Data Privacy and Healthcare Access: Top Issues Shaping Consumers’ Societal ROI

Organizations that address consumers’ data privacy and access to healthcare create greater social brand equity, inspiring people to say nice things about the companies, recommend them as good employers, and be welcomed as businesses operating in peoples’ community. In The Societal ROI Index: A Measure for The Times We Find Ourselves In, Finn Partners and The Harris Poll measure U.S. companies’ reputations for social good, the project’s press release explains. “Our new data shows that the public has a definite opinion about what issues they feel companies should address and the social impact bar has been set high,” according to Amy Terpeluk,
Financial Stress Is An Epidemic In America, Everyday Health Finds

One in three working-age people in the U.S. have seen a doctor about something stress-related. Stress is a way of American life, based on the findings in The United States of Stress, a survey from Everyday Health. Everyday Health polled 6,700 U.S. adults between 18 and 64 years of age about their perspectives on stress, anxiety, panic, and mental and behavioral health. Among all sources of stress, personal finances rank as the top stressor in the U.S. Over one-half of consumers say financial issues regularly stress them out. Finances, followed by jobs and work issues, worries about the future, and relationships cause
Loneliness, Public Policy and AI – Lessons From the UK For the US

There’s a shortage of medical providers in the United Kingdom, a nation where healthcare is guaranteed to all Britons via the most beloved institution in the nation: The National Health Service. The NHS celebrated its 70th anniversary in July this year. The NHS “supply shortage” is a result of financial cuts to both social care and public health. These have negatively impacted older people and care for people at home in Great Britain. This article in the BMJ published earlier this year called for increasing these investments to ensure further erosion of population and public health outcomes, and to prevent
CVS + Aetna: Inflection Point in US Healthcare, Merger Approved Update

CVS Health’s acquisition of Aetna was approved this week by U.S. Federal regulators after months of scrutinizing the antitrust-size-market control implications of the deal. I wrote this post on the deal as an inflection point in American healthcare on 3rd December 2017 when CVS and Aetna announced their marriage intentions. This post updates my initial thoughts on the deal, given the morphing US healthcare market on both the traditional health services front and fast-evolving retail health environment. The nation’s largest retail pharmacy chain signed a deal to combine with one of the top three health insurance companies. The deal
Most U.S. Physicians, Burned Out, Favor A Flavor of Single Payer Health System

Most physicians feel some level of burnout, hassled by electronic health records and lost autonomy. No wonder, then, that a majority of doctors favor some type single payer health system — one-quarter fully single payer, a la Britain’s National Health Service; and another one-third a single payer combined with a private insurance option, discovered in the 2018 Survey of America’s Physicians report on practice patterns & perspectives, published by The Physicians Foundation. Eight in ten physicians are working at full-capacity or are over-extended, the survey found. Furthermore, 62% of doctors are pessimistic about the future of medicine. Physician burnout is a
The Health Consumer Seeks Fresh, Free-From and…Turmeric

The impact of health and wellness is on most consumers’ minds, Nielsen’s consumer research has found. Sarah Schmansky, Nielsen’s strategy leader for health, wellness and “fresh,” moderated a panel at the GMDC Health-Beauty-Wellness Conference in Orlando today that brainstormed how consumers are shopping for health. Underneath that “how” is more than the next-best-me-too-product for allergy or acne. It’s about efficacy of the product at the core, but bundled with social responsibility and sustainability, informative packaging, transparency of ingredients, and education that empowers the individual. “Self-care is the driver of growth,” Sarah began the discussion. But these needs under the self-care umbrella
Disruption Is Healthcare’s New Normal
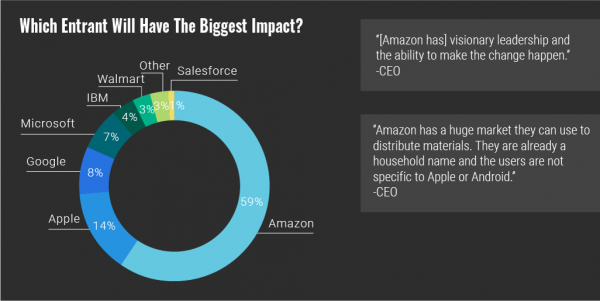
Googling the words “disruption” and “healthcare” today yielded 33.8 million responses, starting with “Riding the Disruption Wave in Healthcare” from Bain in Forbes, Accenture’s essay on “Big Bang Disruption in Healthcare,” and, “A Cry for Encouraging Disruption” in the New England Journal of Medicine Catalyst. This last article responded to the question, “Can we successfully deliver better quality care for patients at a lower cost?” asked by François de Brantes, Executive Director of the Health Care Incentives Improvement Institute. “Disruption” as a noun and an elephant in our room has been with us in healthcare since the September/October 2000 issue of
Healthcare’s Profits Will Be Dramatically Redistributed as Care Shifts to Consumers: Accenture
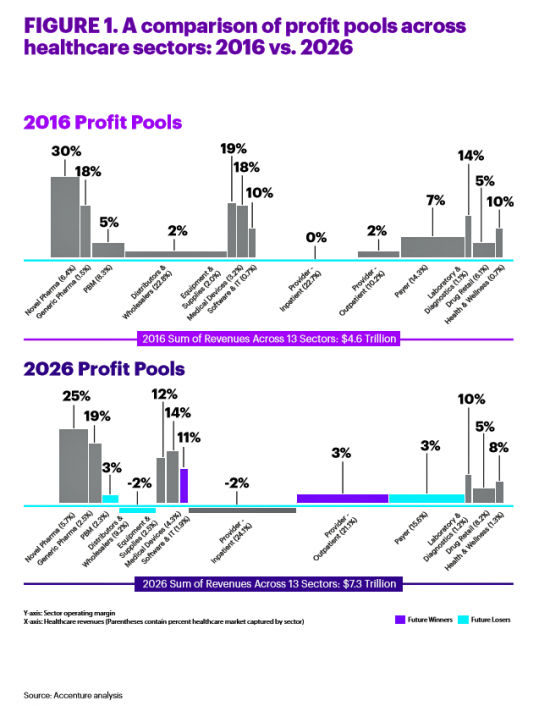
All sectors who are stakeholders in the healthcare ecosystem aren’t created equal, Accenture explains in their report, Healthcare’s future winners and losers. Observing the influx of new flavors of entrants like Amazon and Google, start-ups like Iora Health, Oscar and FetchMD, begs the question: how will legacy healthcare system players fare? Who will survive, and what will be the success factors that bolster long-term viability? To answer that question, Accenture points to three market trends that set “new rules” in healthcare: Blurred lines, which are the grey areas and adjacencies between technology, service, finance, and retail The middle of nowhere,
“Lower Prescription Drug Prices” – A Tri-Partisan Call Across America
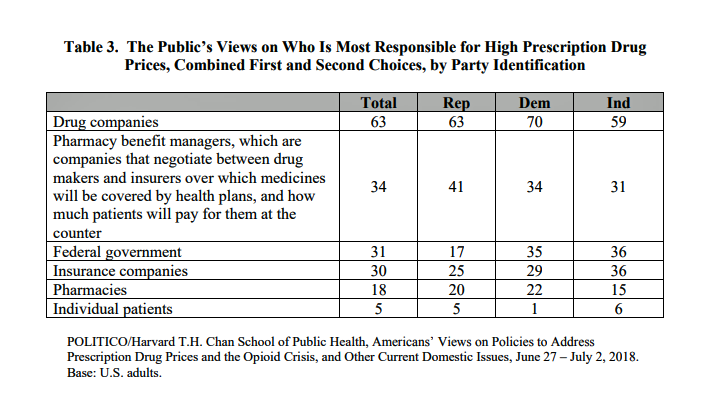
There’s growing evidence that a majority of U.S. voters, across the three-party landscape, agree on two healthcare issues this year: coverage of pre-existing conditions, and lowering the consumer-facing costs of prescription drugs. A new poll jointly conducted by Politico and the Harvard Chan School of Public Health bolsters my read on the latter issue – prescription drug pricing, which has become a mass popular culture union. There may be no other issue on voters’ collective minds for the 2018 mid-term election that so unites American voters than the demand for lower-cost medicines. This is directly relates to consumers’ tri-party
Value Comes to Healthcare: But Whose Value Is It?
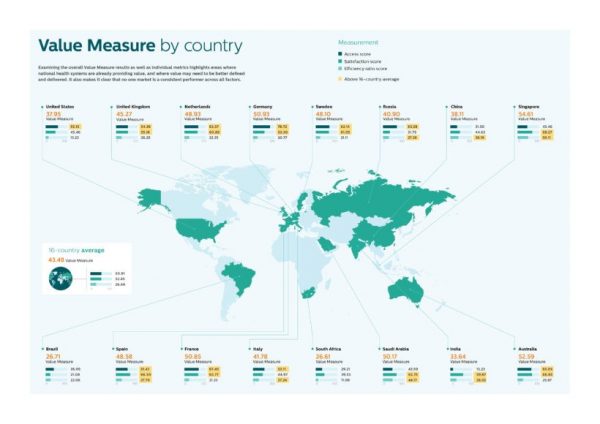
The Search for Value is the prevailing journey to a Holy Grail in healthcare these days. On that, most stakeholders working on the ground, globally. can agree. But whose value is it, anyway? Three reports published in the past few weeks give us some useful perspective on that question, woven together in today’s Health Populi blog. Let’s start with the Philips Future Health Index, which assesses value to 16 national health systems through three lenses: access, satisfaction, and efficiency. The results are shown in the map. “Value-based healthcare is contextual, geared towards providing the right care in the right place, at
Healthcare Policies We Can Agree On: Pre-Existing Conditions, Drug Prices, and PillPack – the June 2018 KFF Health Tracking Poll
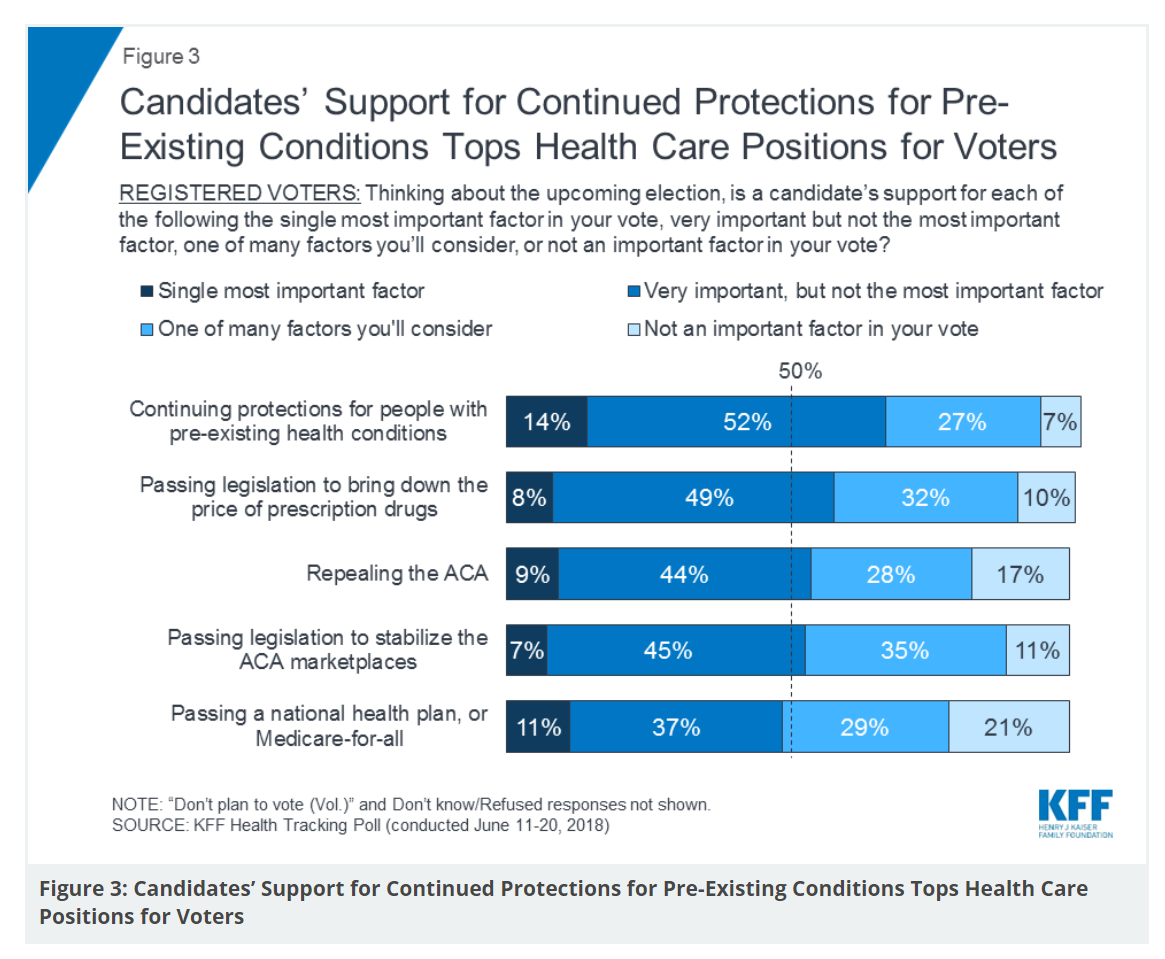
There are countless chasms in the U.S. this moment in social, political, and economic perspectives. but one issue is on the mind of most American voters where there is evidence of some agreements: health care, as evidenced in the June 2018 Health Tracking Poll from Kaiser Family Foundation. Top-line, health care is one of the most important issues that voters want addressed in the 2018 mid-term elections, tied with the economy. Immigration, gun policy, and foreign policy follow. While health care is most important to voters registered as Democrats, Republicans rank it very important. Among various specific health care factors, protecting
Hospitals Work to Address Customer Experience Gap With Consumers, Kaufman Hall Finds

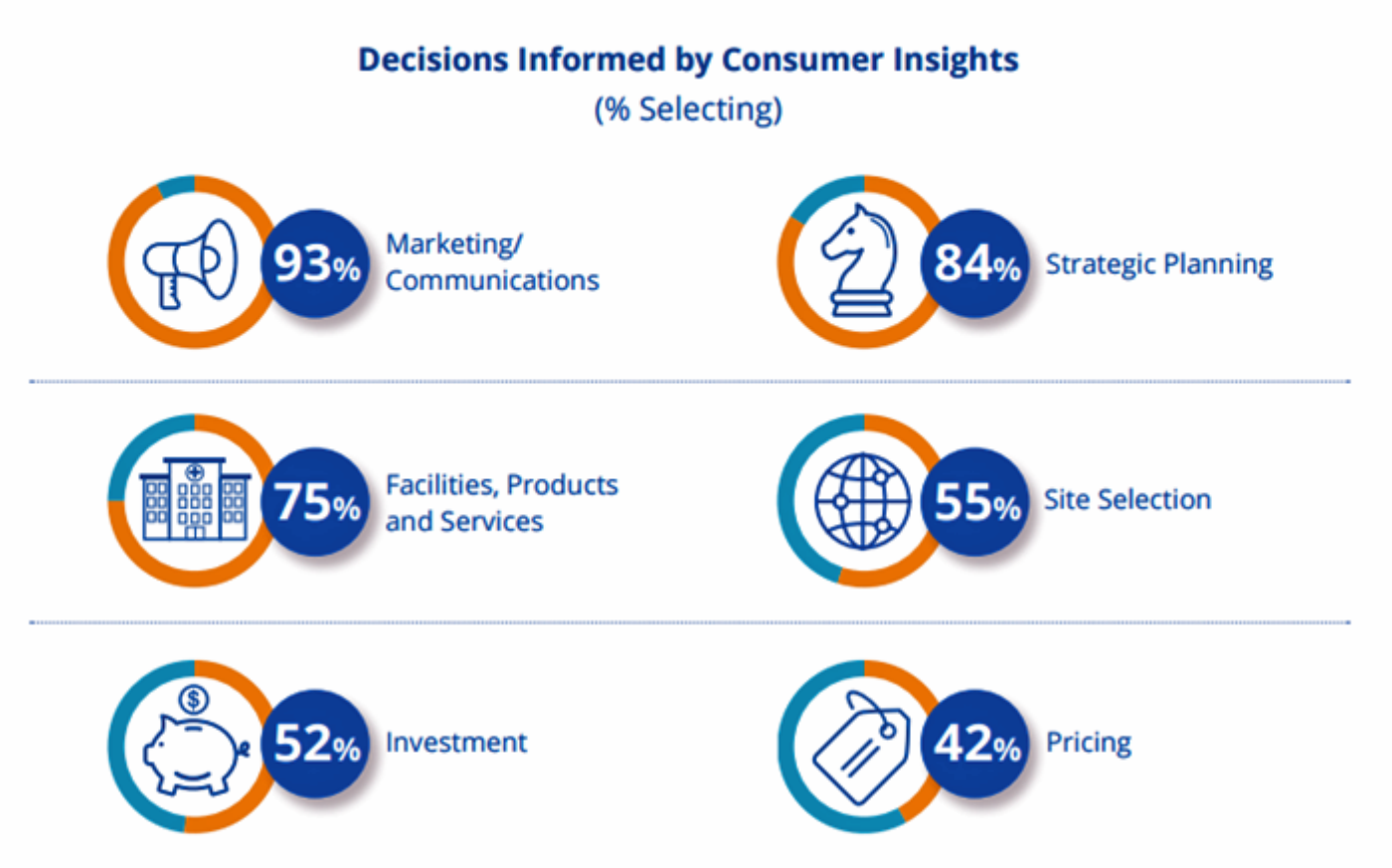
Hospital and healthcare providers are getting real about improving patient and health consumer experience, the latest Kaufman Hall research finds. The company’s 2018 State of Consumerism in Healthcare report is out, subtitled, “Activity in Search of Strategy.” Kaufman Hall has developed a Healthcare Consumerism Index for healthcare providers based on four pillars: access to care, consumer experience, pricing, and a strong foundation of consumer insights. Based on their assessment of providers on these components, Kaufman Hall found identified four tiers of performance: The top-performing group, Tier 1, includes only 8% of providers. These are the early adopters who allocate resources
Patients have ambitious health goals, and look to doctors for help

