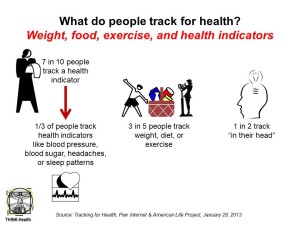
 Most of us keep track of some aspect of our health. Half of all people who track do so “in their heads,” not on paper, Excel spreadsheet, or via digital platform. Furthermore, 36% update their health tracking data at least once a day; but 16% update at most twice a month, and 9% update less than once monthly.
Most of us keep track of some aspect of our health. Half of all people who track do so “in their heads,” not on paper, Excel spreadsheet, or via digital platform. Furthermore, 36% update their health tracking data at least once a day; but 16% update at most twice a month, and 9% update less than once monthly.
Tracking for Health from the Pew Internet & American Life Project paints a portrait of U.S. adults who, on one hand are quantifying themselves but largely aren’t taking advantage of automated and convenient ways of doing so.
Overall, 69% of U.S. adults track a health indicator. The most popular aspects of health to track are weight, diet and exercise. In terms of more medical tracking, one-third of people keep watch on blood pressure, blood sugar, headaches and sleep, as shown in the chart.
These “medical” trackers are more likely to have been diagnosed with a chronic condition, as expected. Moreover, there is a greater likelihood to track as the number of chronic conditions increases beyond a single issue: while 19% of people with no chronic conditions track health, 40% with 1 condition track, and 62% with 2 or more conditions track health indicators. So, too, are people more like to health-track when they’ve experienced a major health change in the past year.
Half of people are tracking ‘in their head,’ and 1/3 are keeping track on paper. 21% of trackers do so digitally, the same proportion as in 2010. Specifically,
- 8% of trackers use a device, such as a digital glucometer for blood sugar or Wi-Fi enabled weight scale. Trackers using digital medical devices that can track tend to be older and diagnosed with 2 or more conditions.
- 7% use a health app via mobile device (phone, tablet)
- 5% use a spreadsheet (THINK: Excel)
- 1% uses a website or online tool.
The survey polled 3,014 U.S. adults over 18 in August and September 2012. The study was supported by the California HealthCare Foundation.
Health Populi’s Hot Points: With three-quarters of health spending in the U.S. allocated to treating chronic health conditions, bending the cost curve will require better managing, and preventing the onset of, noncommunicable diseases: heart disease, diabetes and many cancers, among them. Personally tracking key health measures, such as weight, blood pressure, blood sugar for diabetics and pre-diabetics, and sleep patterns, empowers and engages people in their own health. Knowing your numbers enables people to establish their understand of their baseline health, allowing us to move the needle, one day at a time, toward preventing the onset of illness or the worsening of a diagnosed condition.
People who keep more formal records whether on paper or via technology more regularly update their data vs. 1 in 3 who track “in their head.” Those people tracking on paper or via technologies have realized greater impacts on their health behaviors, especially for people managing chronic conditions.
 “Tracking can affect one’s overall approach to health,” the report concludes, with 63% of health trackers saying that tracking has impacted their health behavior in some way. Nearly one-half of people who health-track find doing so changes their approach to maintaining their own health or health for their loved one. Furthermore, 2 in 5 trackers were motivated to ask a doctor new questions or get a second opinion, and 1 in 3 trackers believe tracking has impacted their decision on how to manage a health condition.
“Tracking can affect one’s overall approach to health,” the report concludes, with 63% of health trackers saying that tracking has impacted their health behavior in some way. Nearly one-half of people who health-track find doing so changes their approach to maintaining their own health or health for their loved one. Furthermore, 2 in 5 trackers were motivated to ask a doctor new questions or get a second opinion, and 1 in 3 trackers believe tracking has impacted their decision on how to manage a health condition.
Formal health-tracking drives people beyond self-health engagement, but motivates the sharing of the data with both clinicians and with other people. 1 in 3 health trackers shares their data with someone else (online and offline) – with older people doing so more than younger people. Among formal trackers who share their data, one-half share with a medical profession, 22% share with a partner/spouse, 11% with another family member, and 8% with a friend.
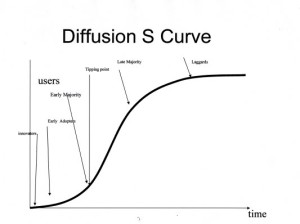
Thus, formal health tracking bolsters social health and personal health engagement, driving health behavior change. We are approaching the inflection point on the diffusion of adopting health tracking in our daily lives; moving from “in our heads” to more formal methods, ultimately to automated processes that don’t require manual entry — will drive further meaningful health engagement. And potentially move our personal health economic cost curves, as well.





 Grateful to Gregg Malkary for inviting me to join his podcast
Grateful to Gregg Malkary for inviting me to join his podcast  This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're
This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're