About 1.3 million people in the U.S. experience a medication error each year, which are preventable events that may cause or lead to inappropriate medication use or harm a patient, any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the health care professional, patient, or consumer. Two very common causes of medication errors are illegible handwriting by prescribers and misplaced decimal points on prescription forms. Twenty percent of adverse drug events lead to life-threatening circumstances, according to The Leapfrog Group. The costs of medication errors has been estimated at $2 billion per year in hospital costs alone.
To Err is Human, the seminal report from the Institutes of Medicine, noted that medication errors cause 7,000 deaths a year in the U.S.
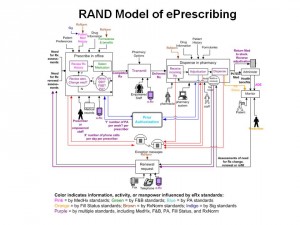
Electronic prescribing, or ePrescribing (eRx), allows prescribers (usually physicians) to use software that enables them to write-up and store prescriptions electronically. The objective is to reduce errors, improve physician practice and pharmacy productivity, and improve quality and patient outcomes. The first chart presents RAND‘s graphic representation of the ePrescribing process. As in most aspects of health care delivery, it’s not as simple as we might think it would be.
eRx systems also incorporate value-added functions beyond the electronic transmission of a prescription from a doctor’s point-of-prescribing to a pharmacy. These features can include patients’ entire medication history, access to a patient’s formulary and drug benefit information, and prescription drug alternatives (branded, generic, and oftentimes over-the-counter substitutes). This information can help round out the prescriber’s full picture of the patient and help determine the optimal choice for a prescription drug to be used in a particular patient.
Physician Practices, E-Prescribing and Accessing Information to Improve Prescribing Decisions, a report from the Center for Studying Health System Change (HSC), finds that the full potential for eRx hasn’t yet been realized within those practices who have adopted the practice. A study of Surescripts prescription data found that 62% of physicians had access to medication histories, but only 56% of these physicians used the histories “most or all of the time.” Don’t just blame un-engaged physicians for the lack of full-on use of eRx features: there’s also missing, incomplete and inaccurate data in the databases.
As physicians amp up their adoption and use of electronic health records (EHRs), ePrescribing will be part of demonstrating meaningful use of the systems in order to qualify for incentive payments in Stage 1. Being deep users of eRx will accelerate over the four years of meaningful use for incentives. Physicians can choose from a menu of several value-added functions for MU in Stage 1. Accessing and using formulary information and medication reconciliation may also ramp up in later stages of MU.
For now, though, physicians have a long way to go in fully realizing the benefits of ePrescribing. HSC identifies several factors that would advance ePrescribing’s potential:
- Increase data availability and usefulness. This would encourage commercial health insurers and Medicaid plans to provide more accurate and complete medication histories and formulary information that’s already in databanks for Medicare Part D. To do this, standardizing drug names would be critical – and industry adoption of the RxNorm technical standard for medication names could help move this forward. HSC notes that RxNorm is not part of MU for Stage 1, but writes that, “the federal government expressed interest in doing so in later stages.”
- Enhancing system design. Readers of Health Populi know of my keen interest in design in health. Good design which is co-created and -inspired by users helps ease adoption and foster sustained use of new (and particularly workflow-disrupting) technologies.
- Targeted physician education and training. Sustained use of new technologies is always bolstered by training and support. HSC calls out the roles of Health Information Technology Regional Extension Centers (RECs) funded under ARRA and HITECH to help doctors adopt EHRs and qualify for incentives.
However, vendors also play a big role in evangelizing and supporting physicians newly adopting EHRs to help them get to meaningful use — including the full use of ePrescribing functionality that works to the benefit of patients and outcomes.
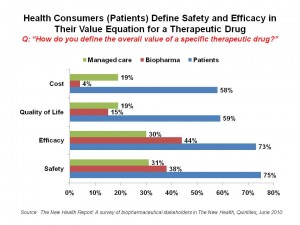 Health Populi’s Hot Points: In that vein, it’s useful to remember consumers’/patients’ perspective on the value of prescription drugs. As the chart shows, most people not only value efficacy (that is, if a drug works effectively) and safety, but what a medication can do to improve her quality of life, and the bottom-line of what the drug costs.
Health Populi’s Hot Points: In that vein, it’s useful to remember consumers’/patients’ perspective on the value of prescription drugs. As the chart shows, most people not only value efficacy (that is, if a drug works effectively) and safety, but what a medication can do to improve her quality of life, and the bottom-line of what the drug costs.
ePrescribing can thus be a link that helps patients better engage with physicians in conversations about prescription drug safety, usefulness, and that elephant in the room: health costs. When doctors can access information about the patient’s drug formulary, they can have an honest conversation about useful alternatives rooted in the real-world of the patient’s out-of-pocket costs. This enhances health engagement and the kind of two-way discussion that can promote medication adherence as well as the basis for growing participatory medicine and connected health.




 Thank you, Jared Johnson, for including me on the list of the
Thank you, Jared Johnson, for including me on the list of the  I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a