Consumers have health goals across many dimensions, topped with eating well, getting fit, reducing stress, sleeping better, feeling mentally well, and improving personal finances. That’s an ambitious health-and-wellness list, identified in the Health Ambitions Study, the first such research Aetna has published. Six in ten people are looking to food and nutrition for health, whether as “medicine” to deal with chronic conditions, for weight loss or general wellness, which is a frequent theme here on Health Populi. Consumers embrace their food habits as a key self-care determinant of health. Fitness, cited by most consumers, is also a can-do, self-powered activity
Doing Less Can Be Doing More for Healthcare – the Biggest Takeaway From ASCO 2018

Less can lead to more for so many things: eating smaller portions, lowering sugar consumption, and driving less in favor of walking or cycling come to mind. When it comes to healthcare utilization, doing less can also result in equal or even better outcomes. Groundbreaking research presented at this week’s ASCO meeting found that some women diagnosed with certain forms of cancer do not benefit from undergoing chemotherapy. The American Society of Clinical Oncology (ASCO) is one of the largest medical meetings annually, and at this huge meeting these research results for the TAILORx trial were huge news with big
Health Care for a Typical Working Family of Four in America Will Cost $28,166 in 2018
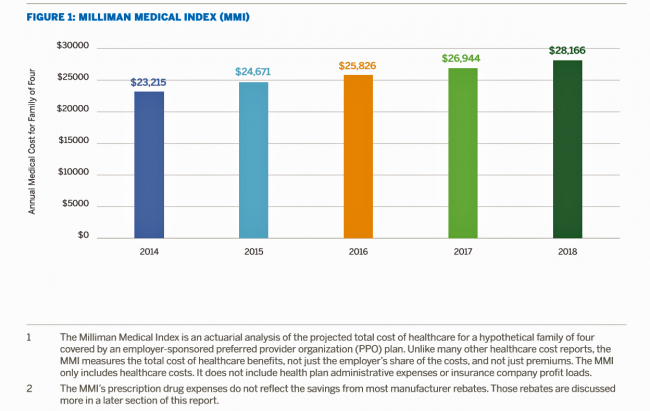
What could $28,166 buy you in 2018? A new car? A year of your child’s college education? A plot of land for your retirement home? Or a year of healthcare for a family of four? Welcome to this year’s edition of the Milliman Medical Index (MMI), one of the most important forecasts of the year in the world of the Health Populi blog and THINK-Health universe. That’s because we’re in the business of thinking about the future of health and health care through the health economics lens; the MMI is a key component of our ongoing environmental analysis of the
Having Health Insurance Is a Social Determinant of Health: the implications of growing uninsured in the U.S.
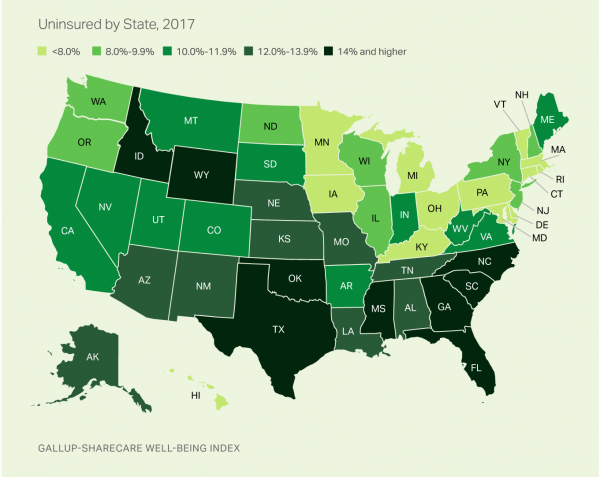
The rolls of the uninsured are growing in America, the latest Gallup-Sharecare Poll indicates. The U.S. uninsurance rate rose to 12.2% by the fourth quarter of 2017, up 1.3 percentage points from the year before. 2017 reversed advancements in health insurance coverage increases since the advent of the Affordable Care Act, and for the first time since 2014 no states’ uninsured rates fell. The 17 states with declines in insurance rates were Arizona, Colorado, Florida, Hawaii, Illinois, Indiana, Iowa, Missouri, New Mexico, New York, North Carolina, South Carolina, Texas, Utah, Washington, West Virginia, Wisconsin, and Wyoming. Among these, the greatest
Think Like a LEGO Builder in Healthcare – Considering PwC’s New Health Economy Vision
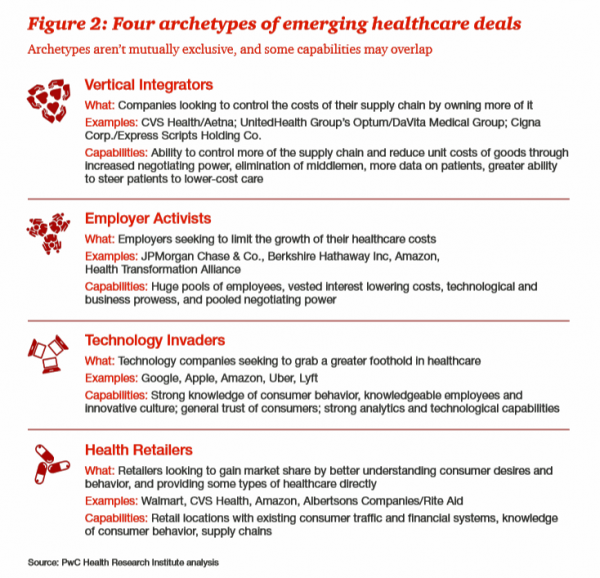
Expect “new combinations” of industry actors and technologies to reorganize and re-imagine healthcare, with an eye on both price and investments in customer experience (CX), PwC envisions in their latest report on The New Health Economy in the Age of Disruption. In this vision, healthcare will be a more flexible marketplace underpinned by data, platforms, and workers. Yes, it’s challenging to get from here-to-there, but PwC explains just how this can happen. Four archetypes, models, of healthcare deals have begun to emerge in the marketplace, illustrated by the Big Deals and announcements reshaping the industry in the past couple of years:
Americans’ Trust in the Healthcare System Low Compared to Rest-of-World’s Health Citizens
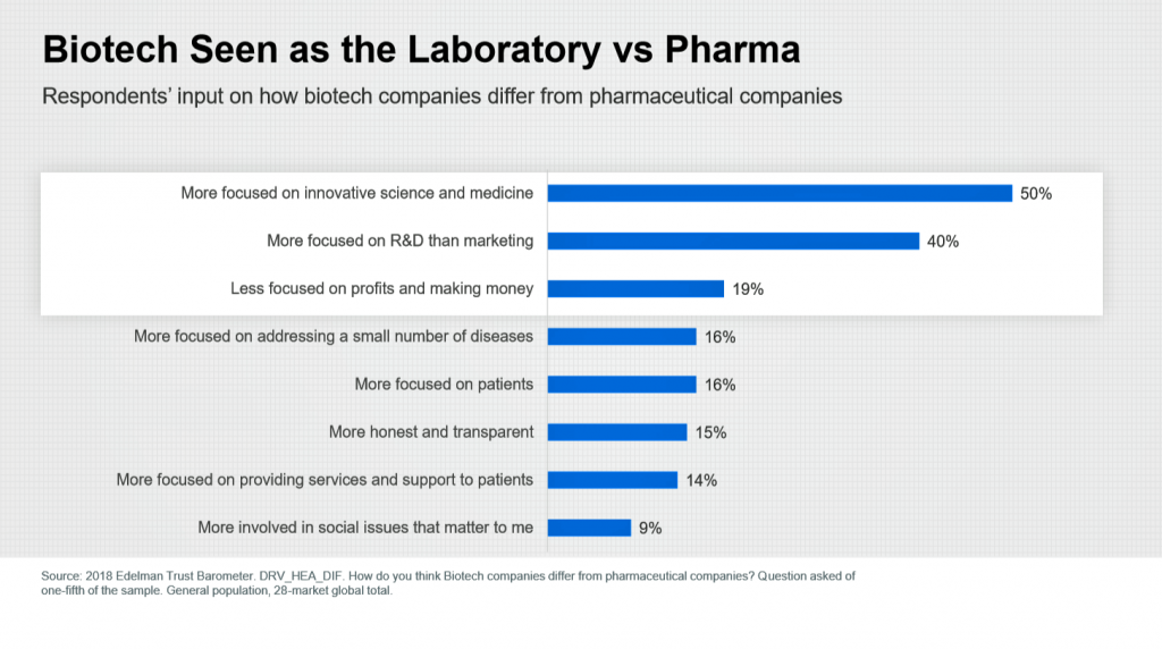
In the U.S., trust in the healthcare industry declined by 9 percentage points in just one year, declining from 62% of people trusting — that’s roughly two-thirds of Americans — down to 53% — closer to one-half of the population. I covered the launch of the 2018 Edelman Trust Barometer across all industries here in Health Populi in January 2018, when this year’s annual report was presented at the World Economic Forum in Davos as it is each year. The Edelman team shared this detailed data on the healthcare sector with me this week, for which I am grateful. Check
Food as Medicine Update: Danone Goes B-Corp, Once Upon a Farm Garners Garner, and Livongo Buys Retrofit

As the nation battles an obesity epidemic that adds $$ costs to U.S. national health spending, there are many opportunities to address this impactful social determinant of health to reduce health spending per person and to drive public and individual health. In this post, I examine a few very current events in the food-as-medicine marketspace. Big Food as an industry gets a bad rap, as Big Tobacco and Big Oil have had. In the case of Big Food, the public health critique points to processed foods, those of high sugar content (especially when cleverly marketed to children), and sustainability. But
Livongo and Cambia Allying to Address Chronic Disease Burden and Scale Solutions to Consumers

Chronic diseases are what kill most people in the world. In the U.S., the chronic disease burden takes a massive toll on both public health and mortality, accounting for 7 in 10 deaths in America each year. That personal health toll comes at a high price and proportion of national health expenditures. A new alliance between Livongo and Cambia Health seeks to address that challenge, beginning with diabetes and scaling to other chronic conditions. Livongo has proven out the Livongo for Diabetes program, which has demonstrated positive outcomes in terms of patient satisfaction and cost-savings. The plan with Cambia is
The Patient As Payor: From Rationing Visits Due to Co-Pays to Facing $370K for Healthcare in Retirement
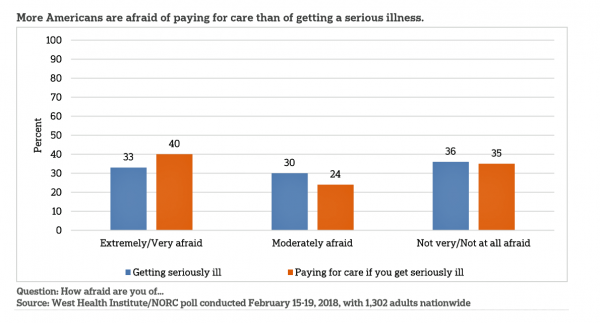
Health care in America is such a scary experience that more people are afraid of paying for care than the actually getting sick part of the scenario. The patient is the payor, and she is afraid…more afraid of the paying than of the illness, according to a survey conducted among U.S. health consumers from WestHealth Institute and NORC, Americans’ Views of Healthcare Costs, Coverage, and Policy from WestHealth and NORC. See the orange bar on the left: 40% of Americans are “extremely or very afraid” about paying for care if they get seriously ill, and 33% are that afraid
Rx 2018: A New Era of Specialty Drugs, Telehealth, Mobile Apps and Value, IQVIA Reports
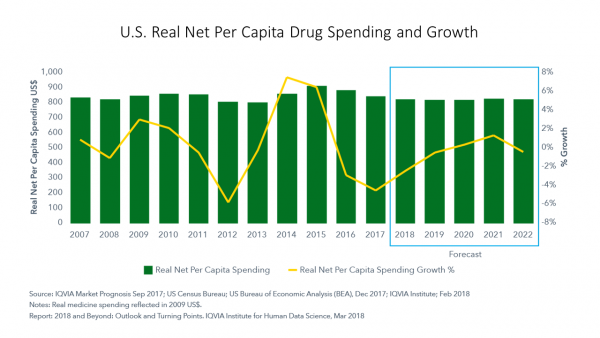
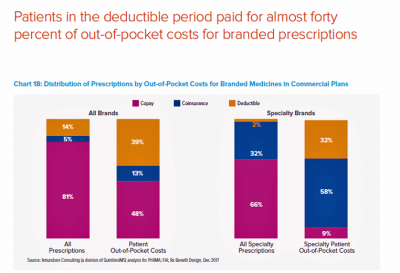
In 2018, spending on branded prescription drugs will fall in wealthy countries, while spending on specialty drugs will increase, resulting in flat medicines spending. In the U.S., net spending on medicines will fall in 2018 and remain flat at about $800 per person, according to forecasts in 2018 and Beyond: Outlook and Turning Points, from the IQVIA Institute for Human Data Science. “Concerns about existing medicine costs have captured significant attention,” the introduction warns, setting the stage for slowing growth. Key factors for slow growth include payor concerns about budgets and the consideration of value when deciding on access for new
Building Trust and Truth in Patient Social Networks
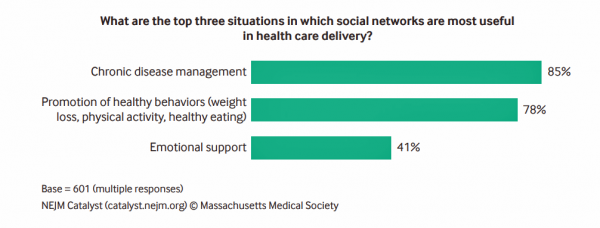
We are only just past the dawn of the second machine age, where digitization is enabling artificial intelligence. “Our new tools are destroying both trust and truth, creating a hunger for community and authenticity. We crave actual physical connection to neighbours, colleagues, and fellow townspeople, even if digitally facilitated.” Anne-Marie Slaughter wrote this in a column I read this morning in the Financial Times titled, “Our struggle with technology to protect trust and truth.” Trust and truth underpin health engagement, we learned in the first Edelman Health Engagement Barometer launched ten years ago. Those were the early days of the formation
More Working Americans Enrolled in High-Deductible Health Plans in 2017
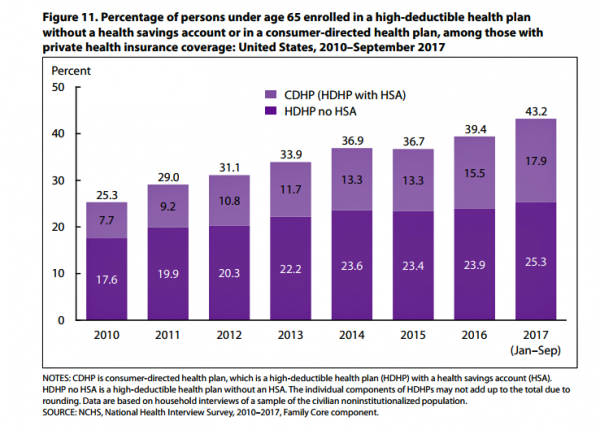
Over four in 10 U.S. workers were enrolled in a high-deductible health plan in the first 9 months of 2017, according to the latest research published by the National Center for Health Statistics, part of the Centers for Disease Control in the U.S. Department of Health and Human Services. The report details Health Insurance Coverage: Early Release of Estimates From the National Health Interview Survey, January-September 2017. About 28 million people were uninsured in the U.S. in 2017, about the same proportion as in 2016 — but nearly 20 million fewer than in 2010, as the line chart illustrates. The
Consumer Health and Patient Engagement – Are We There Yet?

Along with artificial intelligence, patient engagement feels like the new black in health care right now. Perhaps that’s because we’re just two weeks out from the annual HIMSS Conference which will convene thousands of health IT wonks, users and developers (I am the former), but I’ve received several reports this week speaking to health engagement and technology that are worth some trend-weaving. As my colleague-friends Gregg Masters of Health Innovation Media (@2healthguru) and John Moore of Chilmark Research (@john_chilmark) challenged me on Twitter earlier this week: are we scaling sustained, real patient engagement and empowerment yet? Let’s dive into the
The $4 Trillion Health Economy of 2020
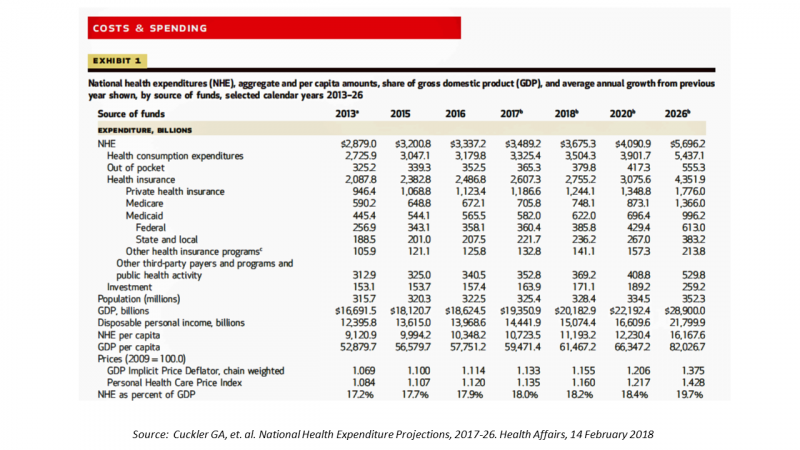
In 2020, national health expenditures (NHE) in the United States will exceed $4 trillion to cover 334.5 million Americans. That equates to 18.4% of the Gross Domestic Product (GDP) and $12,230.40 of health spending per person. I sat in on a press call today with researchers from the Office of the Actuary working in the Centers for Medicare and Medicaid Services (CMS) to review the annual forecast of the NHE, published in Health Affairs in a statistically-dense eleven page article titled, National Health Expenditure Projections, 2017-2026: Despite Uncertainty, Fundamentals Primarily Drive Spending Growth. What are those “fundamentals” pushing up healthcare spending?
When Buying a Pair of Jeans Competes With Filling a Prescription at CVS in Target

