Photographer John Fitzpatrick
Stylist
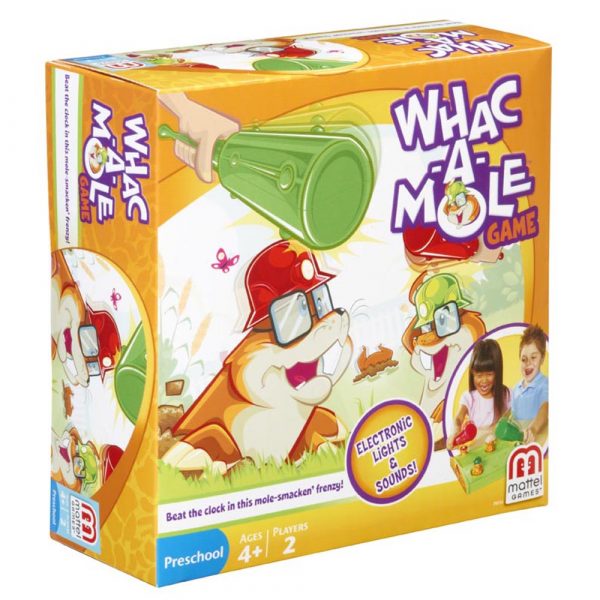
Did you ever play the whac-a-mole game? As Wikipedia describes it,
Dr. Trivedi, et. al., compared changes in utilization in outpatient and inpatient care among Medicare enrollees that increased copayments for ambulatory care. The researchers compared a controlled utilization between enrollees who had increased ambulatory care copayments versus those whose payments did not change.
The outcome: increasing copayments for ambulatory care services resulted in fewer outpatient visits by Medicare enrollees, and increasing inpatient admissions to hospitals.
Health Populi’s Hot Points: The conclusion we draw is that raising cost-sharing for ambulatory care can have adverse consequences — and ironically, drive health spending up.
This study speaks to the important art of value-based benefit design: art and, of course, actuarial science, too. The U.S. health system has a long history of whac-a-mole economics: when inpatient payment rates got cut for hospitals, for example, hospitals rushed to build ambulatory surgery centers and outpatient rehab facilities.
In the meantime, whac-a-mole will continue until those who design health plans recognize the nature of incentives and their consequences. For more on value-based benefit designs, check out Dr. David Hom‘s work at Healthcare Innovation as well as Health Affairs’ article by Michael Chernew et. al. on the evidence of value-based plan design.




 I'm gobsmackingly happy to see my research cited in a new, landmark book from the National Academy of Medicine on
I'm gobsmackingly happy to see my research cited in a new, landmark book from the National Academy of Medicine on 
 Grateful to Gregg Malkary for inviting me to join his podcast
Grateful to Gregg Malkary for inviting me to join his podcast