 There is broad consensus among doctors, patients and health administrators that the current U.S. health system is broken and unsustainable; preventive services is under-utilized and -valued, quality is highly variable from region to region and patient to patient, and costs continue to spiral upward without demonstrating value.
There is broad consensus among doctors, patients and health administrators that the current U.S. health system is broken and unsustainable; preventive services is under-utilized and -valued, quality is highly variable from region to region and patient to patient, and costs continue to spiral upward without demonstrating value.
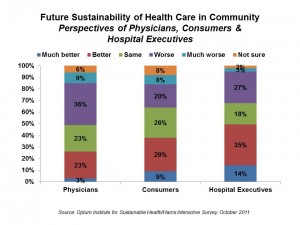
While these 3 segments – physicians, people-patient-consumers, and hospital execs, agree on this topline assessment, what they see about the future of health delivery in America varies, according to a new survey from the new Optum Institute for Sustainable Health, Sustainable health communities: A manifesto for improvement. This is the kick-off of the Optum Institute, a member of the Optum health services business — the reincarnation of Ingenix, part of UnitedHealth Group.
Looking to the future, nearly one-half of community health leaders see health as more sustainable today than five years ago, and expect the next five years to improve. However, physicians disagree: only 22% of doctors said their communities are more sustainable than 5 years ago, and 1 in 4 say this will improve in 5 years. Consumers’ views sit in-between physicians and hospital execs.
On the hopeful side of the ledger, the majority in all three stakeholder groups see opportunities for collaborating together to improve health care quality and reduce costs in their communities.
The Optum Institute categorizes these opportunities across four dimensions:
- Better coordinating health care
- Deploying technology, in particular electronic medical records (EMRs)
- Aligning incentives, such as paying physicians for performance and taking on more financial risk
- Information transparency, especially communicating variation in quality of care in communities, and exposing patients to their health data via EMRs.
The end-game is to achieve the so-called “triple aim” in health care: to improve quality, reduce cost, and engender high satisfaction with the health system.
The survey was conducted by Harris Interactive online in October 2011 among 1,000 U.S. physicians, 2,000 U.S. adults, and 400 U.S. hospital executives.
Health Populi’s Hot Points: It will take the proverbial village to morph the U.S. health system toward an economically sustainable model that brings high value care to health citizens in their local communities. Patients, doctors and hospitals all agree that. The heaviest lifting in getting to that sustainable nirvana will be in the line item Optum points to as “aligning incentives.” In the whack-a-mole game that is health care cost shifting, you can cut costs in one area and they get moved to another segment. The survey showed a gap between what physicians believe can get cut versus what consumers see: 29% of people say that costs could be cut without impacting quality; 14% of physicians think this is possible. The chasm lies in the economic reality of the physician’s practice, where they have been subject to the ongoing changes in Medicare, Medicaid, and commercial insurance reimbursement. The current budget/debt discussions are focused keenly on physician payment, so this issue is top-of-mind for this key stakeholder.
The adoption of electronic health records can help with improving transparency of information and getting patients more engaged in their own health care. This will be one of the ‘costs’ to be borne by patients: to become more involved in their own care, and in the decisions about their care in collaboration with health providers. More engaged patients realize better outcomes. This two-way street of patient engagement is part of meaningful use of EMRs.
Patient engagement also means people taking on more personal responsibility for their health. Aligning incentives will need to be rooted in value-based health benefit designs so that people are ‘nudged’ to adopt healthier behaviors. Beyond the ‘village’ of patients, doctors and hospitals, it will take fellow stakeholders — employers, health plans, schools, communities-at-large — to usher in the new era of sustainability in U.S. health care.




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a