Stories about three fashion brands have me thinking about women and their health economics. Stay with me. Target unveiled its new line of clothing, Universal Thread, which features pieces that are accessible to women who may be dealing with physical limitations or sensory challenges. I first read about Universal Thread on The Mighty website, which is a community of over 1 million people interested in connecting on health and disabilities. As The Mighty described, the brand Universal Thread, “is centered around denim since it is a staple in many women’s wardrobes, but denim can be uncomfortable for many people with disabilities
U.S. Workers Say Health Care is the Most Critical Issue Facing the Nation
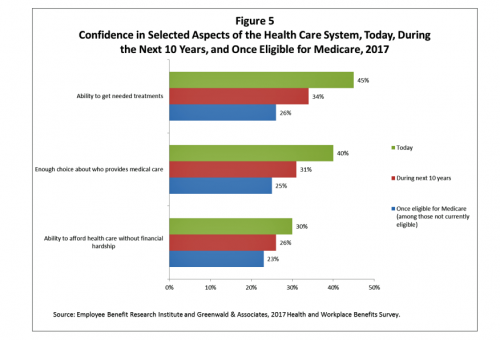
Health care ranks highest among working Americans as the top critical issue facing the country, well above terrorism, the role of the Federal government, unemployment and jobs, education, immigration and taxes. Over half of American workers also rate the country’s healthcare system as “poor” or “fair,” based on the results of the EBRI/Greenwald & Associates Health and Workplace Benefits Survey. Workers dissatisfaction with U.S. healthcare is based largely on cost: one-half of workers experienced an increase in health care costs in the past year. Furthermore, only 22% are satisfied with the cost of their health insurance plan, 18% are satisfied
Health Insurance Costs Stress US Whether We’re Rich or Not / and Why a $0 Budget for CFPB Matters for Healthcare

Health care costs cause anxiety for U.S. adults, regardless of their affluence, we learn in Uncertainty About Healthcare, the latest Stress in America poll from the American Psychological Association. The big stat is that 2 in 3 Americans say the cost of health insurance is a stressor for them or their loved ones, whether the person earns more or less than $50,000 a year. Underneath that top-line are some demographic differences. Millennials are most concerned about access to mental health care compared with Boomers and older adults. Reproductive care access is of most interest to Millennials and Gen Xers. Two-thirds
Healthy Living in Digital Times at CES 2018

Connecting Life’s Dots, the organization Living in Digital Times partners with CES to deliver conference content during the show. At CES 2018, LIDT is connecting a lot of dots to help make health streamline into daily living. Robin Raskin, founder, kicked off LIDT’s press conference setting the context for how technology is changing lifestyles. Her Holy Grail is to help make tech fun for everybody, inclusive for everybody, and loved by everybody, she enthused. LIDT has been a presence at CES for many years, conceiving the contest the Last Gadget Standing, hosting tech-fashion shows with robots, and supporting a young innovators
The Cloud’s Growing Role in Consumer-Pharma Health Engagement

The pharmaceutical industry is facing a multitude of political, regulatory, and financial uncertainties in and beyond 2018. But there’s one thing I know for sure about pharma’s morphing business model: it’s that patients are playing a growing role in the industry’s future well-being. That is, if the industry can meet health consumers where they want to be met. Patients want more communication and support from pharma companies, a new study from Accenture found. In fact, over one-third of patients tell their health care providers about pharma patient-service programs: this chart from Accenture’s study illustrates the top seven ways providers hear
Nurses Rate Highest for Ethics in American Professions Once Again in Gallup Poll
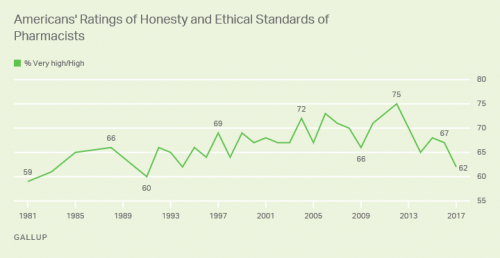
Nurses working in the U.S. are number one when it comes to ethics and honesty, the Gallup Poll found for the sixteenth year in a row. After nurses, military officers, grade school teachers, medical doctors and pharmacists rank second through fifth in ethical-line behind top-rated nursing. It’s important to note that consumers have ranked pharmacists and doctors in second and third place in this annual survey for many years. This year, both professions fall below the military and teachers. Nurses have been #1 in this study every year since Gallup launched the survey in 1999, except for 2001 when firefighters topped
CVS + Aetna: An Inflection Point for American Healthcare

The nation’s largest retail pharmacy chain signed a deal to combine with one of the top three health insurance companies. The deal is valued at $69 billion. I wrote about this inflection point for U.S. healthcare four weeks ago here in Health Populi. CVS is both the biggest pharmacy and pharmacy benefit manager in the U.S., as the first chart shows. In my previous post, I talked about the value of vertical integration bringing together the building blocks of retail pharmacy and pharmacist care, retail clinics, the PBM (Caremark), along with Aetna’s health plan member base and business. As Amazon and other
Movin’ Out(patient) – The Future of the Hospital is Virtual at UPMC

In 2016, most consultations between patients and Kaiser-Permanente Health Plan were virtual — that is, between consumers and clinicians who were not in the same room when the exam or conversation took place. Virtual healthcare may be the new black for healthcare providers. Mercy Health System in St. Louis launched a virtual hospital in 2016, covered here in the Health Populi post, “Love, Mercy, and Virtual Healthcare.” Intermountain Healthcare announced plans to build a virtual hospital in 2018. And, earlier this month, UPMC’s CEO, Jeffrey Romoff, made healthcare headlines saying, “UPMC desires to be the Amazon of healthcare.” UPMC, aka University of Pittsburgh
Health Care Is 2.5 More Expensive Than Food for the Average U.S. Family
The math is straightforward. Assume “A” equals $59.039, the median household income in 2016. Assume “B” is $18,142, the mean employer-sponsored family insurance premium last year. B divided by A equals 30.7%, which is the percent of the average U.S. family’s income represented by the premium cost of health insurance. Compare that to what American households spent on food: just over $7,000, including groceries and eating out (which is garnering a larger share of U.S. eating opportunities, a topic for another post). Thus, health care represents, via the home’s health insurance premium, represents 2.5 times more than food for the
A Health Consumer Perspective on CVS+Aetna
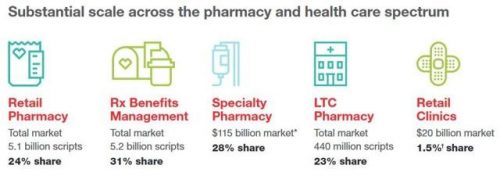
A response to Amazon’s potential moves in healthcare and pharmacy…strategic positioning for the post-Trump healthcare landscape…vertical integration to better manage healthcare utilization and costs…these, and other rationale have been offered by industry analysts and observers of the discussions between CVS and Aetna, for the former to acquire the latter. “A pharmacy chain buying a health insurance company?” many have asked me over the past few days. These inquiring minds include people who work both inside and outside of health/care. I ask back: in 2017 and in the future, “What is a pharmacy? What is a health plan?” See the
CVS Health in Talks to Acquire Aetna – The Changing Retail Health Landscape

Just a few days since CVS Health announced the company would be working with mega-health insurer Anthem on a prescription drug management program, the pharmacy chain today is reportedly in talks to buy Aetna, the national health insurance company, according to CNBC and other credible news outlets like the Wall Street Journal. Remember that Aetna’s bid to acquire Humana was scuttled earlier this year after many months of negotiation and positioning, along with FTC scrutiny about antitrust. That insurance merger “died” on one day in February 2017 along with an Anthem-CIGNA deal, covered here by CNN. A deal between CVS
Health (Healthcare, Not So Much) Abounds in Prophet’s Top 50 Brands

U.S. consumers’ most-valued brands include Apple, Google, Amazon, Netflix, Pinterest, Android, Spotify, PIXAR, Disney and Samsung, according to the 2017 Brand Relevance Index from Prophet. The top 50 are shown in the first chart. On the second chart, I’ve circled in red the brands that have reach into healthcare, health, fitness, and wellness. Arguably, I could have circled every brand in the top 50 because in one way or another, depending on the individual, people find health “everywhere” that’s relevant to them based on their own definitions and value-systems. This is Prophet’s third year conducting this study, and I was
Four Things We Want in 2017: Financial Health, Relationships, Good Food, and Sleep

THINK: money and love. To find health, working-aged people seek financial stability and good relationships, according to the Consumer Health POV Report from Welltok, meQuilibrium, and Zipongo, featured in their webinar broadcast today. The online consumer survey was conducted among 2,000 full-time working U.S. adults in August 2017, segmented roughly into thirds by Boomers (37%), Gen Xers (32%), and Millennials (31%). Much lower down the priority list for healthy living are managing food, sleep, and stress based on the poll. Feeling stress is universal across most consumers in each of the three generational cohorts, especially related to work and finance.
President Trump Utters “M” for Murder, and a $1 MM Price Tag for Rx Therapy – an October 2017 Pharma Update
Last week, President Trump once again used the “M” word (“murder”) in a sentence accusing the pharmaceutical industry of too-high priced products for U.S. health citizens. The sentence included the phrase, “Drug companies are getting away with murder.” That week, USA Today published an article on a new FDA-approved specialty drug therapy that could add up to over a $1 mm price tag. There is much to report in the world of pharmaceutical innovation, pricing, and patient Rx coverage this month. The CVS Health – Epic announcement ranks high in Health Populi’s vision for the evolving health/care ecosystem, bringing together two
What Health Plans Must Learn from Amazon
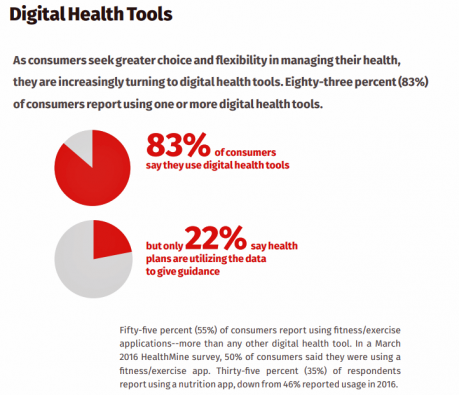
One in two U.S. consumers told Aflac that enrolling in health insurance should feel like an experience on Amazon. But health consumers still lack that high benchmark retail experience with health plans, based on new research published in HealthMine’s 2017 Health Intelligence Report focusing on communication and digital healthcare tools. “Most members believe health plan communications are impersonal and centered around bills rather than healthcare guidance,” HealthMine asserts in the introduction to the report. That’s about as un-Amazon as we can imagine. Top findings from HealthMine’s research are that: 3 in 4 consumers don’t think their health insurance plan
The Mainstreaming of Wellness

“Wellness is a way to cope with the demands and rigors of new modern lifestyles,” according to Ogilvy in their latest report, The Wellness Movement Pioneers: New Global Research Findings. The report makes the case that the mass public are project-managing life adopting mental health, nutrition, physical activity and sleep to boost personal wellness. There is a big business model underneath this, which has inspired Ogilvy to start up the company’s Health & Wellness Practice. Think of this report as the group’s own business case to address the $3.7 trillion global wellness economy, illustrated by the first image. The report
Patients Are Looking to Finance Healthcare Over Time
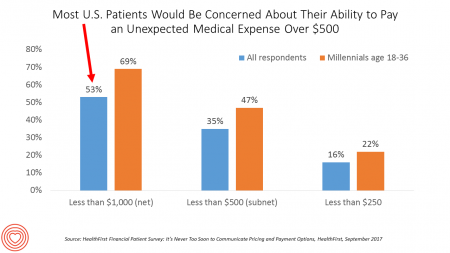
Most U.S. patients want healthcare providers to offer cost information before a procedure, and whether doctors offer financial options to help them extend payments over time. This is an automotive or home appliance procedure we’re talking about. It’s healthcare services, and American patients are now the third largest payors to providers in the nation. Thus, the title of a new report summarizing a consumer survey from HealthFirst notes, “It’s Never Too Soon to Communicate Pricing and Payment Options. The study found that two-thirds of U.S. consumers would like healthcare providers to discuss financing options; however, only 18 percent of providers have
Health Equity Lessons from July 23, 1967, Detroit
On July 23, 1967, I was a little girl wearing a pretty dress, attending my cousin’s wedding at a swanky hotel in mid-town Detroit. Driving home with my parents and sisters after the wedding, the radio news channel warned us of the blazing fires that were burning in a part of the city not far from where we were on a highway leading out to the suburbs. Fifty years and five days later, I am addressing the subject of health equity at a speech over breakfast at the American Hospital Association 25th Annual Health Leadership Summit today. In my talk,
Note to Mooch: The ER is Not Universal Health Care
I quote directly from the Twitter feed of Anthony Scaramucci, @scaramucci: “@dhank2525 agree. We already have Univ Health Care, we made decision long ago to treat everyone that enters an emergency room.” Mr. Scaramucci is President Trump’s Communications Chief, replacing Sean Spicer. Mr. Scaramucci is neither veteran journalist nor healthcare policy wonk. He’s a successful businessman, which I respect for his savvy and ability to build a fund, attract investors, and create a media persona which he has telegenically broadcast on CNBC and elsewhere over the past decade. He’s got a engaging public personality, and goes by the moniker, “Mooch.” But
Strengthening Chronic Care Is Both Personal and Financial for the Patient
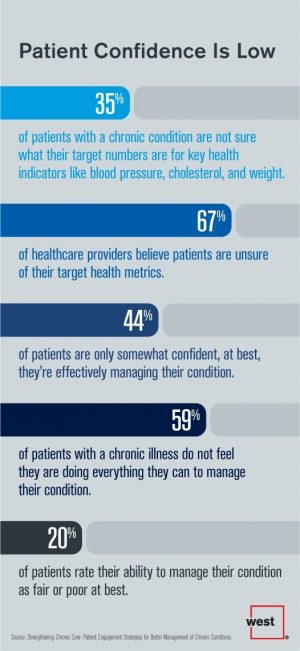
6 in 10 people diagnosed with a chronic condition do not feel they’re doing everything they can to manage their condition. At the same time, 67% of healthcare providers believe patients aren’t certain about their target health metrics. Three-quarters of physicians are only somewhat confident their patients are truly informed about their present state of health. Most people and their doctors are on the same page recognizing that patients lack confidence in managing their condition, but how to remedy this recognized challenge? The survey and report, Strengthening Chronic Care, offers some practical advice. This research was conducted by West
Global Drug Sales Forecasts Fall For Next Five Years
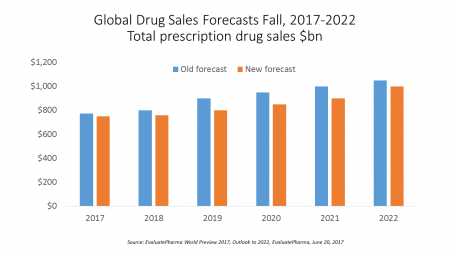
Total prescription drug sales have been trimmed, based on calculations of EvaluatePharma which forecasts a $390 bn drop in revenues between 2017 and 2022. “Political and public scrutiny over pricing of both new and old drugs is not going to go away,” EvaluatePharma called out in its report. The intense scrutiny on pharma industry pricing was fostered by Martin Shkreli in his pricing of Daraprim (taking a $13.50 product raising the price to $750), Harvoni and Sovaldi pricing for Hepatitis C therapies, and last year’s EpiPen pricing uproar. A May 2017 analysis of prescription drug costs by AARP judges that, “Nothing
Consumer Experience Is An Integral Part of the Healthcare Experience
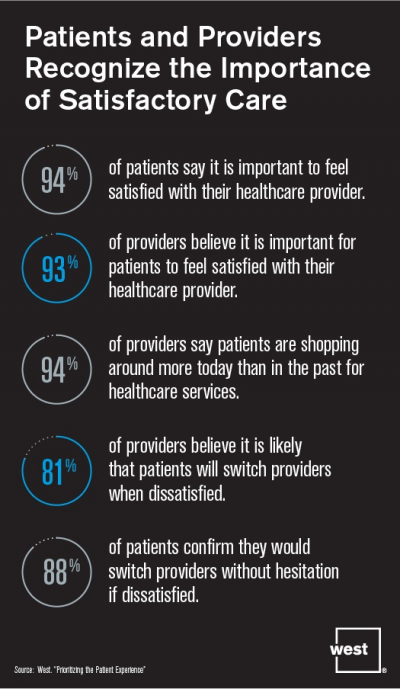
Patient satisfaction should be baked into healthcare provider service goals, according to Prioritizing the Patient Experience from West Corporation, the communications company. West is in the business of improving communications systems, and has a vested interest in expanding comms in health. This research polled patients and providers to assess how each healthcare stakeholder perceives various patient satisfaction issues, which when done well are grounded in sound communications strategy and technologies. Patient satisfaction is directly linked to the bottom lines of healthcare organizations, West contends, due to two key drivers: Evolving payment models are increasingly tying patient satisfaction to reimbursements; and,
Helping People On A Path to Better Health with CVS @Retail

“Helping people on their path to better health” is the mission-mantra of CVS Health. Re-branded from its previous identity as CVS/pharmacy, the organization convened a Health Innovation Summit with its vendor partners whose products fill the front-of-store shelves to empower, inspire and support consumers to manage health and wellness for themselves and their families. I was grateful for the opportunity to provide the first talk for the day, setting the context for the evolving retail health/care landscape with the consumer at the center. The consumer is, at any point in a 24-hour day: a person wearing many hats (a worker,
U.S. Consumers Expect, But Don’t See, Innovation From the Health & Wellness Industry
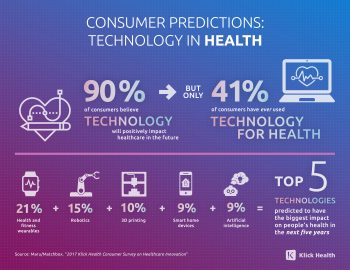
U.S. consumers consider Consumer Electronics to be the most innovative industry they know. But people believe that Health & Wellness should be the most innovative sector in the economy. Welcome to the 2017 Klick Health Consumer Survey, which focuses on health innovation in the context of peoples’ hopes for technology to improve health and healthcare. 1 in 2 people say that technology has had a positive impact on their health and wellness, skewing slightly more toward younger people (although 45% of people 55 years of age and older agree that tech positively contributes to health. 41% of consumers say they’ve
From Hospitality to Health-pitality to Sportspitality

