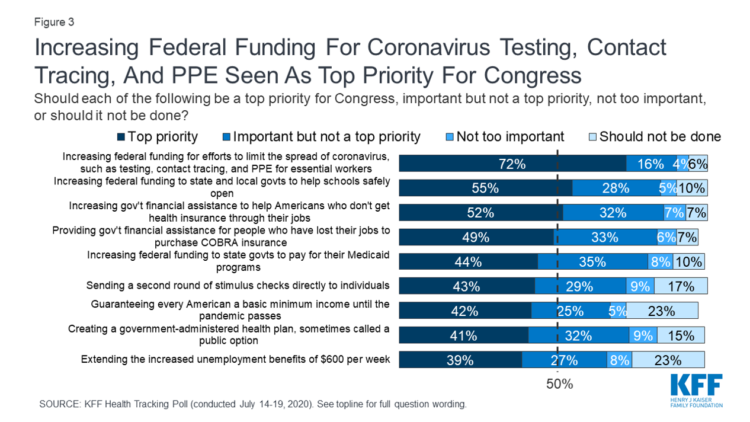
The worse of the coronavirus pandemic is yet to come, most Americans felt in July 2020. That foreboding feeling is shaping U.S. parents’ concerns about their children returning to school, with the calendar just weeks away from educators opening their classrooms to students, from kindergarten to the oldest cohort entering senior year of high school. The Kaiser Family Foundation’s July 2020 Health Tracking Poll focuses on the COVID-19 pandemic, return-to-school, and the governments’ response. KFF polled 1,313 U.S. adults 18 and older between July 14 to 19, 2020. The first line chart illustrates Americans’ growing concerns about the coronavirus, shifting
More Americans Pivot to Distancing and Mask-Wearing in the Hot Summer of 2020
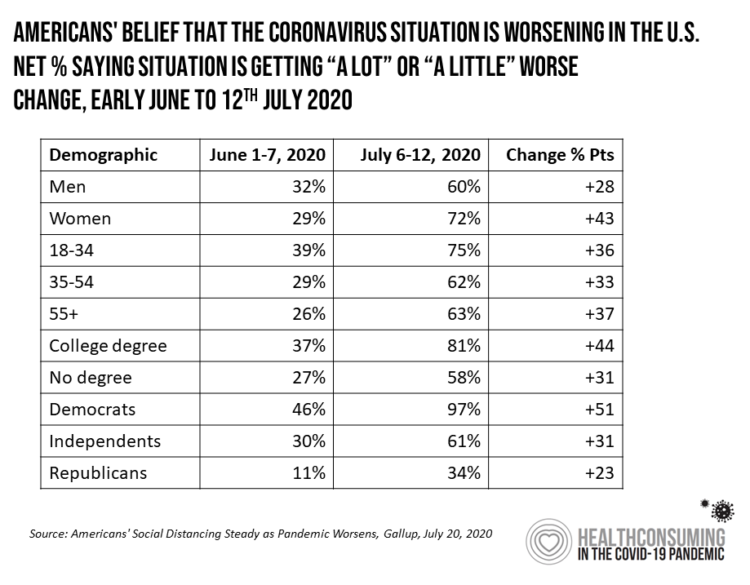
With growing coronavirus case hotspots in southern and western states, more Americans perceive the pandemic is worsening this summer, shown by a Gallup poll published 20 July 2020. Gallup titles the analysis, Americans’ social distancing steady as pandemic worsens. The first table organizes Gallup’s data by demographics, illustrating a significant gap between how women perceive the exacerbating pandemic compared with men. In early June, roughly one-third of both men and women saw COVID-19 was getting “worse”; five weeks later, in the second week of July, men and women’s perceptions were 12 points apart with more women concerned about the situation
The Median Hospital Charge In the U.S. for COVID-19 Care Ranges From $34-45K
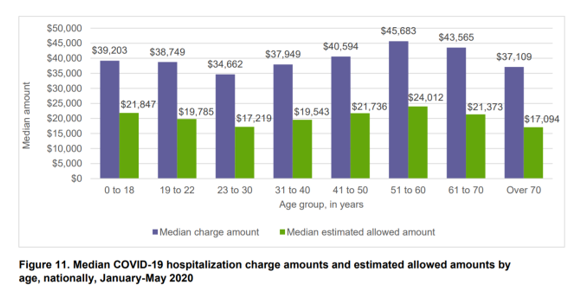
The median charge for hospitalizing a patient with COVID-19 ranged from $34,662 for people 23 to 30, and $45,683 for people between 51 and 60 years of age, according to FAIR Health’s research brief, Key Characteristics of COVID-19 Patients published July 14th, 2020. FAIR Health based these numbers on private insurance claims associated with COVID-19 diagnoses, evaluating patient demographics (age, gender, geography), hospital charges and estimated allowed amounts, and patient comorbidities. They used two ICD-10-CM diagnostic codes for this research: U07.1, 2019-nCoV acute respiratory disease; and, B97.29, other coronavirus as the cause of disease classified elsewhere which was the original code
A Toxic Side Effect of the Coronavirus: Financial Unwellness
One in two people in the U.S. say their financial health has been negatively impacted by the COVID-19 pandemic, through job loss, income disruption, or reduced work hours. The 2020 Financial Wellness Census, from Prudential found that one-half of U.S. adults are anxious about their financial future as of May 2020, an increase from 38% in late 2019. Prudential surveyed 3,000 U.S. adults across three generational cohorts: Millennials, Gen X, and Baby Boomers. The economic hit from the pandemic has disproportionately impacted people of color, younger people, women, small business owners, gig workers, and people working in retailer harder than
Beyond Care and Outcomes, Hospitals Must Deliver on Civics, Inclusivity, Equity, and Value – Lown Institute’s Best Hospitals
