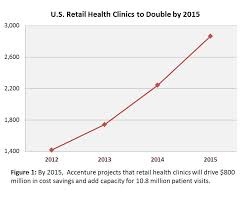
 The number of retail health clinics will double between 2012 and 2015, according to a research brief from Accenture, Retail medical clinics: From Foe to Friend? published in June 2013.
The number of retail health clinics will double between 2012 and 2015, according to a research brief from Accenture, Retail medical clinics: From Foe to Friend? published in June 2013.
What are the driving market forces promoting the growth of retail clinics? Accenture points to a few key factors:
- Hospitals’ need to rationalize use of their emergency departments, which are often over-crowded and incorrectly utilized in cases of less-than-acute care. In addition, hospitals are now financially motivated under the Affordable Care Act (ACA, health reform) to reduce readmissions of patients into beds (particularly Medicare patients with acute myocardial infarction [heart attacks], congestive heart failure, and pneumonia).
- The undersupply of primary care providers (PCPs) – internists, general practitioners, family doctors, and pediatricians – and the need for those in practice to extend services beyond normal hours to serve patients in more convenient times and locations.
- Health plans that want to provide consumer-friendly health services to enrollees, and channel them to cost-effective levels of care to effectively manage costs and health plan premium dollars.
Dr. Kaveh Safavi who leads Accenture’s health practice in North America calls this phenomenon a “release valve” for the U.S. health system.
Health Populi’s Hot Points: Health citizens with a strong primary care backbone, such as those in Europe like Denmark, France, Germany and the United Kingdom, have better health outcomes than patients in the U.S. Retail clinics provide additional “bone structure” for the undersupplied American primary care infrastructure. So “release valve” as coined by Accenture is an apropos metaphor.
But does a release valve guarantee continuity of care or a way to fill an immediate need in a convenient, lower-cost package? It’s the latter, which isn’t a bad thing: it’s just not necessarily an optimal solution.
Don’t get me wrong here: I’m a fan of growing retail, convenient, lower-cost high quality health formats in the community where people live, work, play and pray. What would make my evaluation more positive is seeing the opportunities Accenture hints at come to fruition with the patient encounters getting captured into a continuity of care record. In so doing the person’s health visit gets recorded into a health information system where a medical home, regular care coach, or PCP can track the patient’s full health picture over time.
Adding more fragmentation to an already-episodic health system won’t solve the cost-and quality- problems of the U.S. health system. But if retail health clinics can become integral partners in accountable and value-based care ecosystems in local communities, bring on the Welcome Wagon for these part-time medical homes.




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for