 “Value” in prescription drugs is first and foremost about outcomes, in the eyes of physicians and biopharma. For managed care, “value” is first about safety, then patient outcomes.
“Value” in prescription drugs is first and foremost about outcomes, in the eyes of physicians and biopharma. For managed care, “value” is first about safety, then patient outcomes.
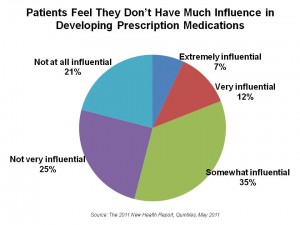
However, although one-third of patients managing a chronic condition cannot define “value” in health care, 9 in 10 say that prescription drugs are “valuable” to their health and wellbeing. In fact, 80% say that the money they spend on prescription medications is “worth it.” Yet patients feel largely out of the prescription drug development process.
These findings come from Quintiles research report, The 2011 New Health Report, subtitled: exploring perceptions of value and collaborative relationships among biopharmaceutical stakeholders.
The Report is based on a survey of executives in biopharmaceuticals (N=200) and managed care (N=153), physicians (N=400), and patients living with chronic conditions, age 18 and up (N=1,000), conducted in January and February 2011.
Physicians are seen by all four stakeholder groups as adding the most value in health care: 46% of patients put doctors first, followed by 23% who say that scientists and medical researchers add the most value. In third place in the patient’s view, patients and patient advocacy groups add the most value. A vast majority of patients (82%) also say that physicians are effective in educating them and understanding their needs, compared with biopharma and managed care. Doctors, in particular, rank managed care relatively low in understanding the needs of patients.
Health Populi’s Hot Points: Following the meeting of the 2011 HIMSS in Orlando in February 2011, I titled my iHealthBeat column wrap-up of the meeting, “Collaborations are the new black” when it came to health information technology. Quintiles asserts the same is true for life science companies, as well, in The 2011 New Health Report.
The key collaborator-partner for biopharma is the patient: patients want to be involved, can handle the truth about risks and clinical trial details, yet feel out of the loop vis-a-vis life science companies.
On one hand, Quintiles quantifies that patients highly value prescription drugs. On the other hand, industry surveys from Harris Interactive and others indicate that consumers place “Big Pharma” fairly low on the list of respected industries compared with supermarkets, hospitals, and even banks which regained favor in 2010.
So biopharma should welcome the participatory health movement — that growing cadre of engaged, empowered patients who inform themselves, work closely with their physicians and other care touchpoints in their personal health ecosystems, and care about the health of other people in their lives. Patients who actively seek information about their conditions have better outcomes, according to two-thirds of physicians interviewed by Quintiles. Thus, biopharma — and especially, the industry’s researchers — are experts on the medical conditions patients manage, and they should expose their research in new ways to patients and caregivers. While biophama’s sales models remain largely unchanged, the industry should develop novel methods to reach patients through their doctors — the most trusted nexus in health care. That’s where most patients get health information, Quintiles’ survey shows.
Patients hold hope for medical research — 85% are optimistic that they will see advancements in medication and treatments. However, two-thirds of patients are pessimistic about fewer people having access to health care — and this would include access to medical treatments.
Importantly, two-thirds of patients say to help discover new medications, they would consider allowing their experience with prescription medications and health data to be included in a global research database — showing a willingness to share private health information.
The opportunity is that patients feel left out of the process of prescription drug development. As life science companies develop ways to reach patients with expert health information and work with patients to co-develop medications in ways that make sense both statistically, clinically and ethically, a trusted relationship can be re-built and re-ignited. That’s the potential for participatory health in pharma. And patients want to participate.




 Thank you FeedSpot for
Thank you FeedSpot for