 Remote health monitoring, which enables people to track health and daily living metrics when they are in one place and communicate those measures to another node via some communications platform, is not a new concept. Telehealth, telemedicine, consumer-facing health electronics like USB-ported blood pressure monitors, and some mobile apps can all fall under the broad umbrella of remote health monitoring. There are strong market forces converging to enable health citizens to connect to their providers, institutions, payors, health coaches, caregivers, and each other.
Remote health monitoring, which enables people to track health and daily living metrics when they are in one place and communicate those measures to another node via some communications platform, is not a new concept. Telehealth, telemedicine, consumer-facing health electronics like USB-ported blood pressure monitors, and some mobile apps can all fall under the broad umbrella of remote health monitoring. There are strong market forces converging to enable health citizens to connect to their providers, institutions, payors, health coaches, caregivers, and each other.
Still, a balanced look under the remote health monitoring hood reminds us that old saw taught to me by colleagues at Institute for the Future: that we tend to overestimate the impact of a technology in the short run, and underestimate its effect in the long run. A variant on that is that objects ahead of you may seem to be closer than they are.
The Connected Patient: Charting the Vital Signs of Remote Health Monitoring, my latest white paper for the California HealthCare Foundation, was published this week during the HIMSS11 conference. The paper lays out the definition of RHM, the market drivers and barriers to its broad adoption, an examination of some of the evidence for major conditions (e.g., heart failure, diabetes, COPD, etc.), and prospects for the future.
The market drivers fostering the adoption of remote health monitoring include the emergence of bundled payment and value-based benefits that reward clinicians for ‘whole health’ caring; the chronic care tsunami, occurring with the advent of Baby Boomers aging; the primary care workforce shortage, which will force innovations like the use of distance health technologies; standards adoption for communications such as ZigBee and WiFi, among others that continue to be developed; Moore’s Law kicking in, pushing costs down for hardware and software; and consumers’ demand for convenience, access, and health innovations. That’s all good news for RHM.
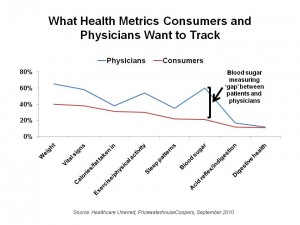
On the other side of the market adoption ledger are the obstacles preventing the use of RHM. First and foremost are several physician barriers: resistance to monitoring in general, which will be a novel and disruptive process for workflows; lack of incentives (that is, reimbursement/payment) to engage with remotely monitored patients; and, the challenge of what to do with the data generated by the devices doing the monitoring. This last point could be mitigated once a physician is using an electronic health record, which could become the data repository for the health metrics gathered by remote health devices. It’s important to note, too, that patients and physicians might be interested in monitoring different measures, as illustrated by the first chart.
A second category of resistance is among patients, for whom remote monitoring might disrupt personal “life flow.” Related to this is consumer health engagement: do people really want to be monitored, and once monitored, will people embrace “their numbers” and use this knowledge to modify health behaviors? A third stakeholder in this mix are hospitals, for which RHM might elicit ambivalent feelings. After all, hospitals’ lifeblood is patient admissions into beds, isn’t it? Perhaps that is Old School thinking, as in health reform (the Affordable Care Act, specifically) there are hard financial incentives for hospitals to avoid readmissions of patients with certain conditions: beginning in 2013, hospitals with readmission rates over the 75th percentile will have payments for the patient’s original admission reduced by 20% if that patient is rehospitalized with a preventable readmission within seven days.
Finally, there are technology obstacles that still haven’t been solved in RHM, such as the diversity of communications platforms in peoples’ homes, which can prevent hospitals’ RHM programs from easily scaling; and, telecommunications platforms which can also be so diverse and fragmented, especially in the U.S. market compared with European and Asian markets.
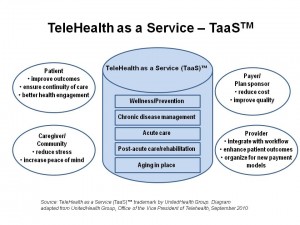 Health Populi’s Hot Points: Even considering these barriers, the forecast is bright for RHM, which can connect the many stakeholders in the patient/person’s health ecosystem. RHM can put the patient back in the center of their health care, and make the person’s home the true health hub and literal “medical home.” Increasingly, what were very expensive big-iron monitoring devices are becoming consumer-facing, well-designed and usable gadgets for people to use at home and on-the-go via mobile platforms, 24×7. As payment reforms align value and quality with outcomes, RHM becomes a no-brainer to adopt. As the market forces align over the next 12-36 months, consumers will learn about the value of RHM from early adopters (some from uber-engaged individuals in the Quantified Self Movement, others in health plans utilizing telehealth-as-a-service [TaaS] such as UnitedHealth Group).
Health Populi’s Hot Points: Even considering these barriers, the forecast is bright for RHM, which can connect the many stakeholders in the patient/person’s health ecosystem. RHM can put the patient back in the center of their health care, and make the person’s home the true health hub and literal “medical home.” Increasingly, what were very expensive big-iron monitoring devices are becoming consumer-facing, well-designed and usable gadgets for people to use at home and on-the-go via mobile platforms, 24×7. As payment reforms align value and quality with outcomes, RHM becomes a no-brainer to adopt. As the market forces align over the next 12-36 months, consumers will learn about the value of RHM from early adopters (some from uber-engaged individuals in the Quantified Self Movement, others in health plans utilizing telehealth-as-a-service [TaaS] such as UnitedHealth Group).
Patients, as people, are also adopting social models in health. Moving away from the traditional relationship of patient taking orders from the physician as trusted intermediary, more people are looking to partner with clinical experts (including and beyond their own personal physicians), as well as share perspectives and support with people like themselves (as patients or caregivers). Eric Dishman of Intel pointed out to me, and is quoted in the paper, that people get more engaged with their health when they see and understand their personal health data. “This (RHM) is not a surveillance model,” Dishman told me; “it’s a social model.”
But even when patients-people seek to engage in that social model, other forces can keep them from doing just that. Hugo Campos, who is a patient advocate fitted with an implantable cardioverter defibrillator, cannot access the data that continuously streams from the very device implanted in his chest. The manufacturer and industry, Campos believes, is preventing that from happening because, as he sees it, sharing the data, “doesn’t fit into their business model, since a pacemaker or defibrillator is put into a patient’s body for the therapy it delivers, not for the information it gathers.”
So some miles to go before full-on participatory, connected health is a reality. But make no mistake: the forecast is clear, and the roots and sub-terranean drivers setting the table for Connected Health are already in motion.




 Thank you FeedSpot for
Thank you FeedSpot for