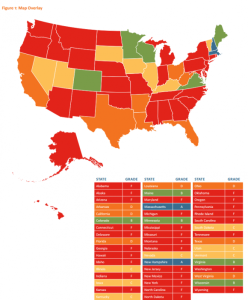
 Only two U.S. states have comprehensive health care price transparency regulations that ensure citizens’ access to clear and open health price information. While those two states, Massachusetts and New Hampshire, earn an “A” in the Report Card on State Price Transparency Laws, an addition five state earn a “B,” with the remainder of the United States garnering a “C” or less. The map illustrates that most states are red states, earning the lowest score of “F.”
Only two U.S. states have comprehensive health care price transparency regulations that ensure citizens’ access to clear and open health price information. While those two states, Massachusetts and New Hampshire, earn an “A” in the Report Card on State Price Transparency Laws, an addition five state earn a “B,” with the remainder of the United States garnering a “C” or less. The map illustrates that most states are red states, earning the lowest score of “F.”
With the growth of high-deductible health plans (under the umbrella of so-called “consumer-directed” plans) where health consumers pay thousands of dollars to meet a spending limit when insurance kicks in to cover health costs, consumers lack access to the kind of information they need to be “rational” economic men and women in the class economic sense.
The Report Card study, published on March 18, 2013, was conducted by the Catalyst for Payment Reform and the Health Care Incentives Improvement Institute (HCI3). The Catalyst is an association of large employers and health plan sponsors who collaborate to advocate for high value health care. HCI3 is a group of payors, providers and other health industry stakeholders who work toward value-based, quality health care.
The two non-profit organizations worked together to evaluate health price transparency laws in all 50 states based on detailed criteria, including by not limited to:
- Providing health pricing information to the state only (10% of the total grade)
- The ability for patients to request pricing information prior to receiving health services (20% of the grade)
- Providing a public report on pricing information (20% of the grade)
- Providing for posting pricing information on a public website (50% of the grade).
Thus, one-half of the state’s grade on price transparency was based on the state’s having laws mandating posting of health prices on a public website, such as paid amounts by insurers and consumers and charges for inpatient and outpatient services by hospitals and providers.
States earning the lowest grade of “F” were those scoring between 0 and 29 based on the grade composition described in the above bullets. These 29 states with low legal provision for price transparency included, in alpha order, Alabama, Alaska, Arizona, Connecticut, Delaware, Georgia, Hawaii, Idaho, Indiana, Kansas, Maryland, Michigan, Mississippi, Missouri, Montana, Nebraska, New Jersey, New Mexico, New York, North Carolina, North Dakota, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, Tennessee, Washington, and Wyoming.
Forbes magazine covered this story well here by Bruce Japsen.
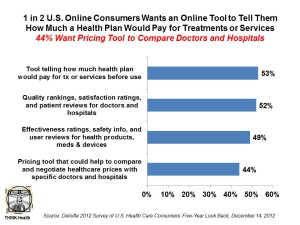 Health Populi’s Hot Points: Most online U.S. consumers would be likely to use a tool that shows what a health plan would pay for treatments or services before they receive them, and 44% of Americans online would welcome a pricing tool to help compare and negotiate health prices for specific doctors and hospitals, and the second chart shows (Source: Deloitte 2012 Survey of U.S. Health Care Consumers). So the consumer demand side for health price and quality transparency information is strong.
Health Populi’s Hot Points: Most online U.S. consumers would be likely to use a tool that shows what a health plan would pay for treatments or services before they receive them, and 44% of Americans online would welcome a pricing tool to help compare and negotiate health prices for specific doctors and hospitals, and the second chart shows (Source: Deloitte 2012 Survey of U.S. Health Care Consumers). So the consumer demand side for health price and quality transparency information is strong.
The phrase “patient engagement” comes to mind, but not in the way it’s often used in terms of pure “health” engagement. Instead, the definition of health engagement must go beyond clinical care engagement to include health financial engagement, as well. U.S. health citizens have been long sheltered from the reality of health prices, with out-of-pocket costs playing the starring role in how most consumers have viewed their costs. However, third party payors and plan sponsors have negotiated these consumer-facing costs, which don’t reflect the real value of the services and products deployed in a patient’s care.
I wrote about patient activation’s potential to lower cost in Health Populi in February 2013, when Health Affairs published a seminal research article by Judith Hibbard et. al., finding that the more engaged a patient is, the lower their costs. Patient engagement is one of the secrets in the sauce to bending the U.S. health care cost curve. But without transparency, this recipe fails.




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for