“Stay well, even on the road,” welcomes the chain of EVEN Hotels. That message from a hospitality company is part of the growth of the retail health landscape, driven by consumers’ desire to live well and make healthy decisions every day – even during business trips. The message is that, “Wellness is more than a word. It’s your way of life. But when it’s time to travel, it all falls apart,” Who among us road warriors for work doesn’t get that message? This is a real trend that engaged health consumers have begun to demand. A friend of mine traveled this week
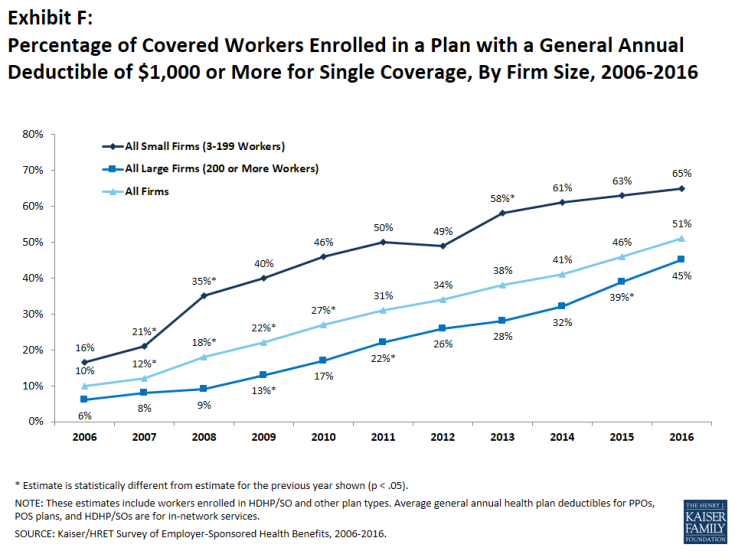
As High Deductible Health Plans Grow, So Does Health Consumers’ Cost-Consciousness
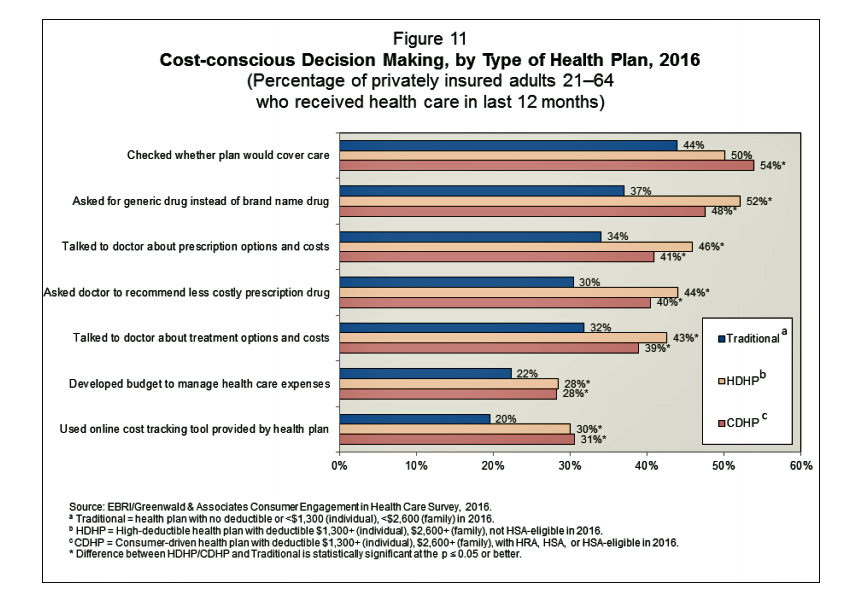
A person enrolled in a high-deductible health insurance plan is more likely to be cost-conscious than someone with traditional health insurance. Cost-consciousness behaviors including checking whether a plan covers care, asking for generic drugs versus a brand name pharmaceutical, and using online cost-tracking tools provided by health plans, according to the report, Consumer Engagement in Health Care: Findings from the 2016 EBRI/Greenwald & Associates Consumer Engagement in Health Care Survey from EBRI, the Employee Benefit Research Institute. A high deductible is correlated with more engaged health plan members, EBRI believes based on the data. One example: more than one-half of people enrolled
How To Pay For A Serious Medical Illness Tops Americans’ Fiscal Fears
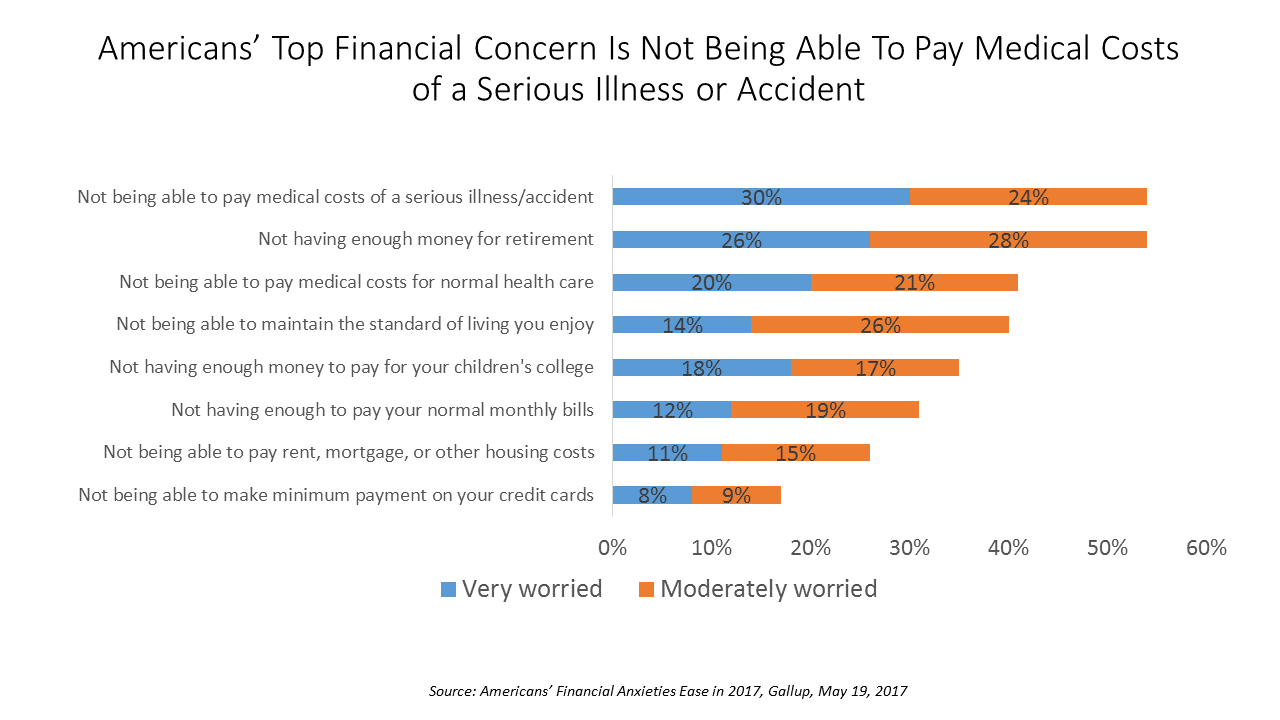
While Americans’ financial worries are softening in 2017, one issue tops the list of fiscal fears: not having enough money to pay the costs involved in a serious illness or accident, Gallup found in a consumer poll fielded in early April 2017. 54% of Americans fear an inability to cover healthcare costs in the event of an accident or serious illness. This percentage was 60% in 2016, and 55% in 2015. This year’s data point ties with Americans financial worry about not having enough money for retirement, but healthcare cost concerns rank higher in terms of being “very worried” versus
Expecting Alexa and Roomba for Health: Emerging AI and Robotics Trends for Healthcare via PwC
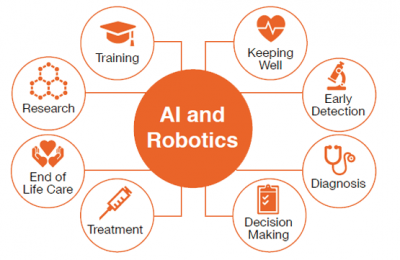
“What doctor?” asks the title of a PwC report on the emergence of artificial intelligence (AI) and robotics in healthcare. AI and robot technology are penetrating all aspects of the macroeconomy, and they’ve begun to re-shape the health economy, as well. Underneath PwC’s titular question are two lenses: the role of the AI/robot doctor vis-a-vis the role of the human doctor. PwC identifies eight areas that AI and robotics will impact in healthcare, shown in the first diagram: Decision making Diagnosis Early detection End of life care Keeping well Research Training, and Treatment. For keeping well, AI and robotics can
Shopping Food for Health is Mainstream, But Nutrition Confusion is Super-Sized
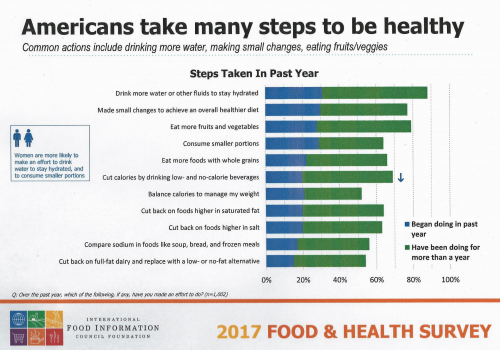
Americans are overwhelmingly keen to use food for their health, and overwhelmed by the amount of nutrition information they face to make good shopping and eating decisions. Welcome to “food confusion,” a phenomenon gleaned from the 12th Annual Food and Health Survey conducted by the International Food Information Council Foundation (IFIC). This 12th annual survey from IFIC finds that most Americans take many steps to be healthy. In the past year, the most popular health-steps include drinking more for hydration, making small changes to achieve a healthier diet, consuming smaller portions, eating more fruits and vegetables, and eating more whole grains.
Home Is the New and Future Medical Home for Dialysis

The economics of kidney disease in America is a hefty burden: about 26 million people in the U.S. have some aspect of chronic kidney disease and are at-risk of kidney failure. The number of people diagnosed with kidney disease doubled during each of the last two decades, according to the American Society of Nephrology. The annual cost of treating end-stage renal disease (ESRD) is over $32 billion, consuming 28% of Medicare expenditures…and increasing. Now consider the personal costs of dialysis in America: about $500 for a single hemodialysis treatment in a center, roughly $72,000 a year for one patient. There
Medicines in America: The Half-Trillion Dollar Line Item
Prescription drug spending in the U.S. grew nearly 6% in 2016, reaching $450 billion, according to the QuintilesIMS Institute report, Medicines Use and Spending in the U.S., published today. U.S. drug spending is forecasted to grow by 30% over the next 5 years to 2021, amounting to $610 billion. In 2016, per capita (per person) spending on medicines for U.S. health citizens averaged $895. Specialty drugs made up $384 of that total, equal to 43% of personal drug spending, shown in the first chart. Spending on specialty drugs continues to increase as a proportion of total drug spending: traditional medicines’ share
Financial Stress As A Health Risk Factor Impacts More Americans
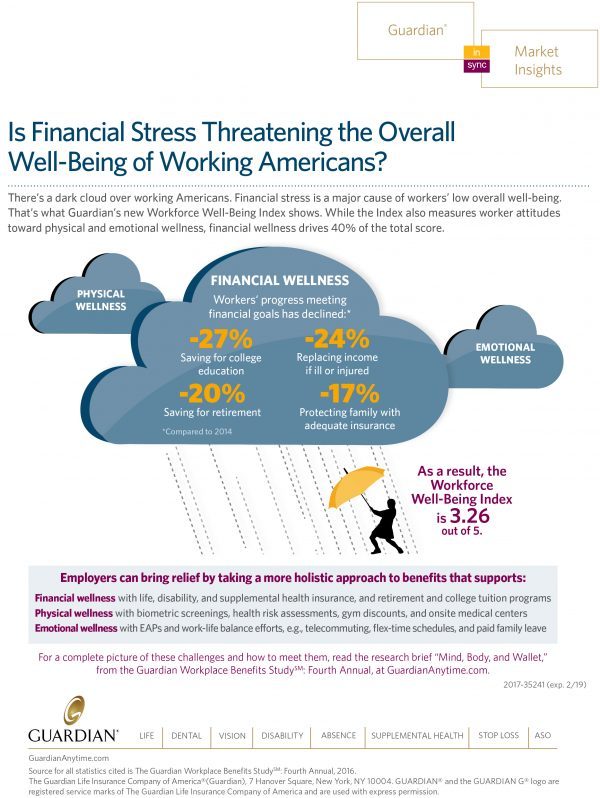
A family in Orange County, California, paid a brother’s 1982 hospital bill by selling 50 pieces of their newly-deceased mother’s jewelry. “It’s what she wanted,” the surviving son told a reporter from The Orange County Register. The cache of jewelry fetched enough to pay the $10,000 bill. Patients in the U.S. cobble together various strategies to pay for healthcare, as the first chart drawn from a Kaiser Family Foundation report on medical debt attests. As health care consumers, people cut back on household spending like vacations and household goods. Two-thirds of insured patients use up all or most of their savings
Telehealth and Virtual Healthcare Are Mainstreaming
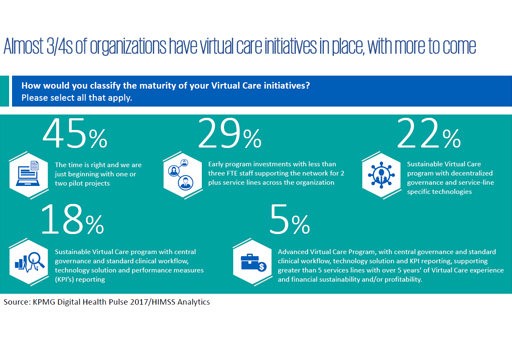
As the annual meeting of the American Telemedicine Association convenes this week in Orlando, there’s a lot of telehealth news to curate. The topline of it all: virtual healthcare is mainstreaming, with more providers, payors, and patients aligning in support of virtual health care delivery. Three-quarters of providers have some form of basic telemedicine or telehealth in place. One-third of healthcare providers use some flavor of virtual care technology in their workflow, according to research from KPMG and HIMSS Analytics summarized in the first graphic. KPMG sees virtual care options — remote patient monitoring, enhanced portals, and web interactions for patient-provider
Finding Health in Consumer Goods

People want to live healthier lives, and consumer good companies are responding to these demands to keep and gain market share and profit margins. Consumer product firms reformulated over 180,000 consumer products in 2016 for in response to consumers’ health and wellness wishes, based on data collected by Deloitte for The Consumer Goods Forum project (CGF) and published in The CGF Health & Wellness Progress Report. The CGF is an industry network of some 400 consumer goods, retail, and service companies supporting the global adoption of standards and practices. This Report focused on the CGF members’ progress toward health and wellness
Health Insurance Plans Rank Lowest In Consumer Experience
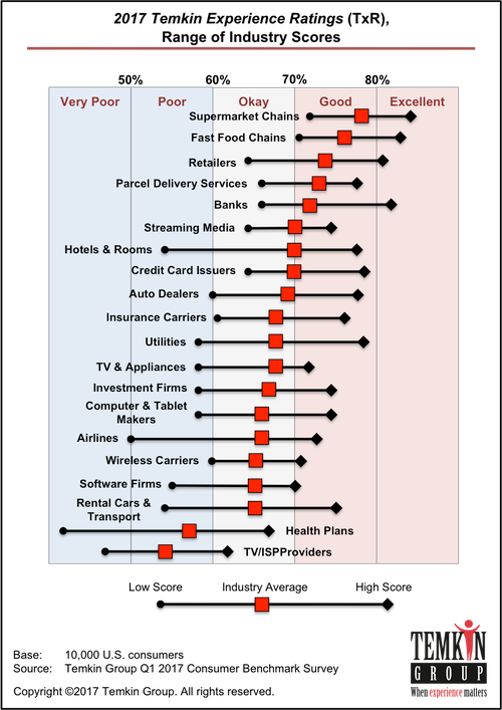
Consumers love their supermarkets, fast food shops, retailers, delivery services, and banks. These industries rank highest in the 2017 Temkin Experience Ratings, my go-to source for understanding consumer service Nirvana. Health insurance companies and internet service providers (ISPs) are at the bottom of the Temkin Ratings, as shown in the first chart. Note that health plans range from a score approaching 70 to under 50, illustrating the very wide range of consumer experience from okay-to-good, too very poor. The top-ranked health plan was Kaiser Permanente, with a rating of 67%; Health Net was ranked the worst of the health plans
Pharma Industry Reputation Declines Second Year In A Row
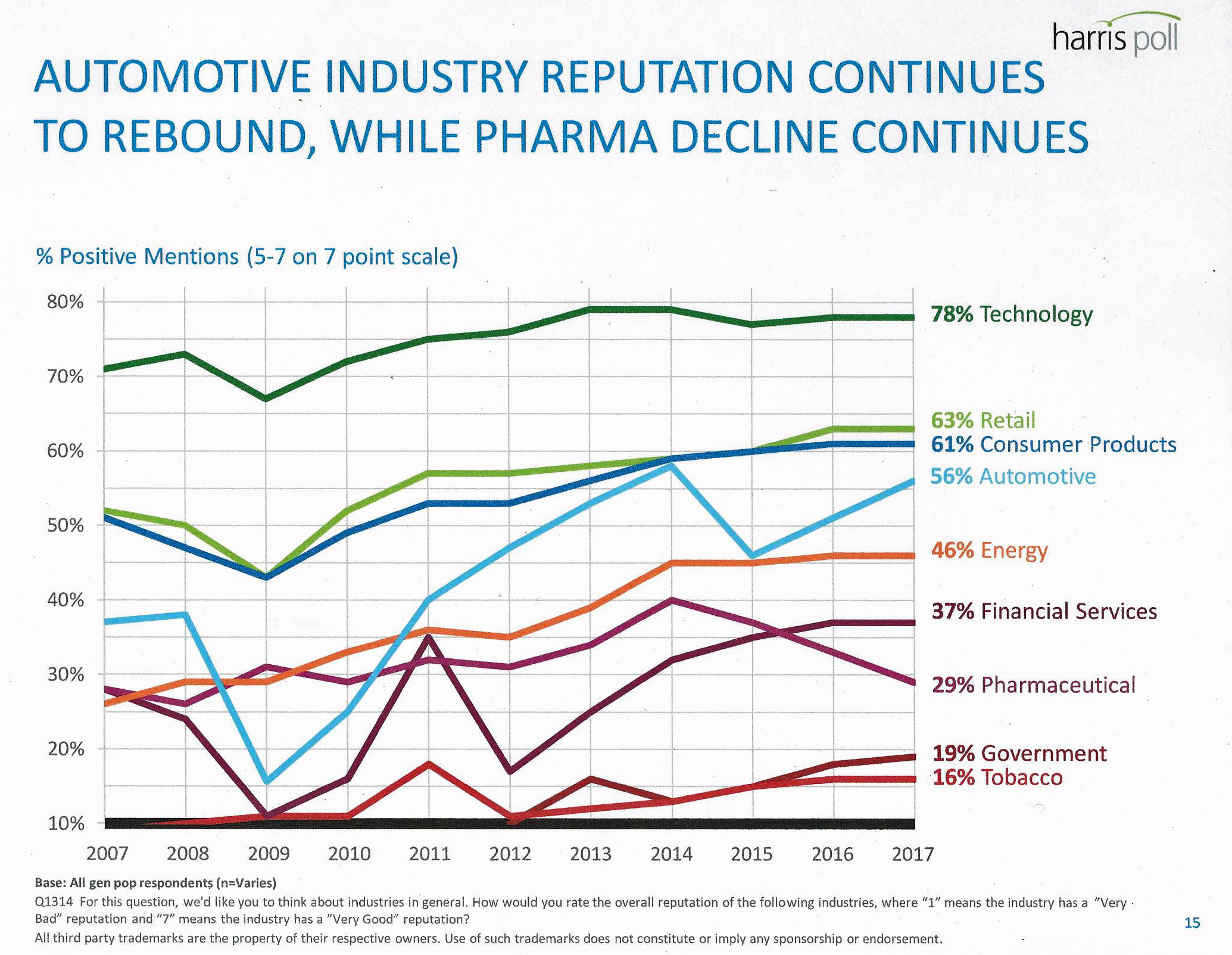
U.S. consumers love technology, retail, and consumer products; automotive company reputations are improving, even with Volkswagen’s emission scandal potentially tarnishing the industry segment. The only corporate sector whose reputation fell in 2016 was the pharmaceutical industry’s, according to the Harris Poll’s 2017 Reputation Quotient report. The line chart illustrates the decline of pharma’s reputation, which puts it on par with its consumer perceptions in 2010 — just before Medicare Part D was legislated and implemented, which improved pharma’s image among American health citizens (especially older patients who tend to be more frequent consumers of prescription drugs). Pharma’s reputation quotient is back
The Fall of the TrumpCare is Retail Health’s Gain in 2017