The core business of hospitals is patient care, often baked with teaching and research. But wait — there’s more, asserts the Lown Institute in their approach to ranking America’s Best Hospitals in 2020. The Institute’s methodology for assessing what’s “best” addresses ten pillars. Several of these are the “stick-to-the-knitting” components of the Webster Dictionary definition of hospital work: patient outcomes, clinical outcomes, avoiding overuse, patient safety, and a recent focus, patient satisfaction. Community benefit has been part of a hospital’s life, especially in the not-for-profit world where hospitals must demonstrate goodwill generated for and provided in the neighborhoods in which
Health Insurance and Demand for Masking, Testing and Contact Tracing – New Data from The Commonwealth Fund
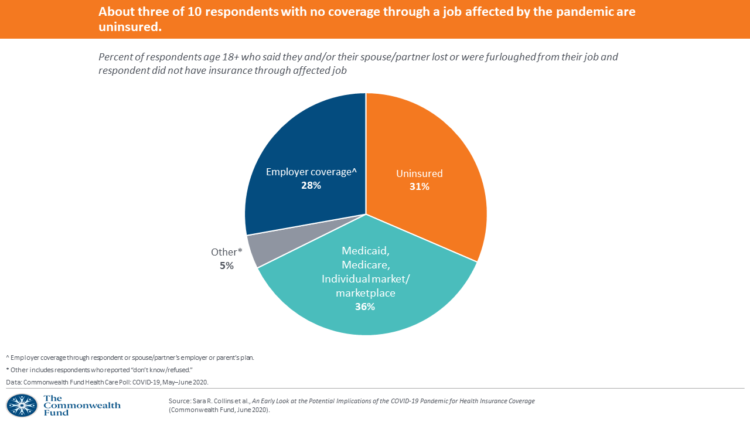
The coronavirus pandemic occasioned the Great Lockdown for people to shelter-at-home, tele-work if possible, and shut down large parts of the U.S. economy considered “non-essential.” As health insurance for working-age people is tied to employment, COVID-19 led to disproportionate loss of health plan coverage especially among people earning lower incomes, as well as non-white workers, explained in the Commonwealth Fund Health Care Poll: COVID-19, May-June 2020. The Commonwealth Fund commissioned interviews with 2,271 U.S. adults 18 and over between 13 May and 2nd June 2020 for this study. The survey has two lenses: first, on health insurance coverage among working
How Can Healthcare Bring Patients Back? A Preview of Our ATA Session, “Onward Together” in the COVID Era

Today kicks off the first all-virtual conference of the ATA, the American Telemedicine Association. ATA’s CEO Ann Mond Johnson and team turned on a dime over the past few months, migrating the already-planned live conference scheduled in early May to this week, all online. I’ll be midwifing a panel this afternoon at 440 pm Eastern time, initially focused on how health care can garner patient loyalty. That theme was given to us in the fourth quarter of 2019, when initial planning for ATA 2020 had begun. What a difference a few months make. Not only has ATA pivoted to an
Juneteenth 2020: Inequality and Injustice in Health Care in America
“Of all the forms of inequality, injustice in health is the most shocking and the most inhuman because it often results in physical death,” Martin Luther King, Jr., asserted at the second meeting of the Medical Committee for Human Rights in Chicago on March 25, 1966. This quote has been shortened over the five+ decades since Dr. King told this truth, to the short-hand, “Of all the forms of inequality, injustice in health care is the most shocking and inhumane.” Professor Charlene Galarneau recently enlightened me on Dr. King’s original statement in her seminal essay, “Getting King’s Words Right.” Among
Economic Anxieties Rise, Medical and Vacation Plans Delayed: the COVID-19 Consumer in June 2020
Some 6 in 10 people in the U.S. have been financially impacted by COVID-19. Those most negatively affected by the pandemic tend to be younger, Gen Z age group and African-American, 63% of whom felt financial pressure directly due from the virus and the national economic lockdown. By late May 2020, 34% of black Americans had lost their jobs compared with 21% in late April, compared with 18% of white consumers, reported in The COVID-19 Pandemic’s Financial Impact on U.S. Consumers, survey research from TransUnion. This post describes data from TransUnion’s Wave 9 report, which polled 2,086 U.S. adults 18
