 Chronic illness represents $3 of every $4 of annual health spending in the U.S. That’s about $1.5 trillion.
Chronic illness represents $3 of every $4 of annual health spending in the U.S. That’s about $1.5 trillion.
Living Well With Chronic Illness, a report from The Institute of Medicine (IOM), issues a “call for public health action” to address chronic illness through:
– Adopting evidence-based interventions for disease prevention
– Developing new public policies to promote better living with chronic disease
– Building a comprehensive surveillance system that integrates quality of life measures, and
– Enhancing collaboration among health ecosystem stakeholders: health care, health, and community non-healthcare services.
The IOM recognizes the social determinants that shape peoples’ health status beyond the care delivery system — such as physical/built environments, food systems, and social connections (peers and family).
The report looks at nine “exemplar” health conditions that share common factors — especially influencing public health and economics. These include arthritis, cancer, chronic pain, dementia, depression, type 2 diabetes, posttraumatic disabling conditions, schizophrenia, and vision and hearing loss.
The IOM recommends incorporating cost-effectiveness analysis in policy decisions that take into account the concept of “living well” with chronic conditions. This could manifest, IOM proposes, in a pilot test for “Health in All Policies” for Federal laws.
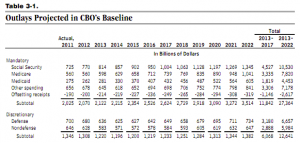
Health Populi’s Hot Points: While the IOM report was going to print, so was another influential report: The Budget and Economic Outlook: Fiscal Years 2012 to 2022 from the Congressional Budget Office (CBO).
This annual report is must-reading for policy wonks, but especially important for those of us focused on solving the long-term deficit challenge in the U.S. Medicare and health costs are the #1 driver for the long-term deficit in America. Thus, focusing on bending the cost-curve on chronic illness in the U.S. would be one prescription (among several) for dealing with the deficit.
In the fine print of the CBO Budget report, you will read CBO’s projections rise “because of increasing expenses generated by the aging of the population and rising costs for health care.” Aging is a demographic given: this is what we in the forecasting business classify as a “certainty.” What is influenceable — a variable — is the rate of increase in health care costs.
Page 3 of the report tells us that the number of people age 65 or older will increase by one-third between 2012 and 2022 – from 14% of the U.S. population to 17%, raising the cost of Medicaid, Medicare and Social Security. This, coupled with the implementation of the Affordable Care Act (health reform) will increase the number of people receiving assistance through Federal health care programs.
Spending on these programs will grow at an annual rate of nearly 7% between 2013 and 2022, outstripping GDP growth…a trend that will continue past 2022, CBO expects.
Getting real, practical and creative about the role of chronic conditions in the U.S. is critical for getting the U.S. economy healthy…and to morphing into a health system that’s built to last.




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for