 When certain people use certain dietary supplements, they can save money, according to a report from the Council for Responsible Nutrition and Frost and Sullivan, the analysts. The report is aptly titled, Smart Prevention – Health Care Cost Savings Resulting from the Targeted Use of Dietary Supplements. Its subtitle emphasizes the role of dietary supplements as a way to “combat unsustainable health care cost growth in the United States.”
When certain people use certain dietary supplements, they can save money, according to a report from the Council for Responsible Nutrition and Frost and Sullivan, the analysts. The report is aptly titled, Smart Prevention – Health Care Cost Savings Resulting from the Targeted Use of Dietary Supplements. Its subtitle emphasizes the role of dietary supplements as a way to “combat unsustainable health care cost growth in the United States.”
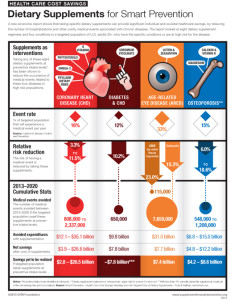
Specifically, the use of eight supplements in targeted individuals who can most benefit from them can save individuals and health systems billions of dollars. The eight money-saving supplements are:
> Omega-3
> B Vitamins
> Phytosterols
> Psyllium Dietary Fiber
> Chromium Picolinate
> Lutein and Zeaxanthin
> Calcium and Vitamin D
> Magnesium.
The researchers reviewed the scientific literature covering these eight regimens across several conditions:
- Coronary heart disease (CHD)
- High cholesterol (LDL) and CHD
- Diabetes-attributed CHD
- Age-related eye disease
- Osteoporosis.
These conditions are largely thought to be non-communicable diseases, amenable to lifestyle changes…such as taking dietary supplements.
Health Populi’s Hot Points: CHD is the most costly disease in the U.S., so it’s useful to consider strategies that can lower the economic and social costs of the condition. The study estimated that if men and women 55 and over who had high-cholesterol took psyllium dietary fiber daily, the cost savings for CHD would be $2.5 bn per year. If women over 55 with osteoporosis took calcium and vitamin D daily, there would be a $1.5 bn savings each year.
The big picture is that non-communicable diseases are what’s killing the planet — not TB or AIDS or other infectious diseases. And, NCDs can be prevented or reversed by making lifestyle changes having very little to do with the doctor — except, if the doctor would recommend these kinds of dietary supplement strategies more often, we could drive better health behavior, prevention, and lower costs. That’s a form of value-based care that often gets overlooked as it doesn’t involve health system assets like rationalizing MRI utilization, preventing hospital readmissions, or pharmacy supply chain management. These are all very useful institutional cost-management strategies, but getting to patients and driving self-care outside of the doctor’s office and institutional setting are also part of accountable and value-based care.




 Thank you FeedSpot for
Thank you FeedSpot for