Americans’ Concerns About the US Healthcare System Loom Larger Than Worries About Their Own Care
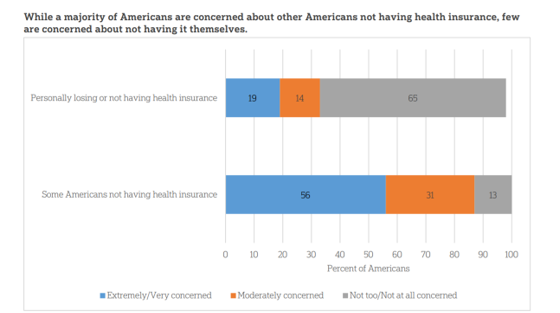
The coronavirus pandemic has further opened the kimono of the U.S. healthcare system to Americans: four months into the COVID-19 outbreak, most consumers (62%) of people in the U.S. are more concerned about other people not having access to high quality health care versus themselves. This is a 16 point increase in concern in May 2020 compared with the response to the same question asked in February in a poll conducted by the University of Chicago Harris School of Public Policy and The Associated Press-NORC Center for Public Affairs Research (the AP-NORC Center). The AP-NORC Poll found more of this
Addressing Health Equity Must Include Digital Equity Beyond Access To Medical Services and Insurance
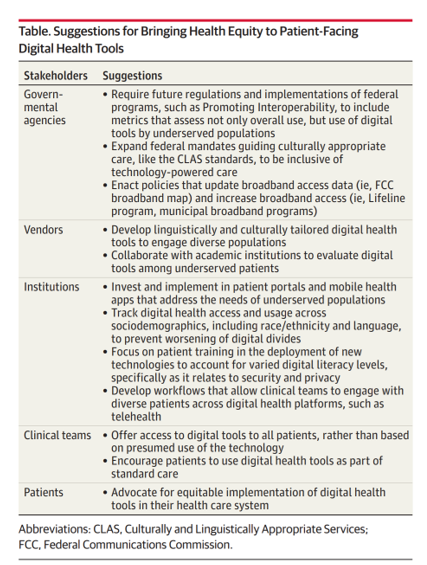
The 21st Century Cures Act emphasizes patients’ control of personal health information. ONC rules issues in March 2020 called for more patient-facing health tools and apps to bolster health consumer engagement and empowerment. But the emergence of the coronavirus in the U.S. revealed many weakness in the American health care system, one of which has been health inequities faced by millions of people — especially black Americans, who have sustained higher rates morbidity and mortality for COVID-19. There have also been digital health divides found in the COVID-19 pandemic, discussed in a timely essay in JAMA, Digital Health Equity as
Big Hearts, High Tech – How Caregiving Has Changed in the U.S.
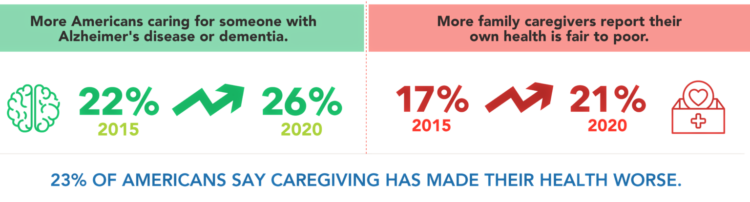
We are all caregivers now. The COVID-19 pandemic has touched and continues to re-shape our daily lives. One reality that the coronavirus era has revealed is that caregiving is a daily life-flow for everyone around the world. In the U.S., this has particularly acute impacts — physical, emotional, and financial. The 2020 AARP report on caregiving was published this month, and the survey research into caregivers uncovered fresh insights about caregivers’ demographics, financial stressors, and intensity of tasks both in volume and time. In addition, more caregivers are looking for and turning to technology to help them hack effort, time
Stress in America – COVID-19 Takes Toll on Finances, Education, Basic Needs and Parenting

“The COVID-19 pandemic has altered every aspect of American life, from health and work to education and exercise,” the new Stress in America 2020 study from the American Psychological Association begins. The APA summarizes the impact of these mass changes on the nation: “The negative mental health effects of the coronavirus may be as serious as the physical health implications,” with COVID-19 stressors hitting all health citizens in the U.S. in different ways. Beyond the risk of contracting the virus, the Great Lockdown of the U.S. economy has stressed the U.S. worker and the national economy, with 7 in 10