The non-vote for and withdrawal of The American Health Care Act on March 24, 2017, was a win for the retail health market, at least in the short-run. Before the vote, there had been some pronouncements that the passage of the AHCA would have been a boon to retail health. Here’s one story stating that, “A boom in medical tourism to Mexico predicted if Obamacare ends.” Another article asserts, “Why the American Health Care Act Works for Retailers,” a public policy statement from the National Retail Federation (NRF). But NRF, please don’t fret. Retail health is consumer-driven and will persist beyond the
Medical Bill Toxicity: 53% of Americans Say A Big Bill Is As Bad As A Serious Diagnosis
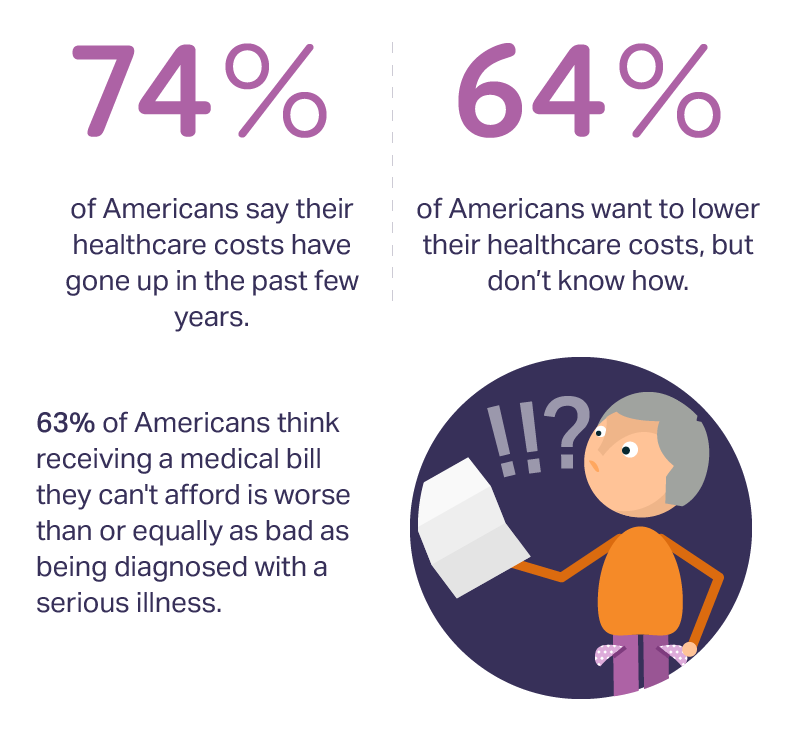
3 in 4 Americans’ health care costs have risen in the past few years. Two-thirds of Americans want to lower their costs, but don’t know how to do that. A survey from Amino released this week, conducted by Ipsos, has found that one in five people could not afford to pay an unexpected medical bill without taking on debt, and another 18% of Americans could only afford up to $100 if presented with an unexpected medical bill. This medical debt side effect more likely impacts women versus men, the less affluent, the unmarried, and those with no college degree. While
Will Republican Healthcare Policy “Make America Sick Again?” Two New Polls Show Growing Support for ACA

Results of two polls published in the past week, from the Kaiser Family Foundation and Pew Research Center, demonstrate growing support for the Affordable Care Act, aka Obamacare. The Kaiser Health Tracking Poll: Future Directions for the ACA and Medicaid was published 24 February 2017. The first line chart illustrates the results, with the blue line for consumers’ “favorable view” on the ACA crossing several points above the “unfavorable” orange line for the first time since the law was signed in 2010. The margins in February 2017 were 48% favorable, 42% unfavorable. While the majority of Republicans continue to be solidly
From EHRecords to EHDelivery: Talking With Dr. Roy Schoenberg of American Well

Telehealth has come of age at HIMSS in 2017. No longer is the concept relegated to footnote or edge-booth status on the conference floor. Instead, telehealth, broadly defined, is now a mainstream concept embraced by healthcare providers, payors and, increasingly, consumers. I spent time brainstorming telehealth with one of the pioneers of modern telehealth in the U.S., Dr. Roy Schoenberg, who co-founded American Well with his brother Ido Schoenberg, in 2007. As such, the company is among the most mature telehealth entities operating in America, delivering live video health visits to millions of health consumers through the American Well telehealth
Healthcare and the Autonomous Car: Setting the Stage for HIMSS17

The autonomous car is a metaphor for healthcare: that’s how my first interview kicking off the HIMSS marathon began. The annual 2017 HIMSS conference isn’t your father’s or mother’s HIMSS of ten years ago, or even the HIMSS of 2010 — the year that financial incentives for EHR adoption began to stream from the HITECH Act of 2009, motivating thousands of healthcare providers to acquire and meaningfully use digital health records systems. Then, the HIMSS conference floor was abuzz with EHR frenzy. This week, over 43,000 people working at the intersection of healthcare and technology have converged in Orlando, Florida, for
How Amazon Has Primed Healthcare Consumers

We are all Amazon Prime primed as consumers now. So it should not surprise healthcare providers, plans and suppliers that consumers expect just-in-time convenience for their healthcare, Accenture has found. Mind the gap: 8 in 10 U.S. patients would welcome some aspect of virtual healthcare, but only 1 in 5 providers is meeting that need. The consumer demand for virtual care is palpable for: Tracking biometrics, among 77% of consumers (say, for measuring blood pressure or blood glucose for people managing diabetes) Following up appointments, for 76% of people after seeing a doctor or being discharged from hospital Receiving reminders
My $100 Flu Shot: How Much Paper Waste Costs U.S. Healthcare

An abbreviated version of this post appeared in the Huffington Post on 9 February 2017. This version includes the Health Populi Hot Points after the original essay, discussing the consumer’s context of retail experience in healthcare and implications for the industry under Secretary of Health and Human Services Tom Price — a proponent of consumer-directed healthcare and, especially, health savings accounts. We’ll be brainstorming the implications of the 2016 CAQH Index during a Tweetchat on Thursday, February 16, at 2 pm ET, using the hashtag #CAQHchat. America ranks dead-last in healthcare efficiency compared with our peer countries, the Commonwealth Fund
Patients Anxiously Prep to Be Healthcare Consumers, Alegeus Finds

Healthcare consumers are in a “state of denial,” according to research conducted for Alegeus, the consumer health benefits company. Overall, 3 in 4 consumers feel fear when it comes to their healthcare finances: most people worry about being hit with unexpected healthcare costs they can’t afford, and nearly half fear they won’t be able to afford their family’s healthcare needs. The wordle illustrates consumers’ mixed feelings about healthcare: while people feel frustrated, overwhelmed, powerless, confused and skeptical about healthcare in America, there are some emerging adjectives hinting at growing consumer health muscle-building: optimistic, hopeful, supported, engaged, accountable. Still, denial and
Medical Debt Is A Risk Factor For Consumers’ Financial Wellness
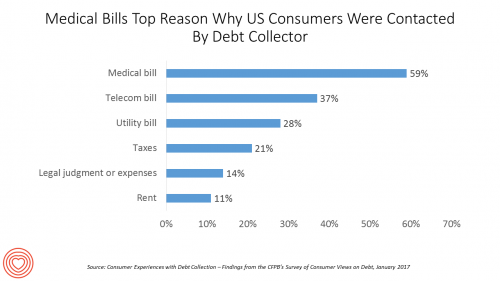
The top reason US consumers hear from a debt collector is due to medical bills, for 6 in 10 people in Americans contacted regarding a collection. This month, the Consumer Financial Protection Bureau (CFPB) published its report on Consumer Experiences with Debt Collection. Medical bill collections are the most common debt for which consumers are contacted by collectors, followed by phone bills, utility bills, and tax bills. The prevalence of past-due medical debt is unique compared with these other types because healthcare cost problems impact consumers at low, middle, and high incomes alike. Specifically: 62% of consumers earning $20,000 to
You Don’t Know What You’ve Got ‘Til It’s Gone: More Americans Liking the ACA
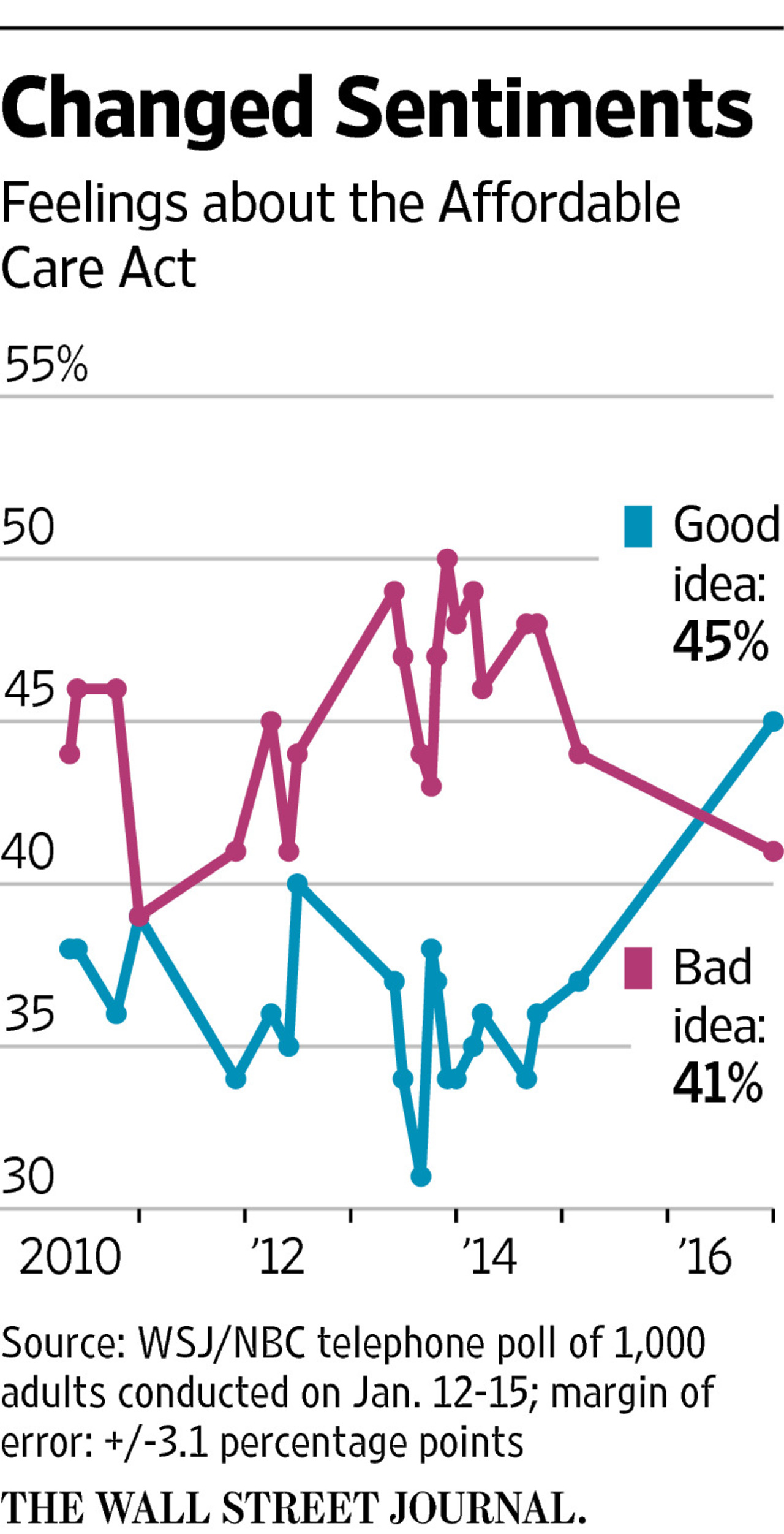
It’s human nature to take what we have for granted. But it wasn’t all that long ago that millions of Americans were uninsured. Since the advent of the Affordable Care Act (ACA), American voters’ feelings about the plan were split roughly 50/50, with slightly more U.S. voters, at the margin, disliking Obamacare than liking it. “Don’t it always seem to go that you don’t know what you’ve got ’til it’s gone,” Joni Mitchell sang in her iconic song, “Big Yellow Taxi.” In the lyrics, Mitchell was referring back in 1970 to land development and eroding public green space. “You paved
Pharma’s Branding Problem – Profits Over Patients
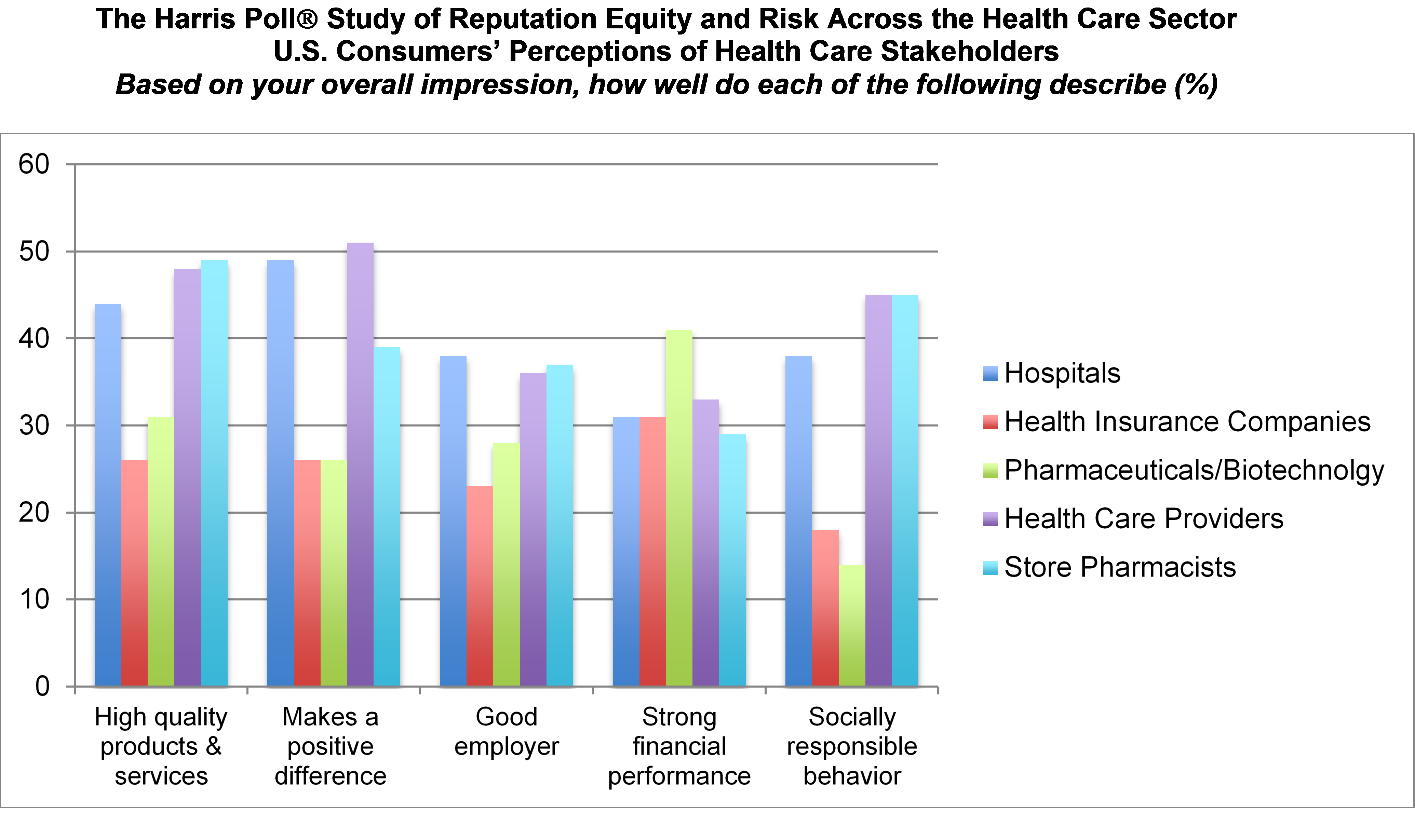
Nine in 10 U.S. consumers think pharma and biotech put profits above patient interests, according to the latest Harris Poll studying reputation equity across organizations serving health care. Notice the relatively low position of the green bars in the first chart (with the exception of the impression for “strong financial performance); these are the pharma/biotech consumer impressions. The health industry stakeholders consumers believe would more likely place them above making money are health care providers, like doctors and nurses, hospitals, and pharmacists. Health insurance companies fare somewhat better than pharma and biotech in this Poll, although rank low on social
The Shift to Healthcare Value in a Post-Trump America, via PwC
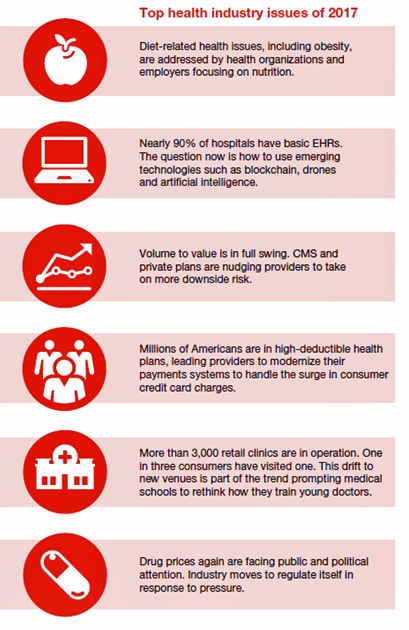
In President Donald Trump’s preliminary thoughts about health care in America, the landscape would feature a mix of tax credits, health savings accounts, high-risk pool, state Medicaid block grants, and regulatory control shifting from the Federal government to the states, according to PwC’s forecast for the new year, Top health industry issues of 2017. PwC frames the 2017 top healthcare issues under the overall strategic imperative of value, with three categories: Adapting for value Innovating for value Building for value. The ten top issues that will shape U.S. healthcare for the next year, PwC expects, will be: An uncertain fate for the
Health Is Personal at the Connected Health Summit

