 The usual questions a rational health citizen might ask when selecting a physician based on quality aren’t consistently yielding the best choices, according to a study funded by The Commonwealth Fund, Associations Between Physician Characteristics and Quality of Care.
The usual questions a rational health citizen might ask when selecting a physician based on quality aren’t consistently yielding the best choices, according to a study funded by The Commonwealth Fund, Associations Between Physician Characteristics and Quality of Care.
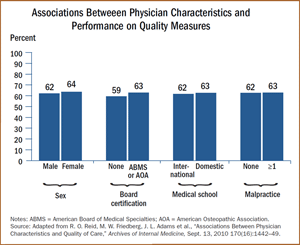
Researchers found that individual physician-comparative parameters such as malpractice claims and disciplinary actions, years in practice or medical school ranking had no significant association with better quality performance. Female physicians (vs. male) and Board certification had small significance, 1.6 points and 3.3 points, respectively.
This study’s results demonstrate that the metrics consumers assume should be useful proxies for physician quality aren’t as useful as they might have thought. On average, physicians provided 63% of recommended care based on community standard guidelines. This average varied based on conditions, with the low of 31% for cataract care to 68% for congestive heart failure.
The study was conducted by analyzing claims data from 1.13 million patients treated by 10,408 physicians in Massachusetts in 2004 and 2005. These data were compared with publicly available data on physicians’ characteristics from the Massachusetts Board of Registration in Medicine such as gender, medical school graduation date, board certification, and malpractice claim payments. The researchers are associated with RAND and the University of Pittsburgh School of Medicine.
Health Populi’s Hot Points: What’s the thoughtful, quality-seeking health citizen in the U.S. to do? The study authors say, “look to public reporting of individual quality data.”
People in the U.S. have been charged with taking on more personal and individual responsibility to seek health care and pay more out-of-pocket. This study demonstrates that people don’t have access to the necessary information they need to become fully engaged, well-informed consumers: full, useable, and complete information is a pre-cursor for a market to work (according to the economist’s definition of “market”). Thus, while we use the phrase ‘health consumer’ in the U.S., it’s clear we’re not yet ready for the playing that primetime role yet.
Public reporting of physician quality metrics may be the ‘place’ to go for such information, but those sources aren’t yet comprehensive and fully populated. Thus, health citizens in the U.S. will be forced to use the somewhat unhelpful proxy measures and word-of-mouth from friends and family –still a prevailing form of trusted quality reporting for many people.





 Grateful to Gregg Malkary for inviting me to join his podcast
Grateful to Gregg Malkary for inviting me to join his podcast  This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're
This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're