How COVID-19 Is Driving More Deaths of Despair
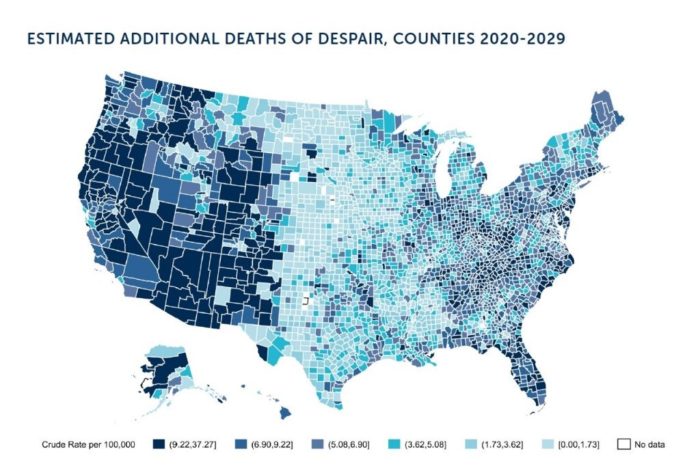
In the current state of the COVID-19 pandemic, we all feel like we are living in desperate times. If you are a person at-risk of dying a Death of Despair, you’re even more at-risk of doing so in the wake of the Coronavirus in America. Demonstrating this sad fact of U.S. life, the Well Being Trust and Robert Graham Center published Projected Deaths of Despair from COVID-19. The analysis quantifies the impact of isolation and loneliness combined with the dramatic economic downturn and mass unemployment with the worsening of mental illness and income inequity on the epidemic of Deaths of
Food In-Security in a Coronavirus America
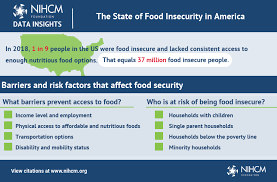
One in 10 people in the U.S. were defined as food-insecure without consistent access to nutritious food options in 2019. The COVID pandemic has quickly and negatively impacted food insecurity in America, detailed in an assessment from NIHCM on the current state of food insecurity in America. As many as 4 in 10 U.S. households reported being food-insecure as of April 2020. That includes 20% of children living in the U.S. lacking nutritious food on a daily basis. The NIHCM adopted the definition of food insecurity from the USDA Adult Food Security Survey which is a 10-question poll asking people
TransUnion Reveals the Home Economics and Social Determinants of COVID-19
Today, 7th May 2020, the U.S. Bureau of Labor Statistics announced that about 3.17 million jobs were lost in the nation in the last week. This calculated to an unemployment rate of 15.5%, an increase of 3.1% points from the previous week. Total jobs lost in the COVID-19 pandemic, starting from the utterance of the “P” word, has been ___ in the I.S. The virus’s global impact has led to what IMF called the Great Lockdown, resulting in economic inertia and contraction since Asia and Europe reported the first patients diagnosed with the coronavirus. The economic impact the world
Food, Housing, Energy and Medical Care – the Material Hardships of COVID-19 in America
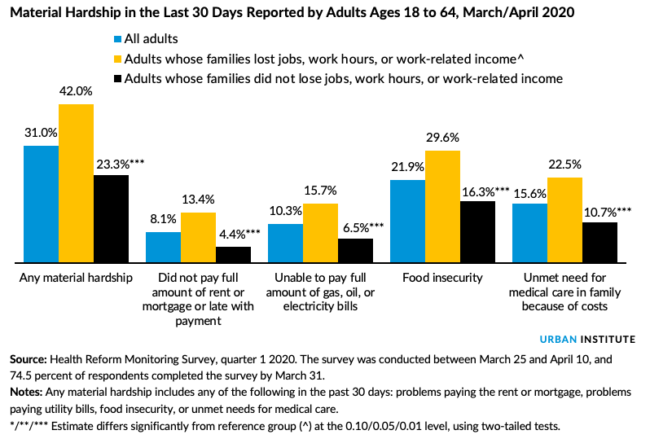
The Coronavirus has impacted every aspect of human life: first, the direct biological impact of COVID-19 on people, as of today the cause of over 63,000 deaths in the U.S. along with unquantifiable morbidity among millions of Americans who are surviving the virus and the toll on family caregivers. Beyond the direct physical impact of the virus, social and emotional health impacts are emerging now due to physical distancing, mandates to #StayHome, and telecommuting to jobs when possible. Mental health impacts will persist as a pandemic after the Coronavirus pandemic, I’ve previously detailed here in Health Populi. On a global




 I am gratified and grateful for my Health Populi blog to be named #1 by Feedspot in the category of
I am gratified and grateful for my Health Populi blog to be named #1 by Feedspot in the category of  Jane will deliver the keynote address at the upcoming
Jane will deliver the keynote address at the upcoming  Thank you, Jared Johnson, for including me on the list of the
Thank you, Jared Johnson, for including me on the list of the