 While Congressfolk and political pundits await the President’s speech tonight about why and how to reform the health system, patients on-the-street and in-their-homes are getting on with their daily lives dealing with chronic diseases. In the U.S., 75% of health care costs annually go to ‘manage’ chronic conditions. That’s about $1.7 billion of the $2.2 billion spent on health care in 2007.
While Congressfolk and political pundits await the President’s speech tonight about why and how to reform the health system, patients on-the-street and in-their-homes are getting on with their daily lives dealing with chronic diseases. In the U.S., 75% of health care costs annually go to ‘manage’ chronic conditions. That’s about $1.7 billion of the $2.2 billion spent on health care in 2007.
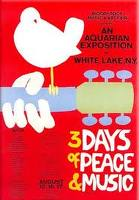
Not waiting for a government agency or health plan to provide a recipe for self-care, a cadre of highly engaged health citizens have taken care into their hands and minds. “Participatory health,” David Lester of Theranos told me, “is the new Woodstock.”
Participatory Health: Online and Mobile Tools Help Chronically Ill Manage Their Care is my latest issue brief written for the California HealthCare Foundation. The paper outlines the challenge of chronic care in America — the costs, the prevalence, the lack of aligned incentives — and explains how the enabling communications technologies, already being used by the masses, have begun to lay the foundation for patients to manage care at home and on-the-go, 24×7.
“Clinical settings can contribute to both environmental and individual behavior change,” Wiliam Novelli, former CEO of the AARP, said. “But people do not live in clinical settings. They live in supermarkets, convenience stores, schools, playgrounds, restaurants, offices and factories.”
That’s why participatory health can crack the difficult code of chronic disease. Look at the Care Model chart, developed by the Robert Wood Johnson Foundation project on chronic disease.
While patients spends mere minutes within the confines of the clinician’s exam room and in the so-called health system, people live, breathe, eat, work, and move in their own real worlds 24×7. Participatory health means mashing up lifestyles and numbers and clinical advice in a continuous stream that is personalized for the individual patient, and largely controlled by her with the input of clinical experts, coaches, personal physicians — trusted partners in customized care.
Participation in health is enabled today through peoples’ use of the Internet (enhanced through broadband connections) and mobile communications platforms (namely mobile phones). Health applications available at the iTunes store are among the fastest-growing categories available to iPhone users. Among many participatory health pioneers I feature in the report, you’ll learn about the developer Brett Shamosh whose Wellapps start-up was inspired by his own self-management of Crohn’s Disease. His apps are now available on iTunes.
Health Populi’s Hot Points: For participatory health to really take off in the mainstream, payment and incentives must align between providers, patients and other stakeholders. Incentives for many health citizens will include a fiscal and/or other-valued ‘nudge’ which keeps people on the participative health journey. Read in my report, for example, about Sensei’s approach to nudging on-the-go, involving customized couponing via phone for everything from fast food to jeans.
Participatory health is already here for uber-engaged patients and providers. Read about a long-distance truck driver, David Jesse, who with the help of a Microsoft HealthVault enabled PHR and The Cleveland Clinic, brought his blood pressure down to 120/82 as he drove the highways and byways of the U.S.
The long journey of managing chronic care can be made less arduous and more successful through participatory health care and the array of tools emerging to support people in managing their own care. Here’s health reform that starts at home.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.