“Because health is personal” is the tagline at the 2016 Connected Health Conference being held at the Gaylord Resort in National Harbor in metro Washington, DC. “Personal,” “Connected,” and “Health” are the three words that comprise the adjectives in the Personal Connected Health Alliance, the host of this conference. PCHA was formed through the merger of HIMSS, the health IT association, and Continua, the organization advocating for health technology “interoperability” — the ability for digital and communications technologies to communicate with each other, to remove friction from health data exchange. This week, PCHA announced that it will bring the Wireless-Life Sciences Alliance into
You Better Watch Out, You Better Not Cry, Pharma: Donald Trump is Coming to Town

Based on a TIME magazine interview conducted today with President-Elect Donald Trump, the pharmaceutical and life science industries may expect to find coal in their Christmas stocking, and tougher pricing constraints in 2017. “I’m going to bring down drug prices,” Mr. Trump said, quoted on the TIME website naming him Person of the Year. “I don’t like what’s happened with drug prices.” As CNN put it, “Trump put the entire drug industry on notice on Wednesday in an interview with Time.” In fact, Donald Trump’s campaign website talked about drug importation as one potential tactic consumers could potentially use to
The Digital Health Gap For High-Cost, High-Need Patients
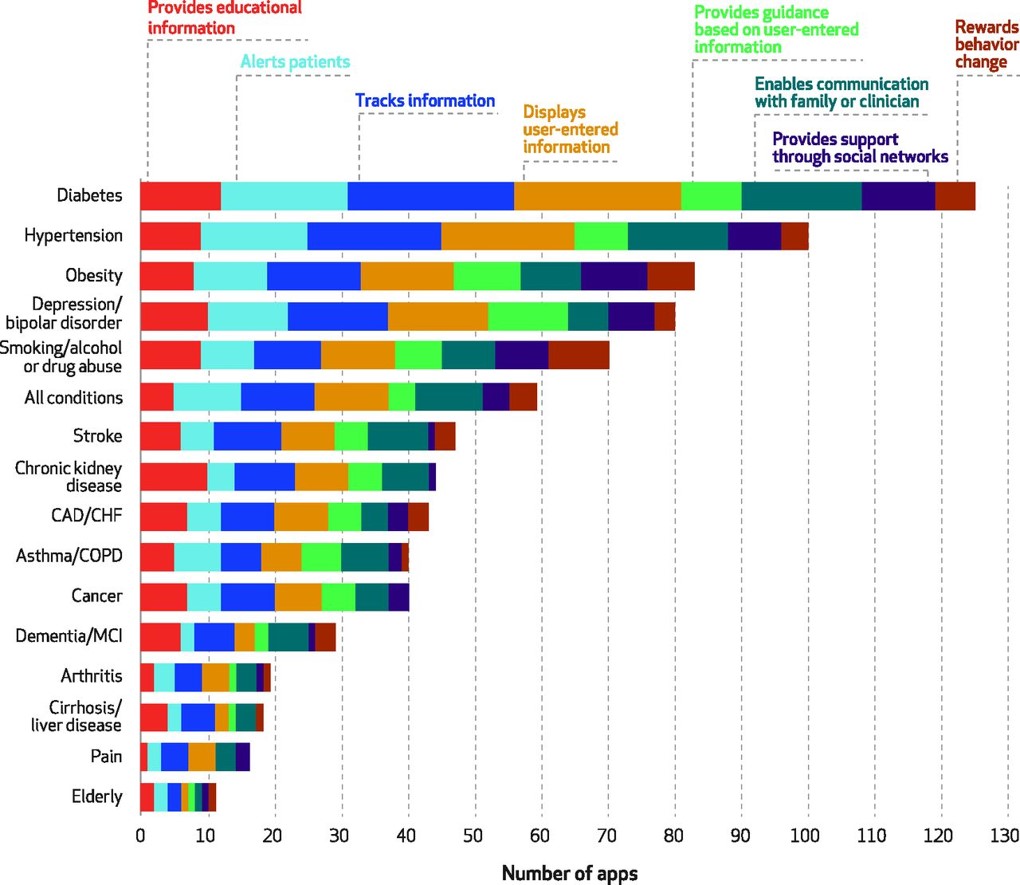
Several market forces are converging that boost patients’ ability to engage in their health and self-care, including peoples’ growing adoption of smartphones, demand for self-service and DIY lifestyles, and Americans’ growing responsibility as health consumers. Health consumers are using a growing array of self-health tools, enabled through digital technologies. However, these tools aren’t yet engaging some of the very people who need them the most: high-need, high-cost patients. Research into this situation is discussed in the December 2016 Health Affairs article, Many Mobile Heaath Apps Target High-Need, High-Cost Populations, But Gaps Remain, published in the December 2016 issue of Health Affairs. For
A Growing Medicines Bill for Global Health Consumers to 2021
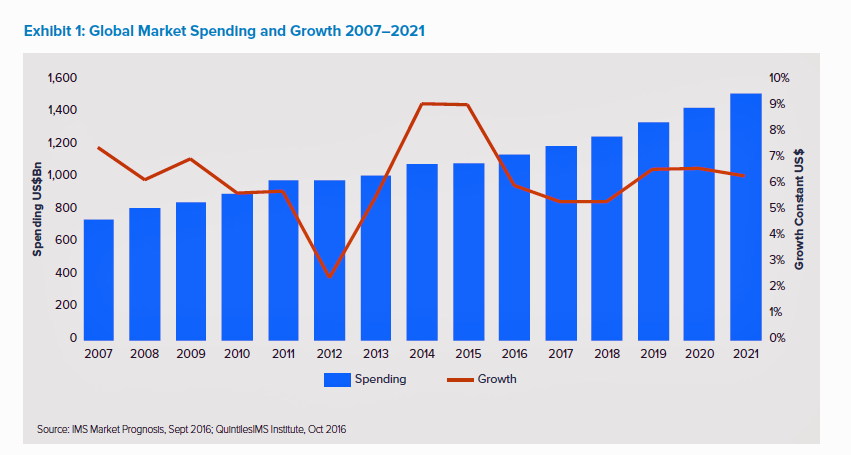
The global market for spending on medicines will high $1.5 trillion by 2021, according to the latest forecast from QuintilesIMS. Drug spending grew about 9% in the past two years, and is expected to moderate to 4 to 7 percent annually over the next five years. That dramatic 9% growth was heavily driven by new (expensive) specialty drugs to treat Hepatitis C (e.g., Harvoni and Sovaldi) and cancer therapies that hit the market in the past couple of years. There will be a “healthy level” of new innovative meds coming out of the drug pipeline in the next several years
U.S. Healthcare Spending Hit Nearly $10,000 A Person In 2015
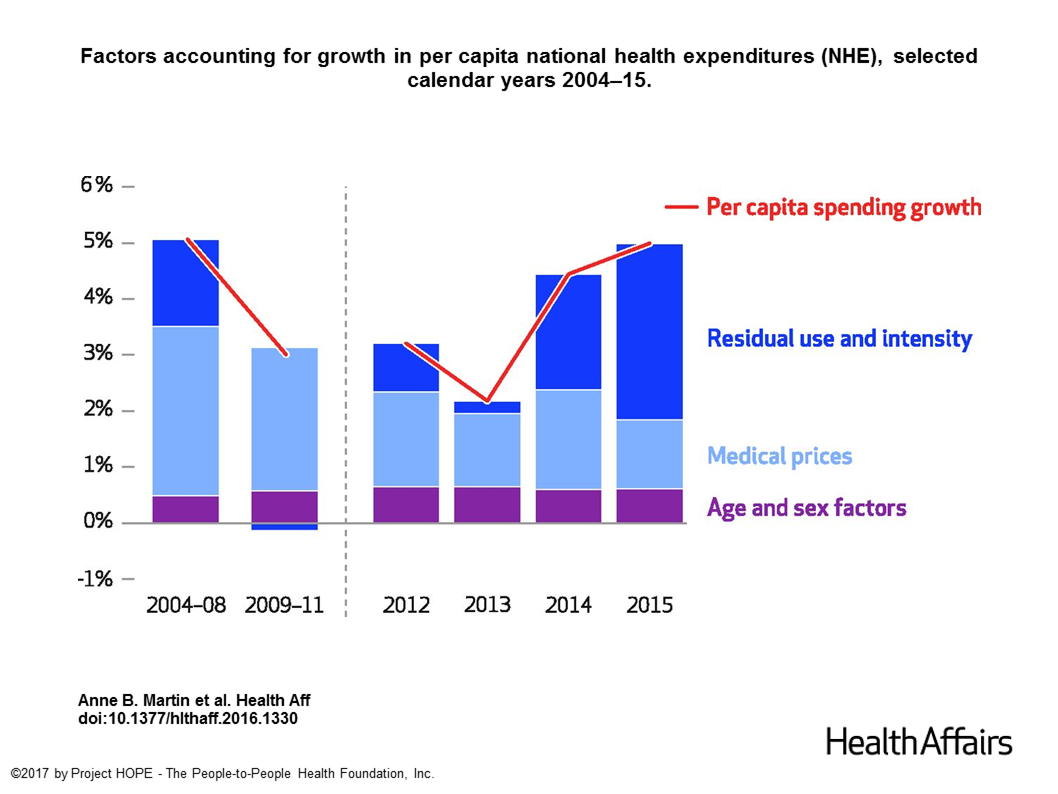
Spending on health care in the U.S. hit $3.2 trillion in 2015, increasing 5.8% from 2014. This works out to $9,990 per person in the U.S., and nearly 18% of the nation’s gross domestic product (GDP). Factors that drove such significant spending growth included increases in private health insurance coverage owing to the Affordable Care Act (ACA) coverage (7.2%), and spending on physician services (7.2%) and hospital care (5.6%). Prescription drug spending grew by 9% between 2014 and 2015 (a topic which I’ll cover in tomorrow’s Health Populi discussing IMS Institute’s latest report into global medicines spending). The topic of
See Me, Feel Me, Touch Me, Heal Me – What The Who’s Tommy Can Teach Healthcare
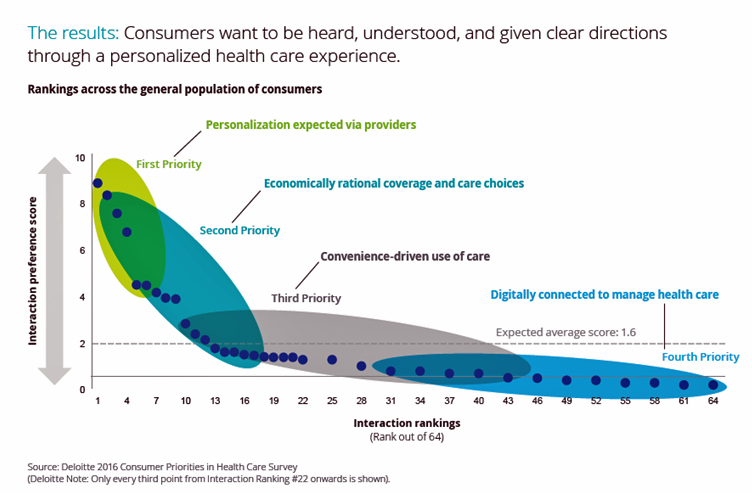
“See me, feel me, touch me, heal me,” is the lyrical refrain from The Who’s Tommy. These eight words summarize what Deloitte has learned from the firm’s latest look into healthcare consumers, published in the report, Health plans: What matters most to the health care consumer. U.S. consumers’ demands for health care are for: Personalization from doctors, hospitals, and other care providers — the most important priority; Economically rational coverage and care choices; Convenience-drive access and care experience; and, Digitally connected care. Personalization is Job 1: “Consumers want to be heard, understood, and given clear directions through a personalized health care
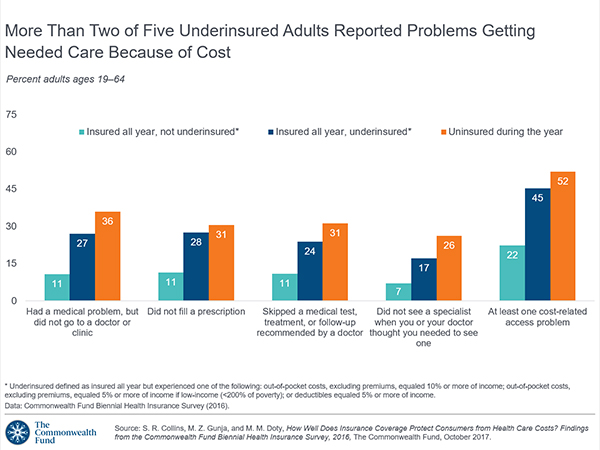
1 in 3 Americans Still Self-Rations Healthcare
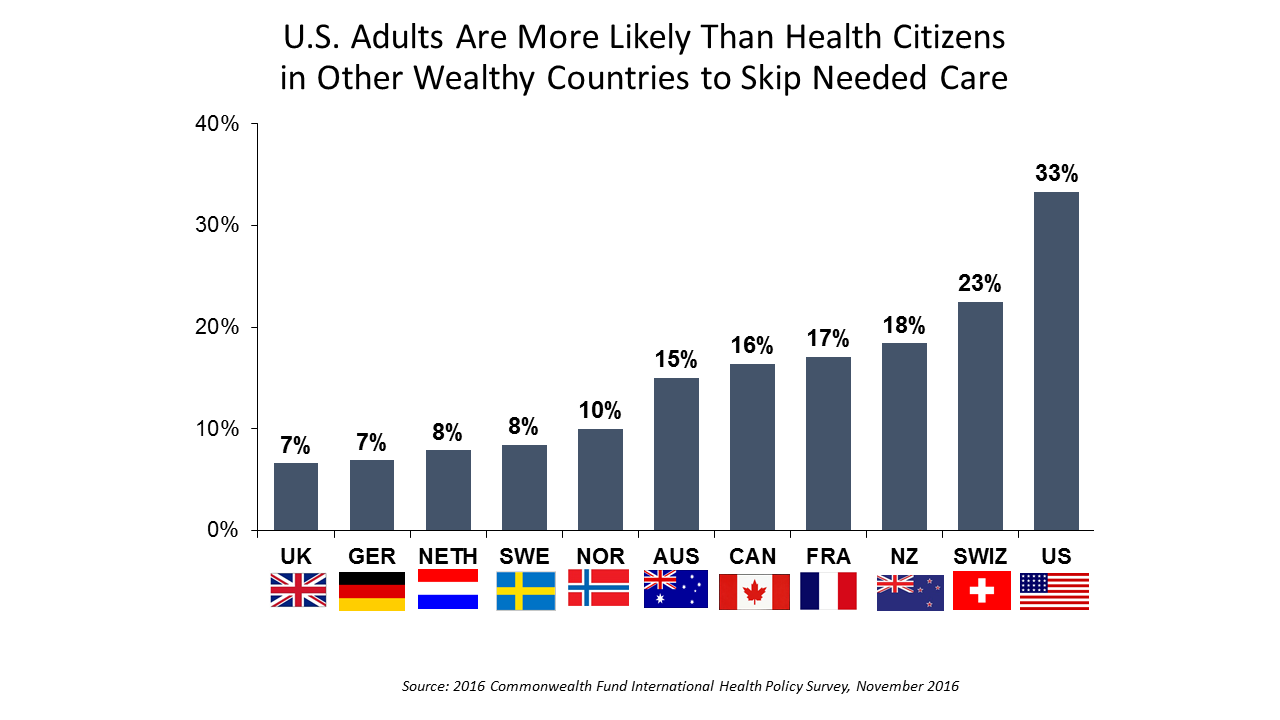
People in the U.S. are much more likely to go without health care they need compared with health citizens in 10 other wealthy countries, according to the Commonwealth Fund’s 2016 international survey. One-third of Americans did not seek care due to costs, including going without recommended care, failing to fill a prescription drug, and/or not seeing a doctor when sick. While this self-rationing proportion of Americans dropped from 37% in 2013, the U.S. still ranks #1 in foregoing necessary healthcare due to cost. “In comparison to adults in the other 10 countries, adult sin the U.S. are sicker and more
The Patient Is The Best Sensor – Consumers At the Center of Health

