 This week, I had a conversation with a physician whom I consider quite patient-engaged, who uses an EHR, and who works with one of the most wired health organizations in the United States. I complained to her that my user-generated data from my Bodymedia armband, Fitbit, Withings scale, among other #QuantifiedSelf devices, can’t find their way through the cloud to my doctors’ electronic health records or my patient portal. Her reaction was surprising to me. She was not so keen on the idea, saying, “It’s the physician workflow” that’s the problem.
This week, I had a conversation with a physician whom I consider quite patient-engaged, who uses an EHR, and who works with one of the most wired health organizations in the United States. I complained to her that my user-generated data from my Bodymedia armband, Fitbit, Withings scale, among other #QuantifiedSelf devices, can’t find their way through the cloud to my doctors’ electronic health records or my patient portal. Her reaction was surprising to me. She was not so keen on the idea, saying, “It’s the physician workflow” that’s the problem.
The wordle on workflow comes from Dr. Chuck Webster (@EHRworkflow), one of the unique clinicians who blogs and is passionate about electronic health records and business process re-engineering. Learn more about Dr. Chuck via this great Perficient video from HIMSS 2012.
If you dig into the wordle and play a game of “magnetic poetry” with the words, you can cobble together various takes on workflow. I like the following mash-up: “the process or systems that clinicians use to ensure coordinated patient care.”
In this week’s Information Week, there’s a column that speaks to this issue: Doctors Push Back on Health IT’s Workflow Demands by Michelle McNickle (@m_mcnickle on Twitter). “The process for caring for patients is broken,” McNickle writes. Dr. Simeon Schwartz of Westmed Medical Group in Westchester County, NY, is quoted as saying that with respect to patient involvement, “”you can fix as many pieces as you want, but until you bring those pieces together into a new workflow, that won’t change the patient experience.” He confessed, “We’re [still] not creating the experience they [patients] want.”
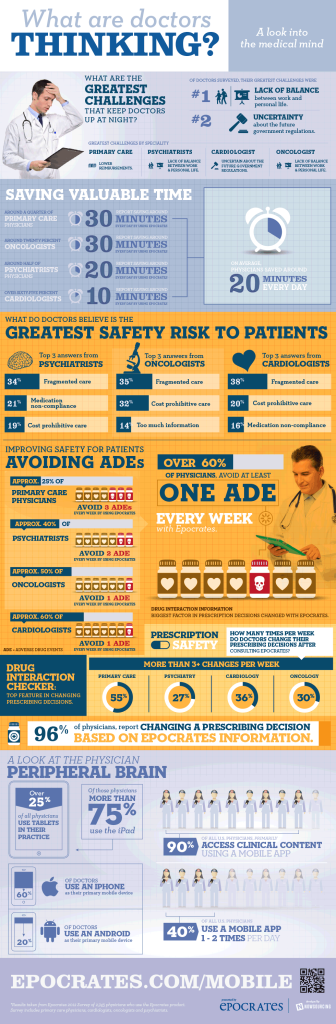 In the meantime, Epocrates polled physicians in late 2012 to learn what’s keeping them up at night. The infographic summarizes the results of the study, with the topline finding that physicians’ lack of balance between work/home life, and uncertainty about government regulations, are most concerning.
In the meantime, Epocrates polled physicians in late 2012 to learn what’s keeping them up at night. The infographic summarizes the results of the study, with the topline finding that physicians’ lack of balance between work/home life, and uncertainty about government regulations, are most concerning.
Epocrates also learned that 90% of physicians access clinical content via a mobile app, and 40% use a mobile app once or twice a day.
Health Populi’s Hot Points: Physicians have quickly adopted mobile platforms like iPhones and iPads because they realize, in real-time and quite immediately, real value from using them (see link to Manhattan Research’s survey). Epocrates captured aspects of physician value perceptions in their survey, shown in the graphic, that using clinical mobile apps bolsters patient safety and saves time: the most precious resource of the busy physician, who wants to recapture work/life balance per the survey.
Accessing my health/wellness activity data, for most physicians, isn’t so valuable to them…yet. Two of my PCPs (my OBGYN and internist) actually want to have my user-generated data populating my health record, but the vendor of their EHR (one of the big iron, closed systems that isn’t based on open-source standards) isn’t worried about that functionality right now.
The HITECH Act’s Meaningful Use, Stage 3, may foster this capability three or four years from now. But that’s one of those pesky government mandates — headache #2 for physicians — that’s a pain point, per the Epocrates study.
I will continue to be a shoemaker’s child with no shoes when it comes to marrying my self-generated health data to my medical information. So much for patient engagement. For now, bless Runkeeper, whose HealthGraph helps me track my activities, my food, and my sleep.
Now that’s what I call meaningful use.




 Thank you, Trey Rawles of @Optum, for including me on
Thank you, Trey Rawles of @Optum, for including me on  I was invited to be a Judge for the upcoming
I was invited to be a Judge for the upcoming  For the past 15 years,
For the past 15 years,