“The patient is the best sensor,” asserted Jamie Heywood, founder of Patients Like Me, during the perennial meeting sponsored by PwC, the 180° Health Forum. This event featured several panels of PwC’s curated group of so-called “provocateurs” in healthcare, and I was grateful to be one of nine selected for the event. Heywood joined Dr. Leanna Wen, Baltimore City Health Commissioner, and me in a panel called, “Strange Bedfellows or Soul Mates? The New Dating Game in Health.” The theme of our collective brainstorm was how collaborations across the ecosystem could help make health and healthcare better. The drawing is
Hospitals Need to Cross the Health Consumer Chasm
Most U.S. hospitals have not put consumerism into action, a new report from KaufmanHall and Caden’s Consulting asserts from the second paragraph. Patient experience is the highest priority, but has the biggest capability gap for hospitals, the report calls out. KaufmanHall surveyed 1,000 hospital and health system executives in 100 organizations to gauge their perspectives on health consumers and the hospital’s business. KaufmanHall points out several barriers for hospitals working to be consumer-centered: Internal/institutional resistance to change Lack of urgency Competing priorities Skepticism Lack of clarity (vis-a-vis strategic plan) Lack of data and analytics. The key areas identified for consumer centricity
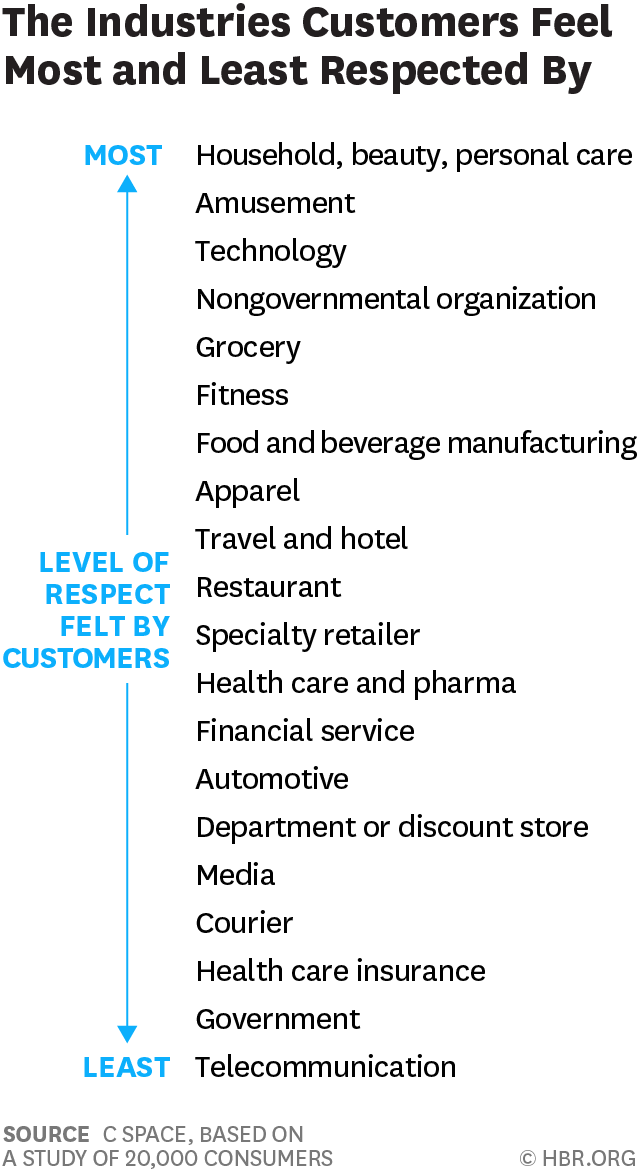
Consumers Feel More Respect from Personal Care and Grocery Brands Than Pharma or Insurance
People feel like get-no-respect Rodney Dangerfield when they deal with health insurance, government agencies, or pharma companies. Consumers feel much more love from personal care and beauty companies, grocery and fitness, according to a brand equity study by a team from C Space, published in Harvard Businss Review. As consumer-directed health care (high deductibles, first-dollar payments out-of-pocket) continues to grow, bridging consumer trust and values will be a critical factor for building consumer market share in the expanding retail health landscape. Nine of the top 10 companies C Space identified with the greatest “customer quotient” are adjacent in some way to health:
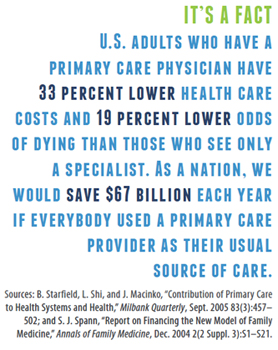
Building the Primary Care Dream Team
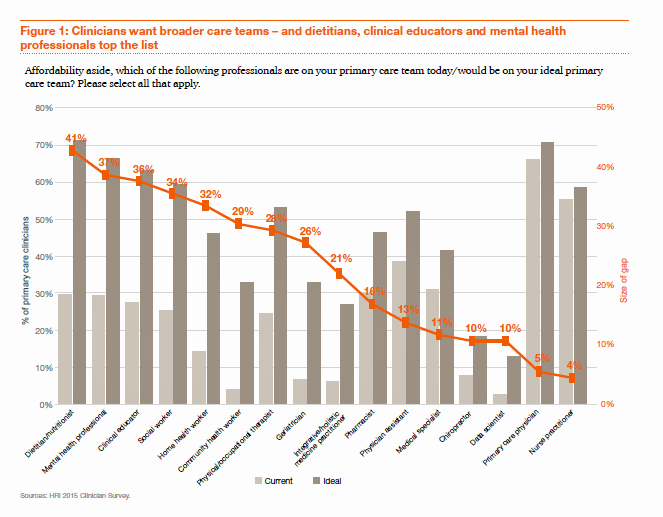
“Today’s primary care won’t work tomorrow,” given the shortage of primary care providers (PCPs) and the need to do more in healthcare with fewer resources in the emerging value-based economy. So let’s re-imagine primary care models, PwC asserts, and makes the case in their report, ROI for primary care: Building the dream team. What’s the financial impact of this dream team on healthcare providers? It’s potentially $1.2 million in savings for every 10,000 patients served, PwC calculates. Historically, physicians have been loath to share their work with non-physicians because of how doctors have been paid — on the basis of fee-for-service,
How Value and Consumerism Will Reshape the $5 Trillion Healthcare Market
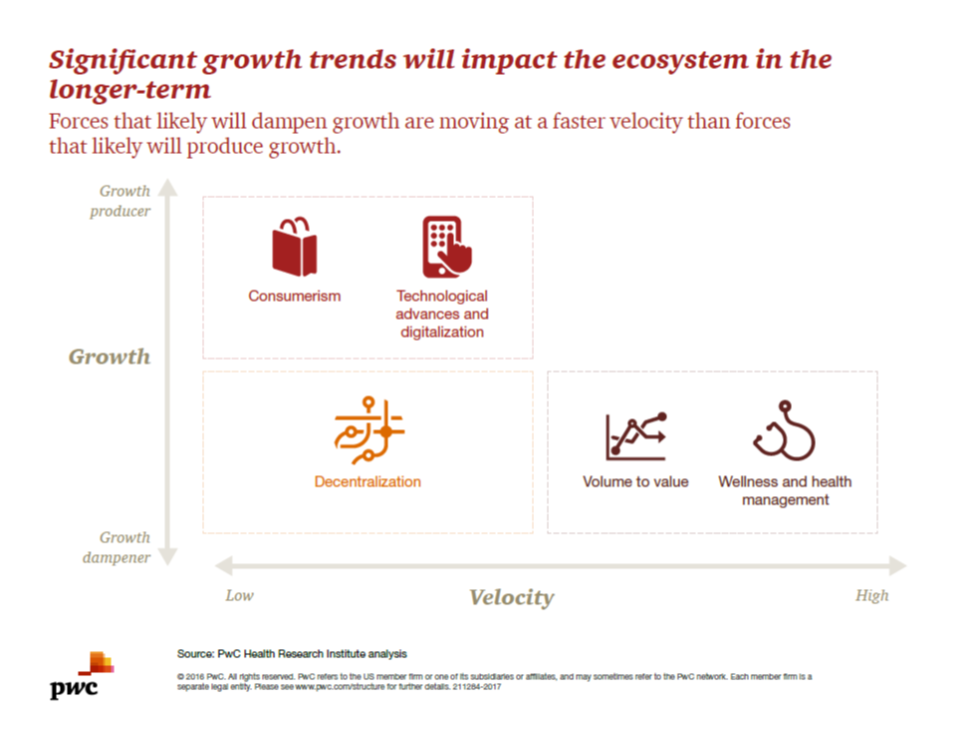
Existing healthcare industry players – the stakeholders of hospitals, physicians, pharma/life sciences, medical device manufacturers, and health plans – are operating in a whirlwind of change. While there are many uncertainties in this period of transition, there’s one operational certainty: learn to do more with less payment. That’s due to the growing pursuit of payors paying for value, not on the basis of volume or what’s “done” to a patient in care delivery. At the same time, another force re-shaping healthcare is interest and focus on wellness and health management. Combined with the growing health economic value proposition, wellness and
Let’s Go Healthcare Shopping!
Healthcare is going direct-to-consumer for a lot more than over-the-counter medicines and retail clinic visits to deal with little Johnny’s sore throat on a Sunday afternoon. Entrepreneurs recognize the growing opportunity to support patients, now consumers, in going shopping for health care products and services. Those health consumers are in search of specific offerings, in accessible locations and channels, and — perhaps top-of-mind — at value-based prices as defined by the consumer herself. (Remember: value-based healthcare means valuing what matters to patients, as a recent JAMA article attested). At this week’s tenth annual Health 2.0 Conference, I’m in the zeitgeist
Older Couples Have Lower Out-of-Pocket Healthcare Costs Than Older Singles
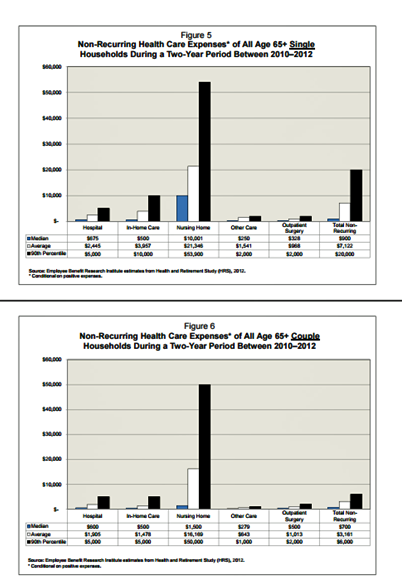
It takes a couple to bend the health care cost curve when you’re senior in America, according to the EBRI‘s latest study into Differences in Out-of-Pocket Health Care Expenses of Older Single and Couple Households. In previous research, The Employee Benefit Research Institute (EBRI) has calculated that health care expenses are the second-largest share of household expenses after home-related costs for older Americans. Health care costs consume about one-third of spending for people 60 years and older according to Credit Suisse. But for singles, health care costs are significantly larger than for couples, EBRI’s analysis found. The average per-person out-of-pocket spending for
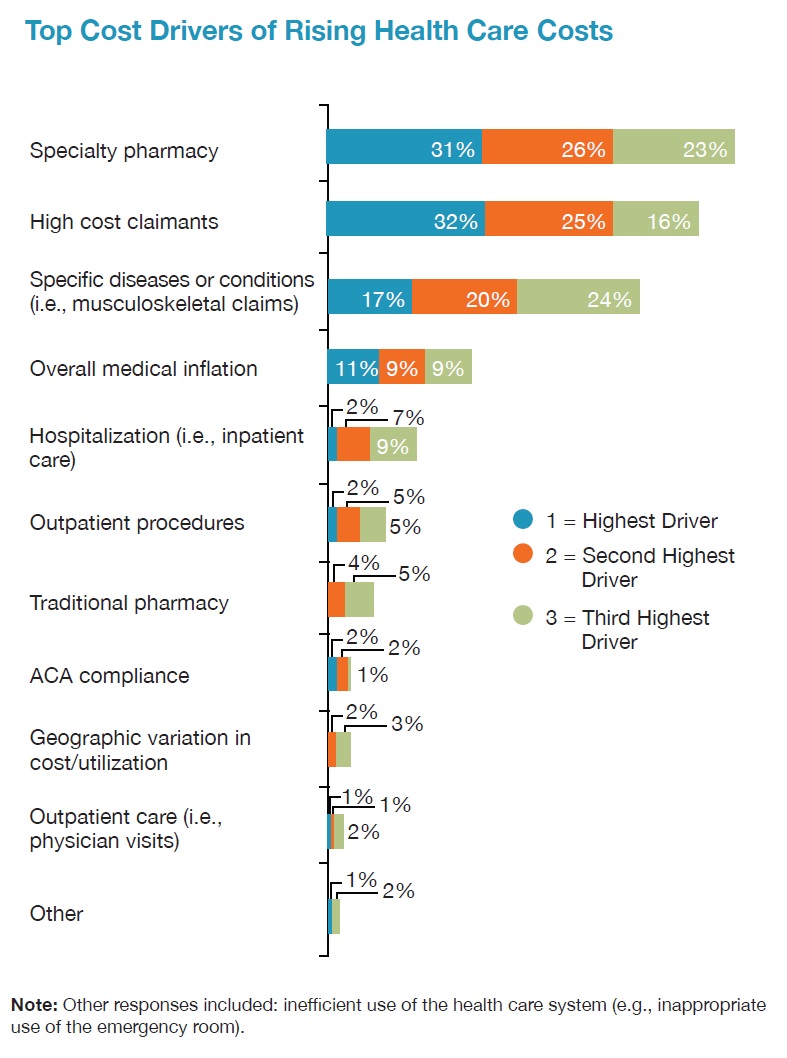
Employers Changing Health Care Delivery – Health Reform At Work
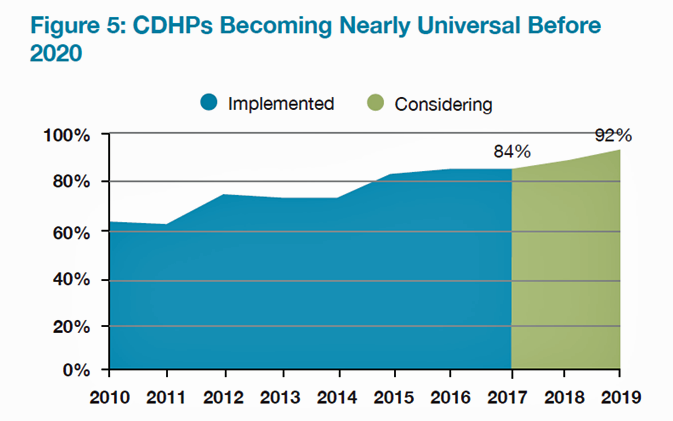
Large employers are taking more control over health care costs and quality by pressuring changes to how care is actually delivered, based on the results from the 2017 Health Plan Design Survey sponsored by the National Business Group on Health (NBGH). Health care cost increases will average 5% in 2017 based on planned design changes, according to the top-line of the study. The major cost drivers, illustrated in the wordle, will be specialty pharmacy (discussed in yesterday’s Health Populi), high cost patient claims, specific conditions (such as musculoskeletal/back pain), medical inflation, and inpatient care. To temper these medical trend increases,
PhRMA vs. Employers: Healthcare Costs In the Eye of the Beholder
In the past week, the Pharmaceutical Research and Manufacturers of America (PhRMA), the advocacy organization for the branded prescription drug industry, published Medicines: Costs in Context,” the group’s lens on the value of prescription drugs in the larger healthcare economy. Their view: that prescription drug costs comprise a relatively low share of health care spending in America, and a high-value one at that. PhRMA contends that 10% of the health care dollar was allocated to prescription drugs in 2015, the same proportion as in 1960. “Even with new treatments for hepatitis C, high cholesterol and cancer, spending on retail prescription
Most US Doctors Say They Ration Patients’ Healthcare
Rationing has long been seen as a common practice in national, single-payer health systems like the UK’s National Health Service and Canada’s national health insurance program (known as “Medicare”). However, over half of U.S. physicians say they ration care to patients. In a peer-reviewed column in the Journal of General Internal Medicine published in July 2016, Dr. Robert Sheeler and colleagues at the Mayo Clinic, University of Iowa, and University of Michigan, found that 53% of physicians surveyed personally “refrained” in the past six months from using specific clinical services that would have provided the “best patient care” due to cost.
The Future of Retail Health in 2027
As consumers gain more financial skin in the game of paying for health care, we look for more retail-like experiences that reflect the Burger King approach to consuming: having it our way. For health are, that means access, convenience, transparency and fair costs, respect for our time, and a clear value proposition for services rendered. That doesn’t happen so much in the legacy health care system — in hospitals and doctors’ offices. It has already begun to happen in retail health settings and, especially, in the changing nature of pharmacies. Retail Health 2027, a special supplement to Drug Store News
US Health Care Prices Would Be Sticker-Shocking For Europeans
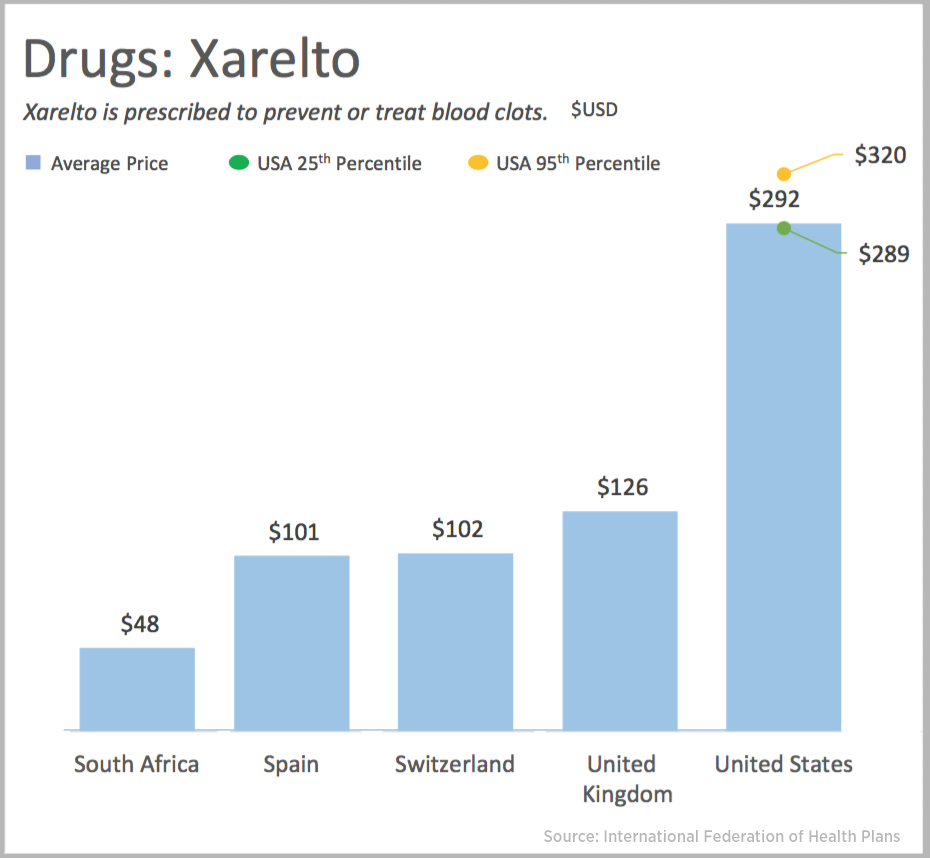
The average hospital cost per day in the U.S. is $5,220. In Switzerland it’s $4,781, and in Spain that inpatient day looks like a bargain at $424. An MRI in the U.S. runs, on average, $1,119. In the UK, that MRI is $788, and in Australia, $215, illustrated in the first chart. Drug prices are strikingly greater in the U.S. versus other developed nations, as shown in the first chart for Xarelto. If you live in the U.S. and have a television tuned in during the six o’clock news, chances are you’ve seen an ad for this drug featuring Arnold
Retail Clinics Continue to Shape Local Healthcare Markets
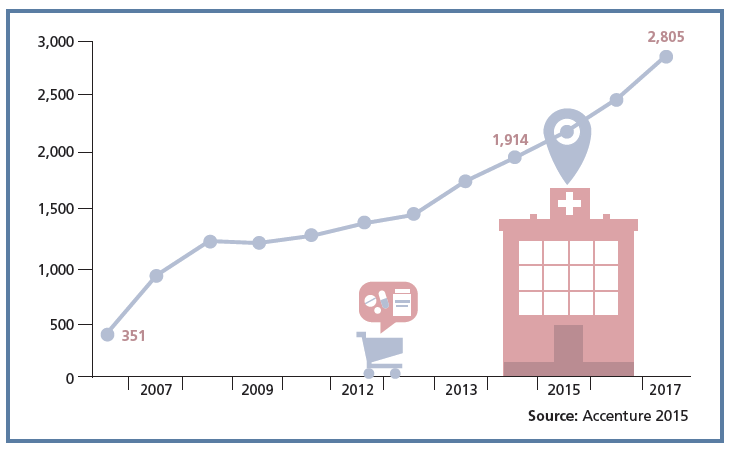
Retail clinics are a growing source of primary care for more U.S. health consumers, discussed in a review of retail clinics published by Drug Store News in July 2016. There will be more than 2,800 retail clinics by 2018, according to Accenture’s tea leaves. Two key drivers will bolster retail clinics’ relevance and quality in local health delivery systems: Retail clinics’ ability to forge relationships with legacy health care providers (physicians, hospitals); and, Clinics’ adoption and effective use of information technology that enables data sharing (e.g., to the healthcare provider’s electronic health records system) and data liquidity (that is, securely moving
U.S. Health Spending Will Comprise 20% of GDP in 2025
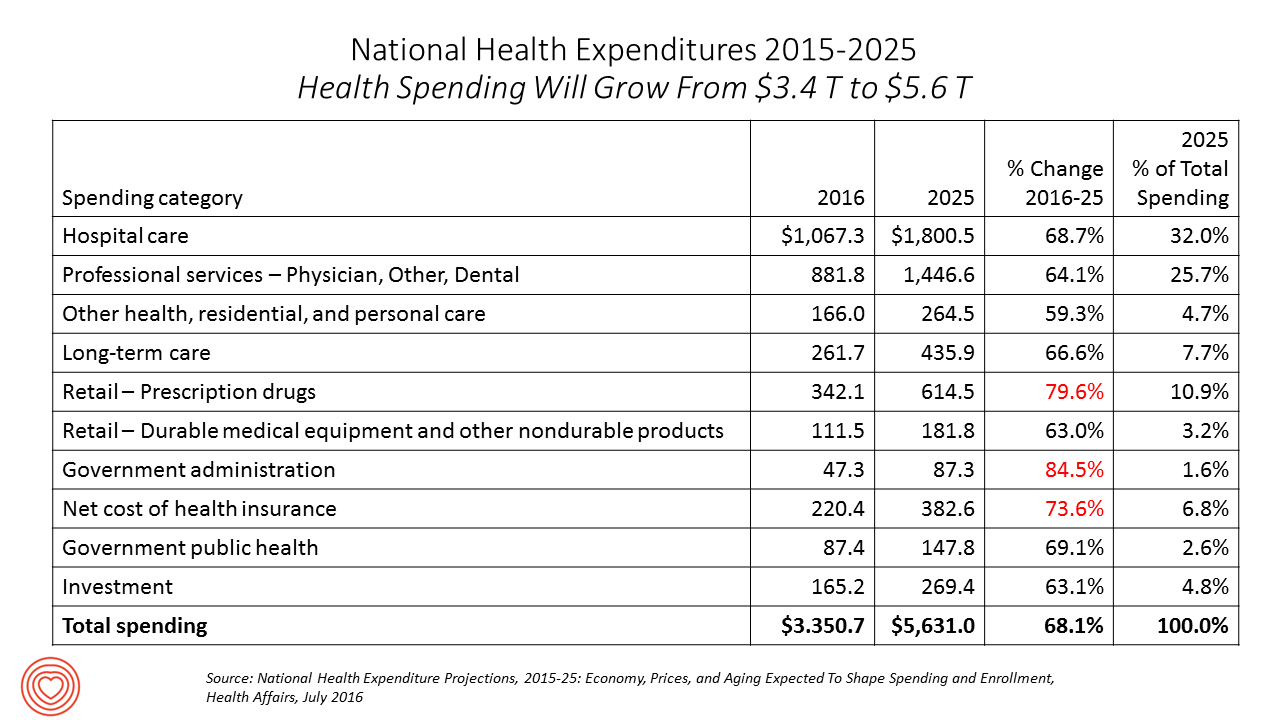
Spending on health care in America will comprise $1 in every $5 of gross domestic product in 2025, according to National Health Expenditure Projections, 2015-25: Economy, Prices, And Aging Expected to Shape Spending and Enrollment, featured in the Health Affairs July 2016 issue. Details on national health spending are shown by line item in the table, excerpted from the article. Health spending will grow by 5.8% per year, on average, between 2015 and 2025, based on the calculations by the actuarial team from the Centers for Medicare and Medicaid Services (CMS), authors of the study. The team noted that the Affordable Care
In Healthcare, Pharmacists and Doctors Most Trusted. Insurance Execs and Congress? Not.
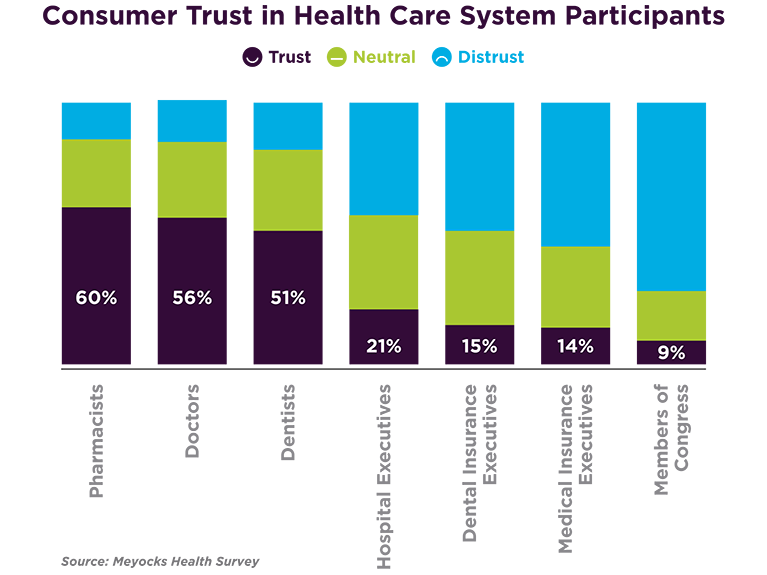
When consumers consider the many stakeholder organizations in healthcare, a majority trust pharmacists first, then doctors and dentists. Hospital and health insurance execs, and members of Congress? Hardly, according to a survey from Meyocks, a marketing consultancy. Meyocks conducted the survey via email among 1,170 US adults, 18 years of age and older. This survey correspondends well with the most recent Gallup Poll on most ethical professions, conducted in December 2015. In that study, pharmacists, nurses and doctors come out on top, with advertisers (“Mad Men”), car salespeople, and members of Congress at the bottom, as shown in the second
More Patients Morph Into Financially Burdened Health Consumers
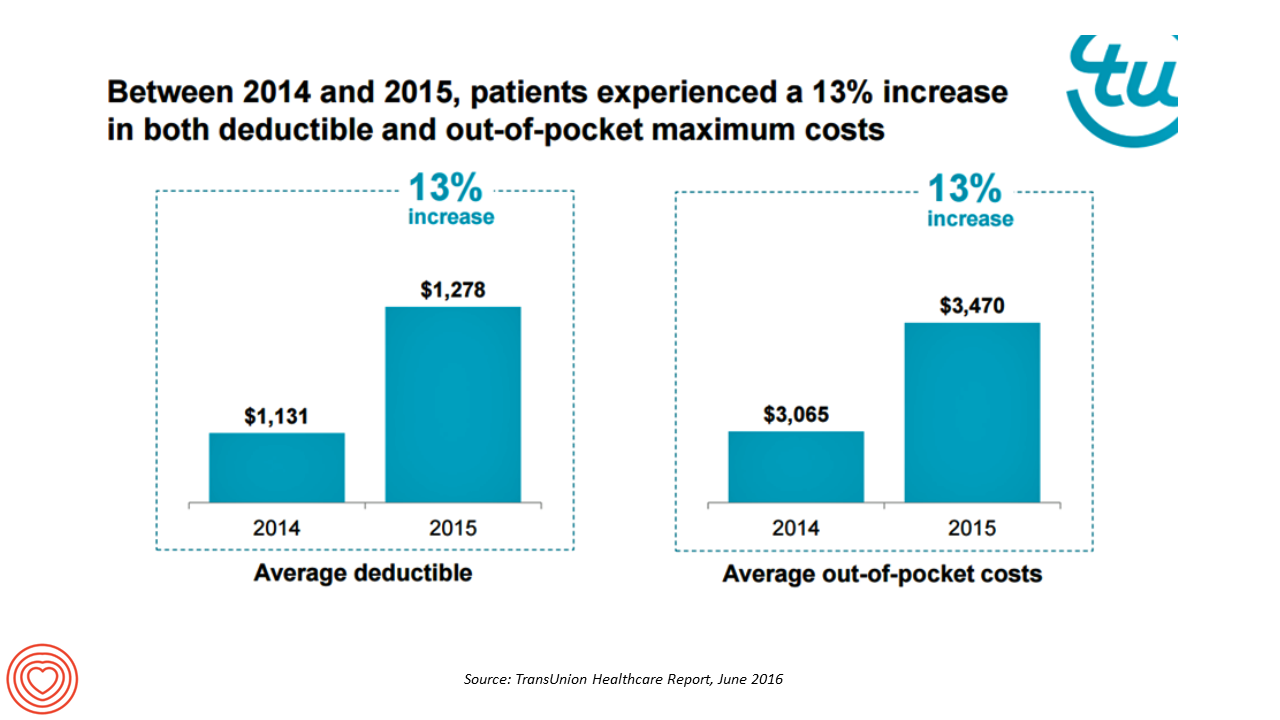
Health care payment responsibility continues to shift from employers to employee-patients, More of those patients are morphing into financially burdened health consumers, according to TransUnion, the credit agency and financial risk information company, in the TransUnion Healthcare Report published in June 2016. Patients saw a 13% increase in their health insurance deductible and out-of-pocket (OOP) maximum costs between 2014 and 2015. At the same time, the average base salary in the U.S. grew 3% in 2015, SHRM estimated. Thus, deductibles and OOP costs grew for consumers more than 4 times faster than the average base salary from 2014 to 2015. In
Accountable Care Will Happen Best When Patients Engage
Technology alone won’t improve health care in America, especially in people with chronic health problems don’t want to use it. Furthermore, too many clinicians who have invested in digital health technologies (namely, electronic health records systems), aren’t fully taking advantage of what they have. This and other health care realities are explored in Better Together: Patient Expectations and the Accountability Gap, based on a consumer survey conducted by Nielsen Strategic Health Perspectives for the Council of Accountable Physician Practices, an affiliate of the American Medical Group Foundation. The survey polled 30,007 consumers in March 2016, and combined physician data culled from Nielsen’s
Healthcare Consumerism? Not So Fast, Alegeus Finds
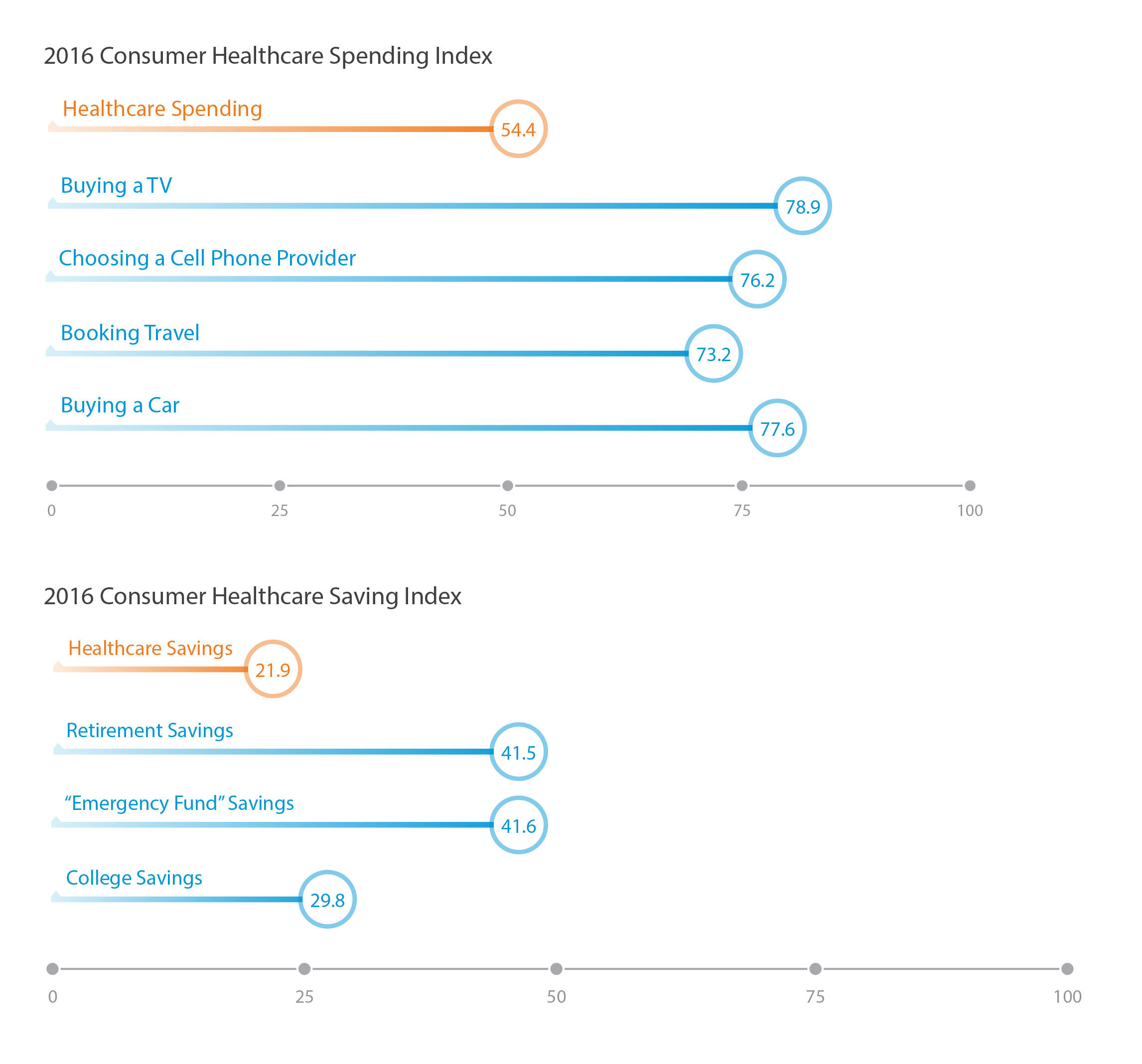
Millions of U.S. patients have more financial skin in the American health care game. But are they behaving like the “consumers” they are assumed to be as members in consumer-directed health plans? Not so much, yet, explained John Park, Chief Strategy Officer at Alegeus, during a discussion of his company’s 2016 Healthcare Consumerism Index. This research is based on an online survey of over 1,000 U.S. healthcare consumers in April 2016. Alegeus looks at healthcare consumerism across two main dimensions: healthcare spending and healthcare saving. As the chart summarizes, consumers show greater engagement and focus on buying a TV or car, choosing
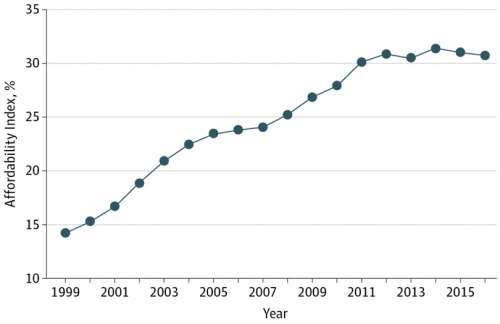
PwC’s “Behind the Numbers” – Where the Patient Stands
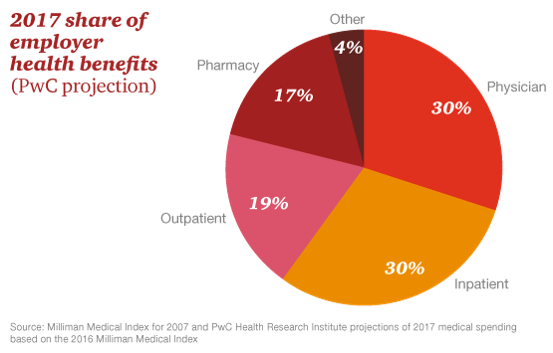
The growth of health care costs in the U.S. is expected to be a relatively moderate 6.5% in 2017, the same percentage increase as between 2015 and 2016, according to Medical Cost Trend: Behind the Numbers 2017, an annual forecast from PwC. As the line chart illustrates, the rate of increase of health care costs has been declining since 2007, when costs were in double-digit growth mode. Since 2014, health care cost growth has hovered around the mid-six percent’s, considered “low growth” in the PwC report. What’s driving overall cost increases is price, not use of services: in fact, health care





 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.