 Self-service – people DIYing health care — can help solve the primary care shortage in America, based on the findings of 23 studies published this week.
Self-service – people DIYing health care — can help solve the primary care shortage in America, based on the findings of 23 studies published this week.
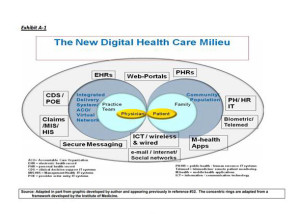
If health information technologies (health IT) were “fully implemented” in 30% of doctors’ offices, demand for physicians would fall by 4 to 9%, according to The Impact of Health Information Technology and e-Health On the Future Demand for Physician Services, published in the November 2013 issue of Health Affairs. Weiner, Yeh and Blumenthal did a meta-analysis of the literature on health IT and its potential to improve productivity and extend physician services and found that using HIT can help salve shortages in physician markets. The authors discuss “the new digital practice milieu,” where 82% of office-based physicians in the U.S. now have an EHR. However, fewer than 35% of physicians are using a comprehensive HIT system, so that “full use” and potential benefits of these tools are elusive.
At the same time, health consumers in the U.S. want to use e-health tools – such as emailing doctors and looking into their personal health records such as lab test results.
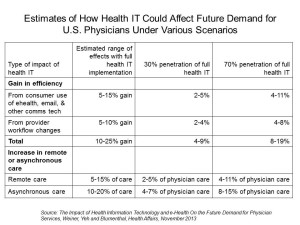 While the authors believe that “the likelihood of that health IT adoption will not progress at all beyond its present status….is nil,” the forecast for providers’ universal full-on embrace of EHR functionality is hazy. One of the key issues to keep in mind when forecasting deep use of EHRs and health IT include is how the use of Big Data and analytics will impact medicine – something of a wild card for the next 5-10 years. What’s past won’t be prologue, the researchers predict.
While the authors believe that “the likelihood of that health IT adoption will not progress at all beyond its present status….is nil,” the forecast for providers’ universal full-on embrace of EHR functionality is hazy. One of the key issues to keep in mind when forecasting deep use of EHRs and health IT include is how the use of Big Data and analytics will impact medicine – something of a wild card for the next 5-10 years. What’s past won’t be prologue, the researchers predict.
Clinical Management Apps: Creating Partnerships Between Providers and Patients, from The Commonwealth Fund, posits that apps can help to transform health care delivery across all populations – even hard-to-reach lower-income people who often fall through both the health care safety net and digital divide.
Silow-Carroll and Smith look into the 40-60,000 health and wellness apps in the market, and believe that these may be beneficial for low-income and minority patients disproportionately affected by chronic disease. Because these people often face barriers to accessing health care, self-managed apps – when adopted and used – can address this challenge. The researchers point to data from the Pew Internet & American Life Project which shows that African Americans and Hispanics are more likely than white people to own a smartphone and among cell phone owners, minorities are also more likely to use their phones for accessing health information.
A Harris poll found that at least one-third of people who participate in online activities are keen to use smartphones or tablets to “do” health online: ask doctors questions, make appointments, and receive medical test results, for example. Among the many clinical management apps discussed are dermatology, diabetes, asthma, and general medication reminders.
Before we get too techno-optimist about this scenario, there are drawbacks and barriers to consider in the form of reimbursement, technical, regulatory, personal and financial challenges. The FDA Guidance issued in September 2013, before this paper got approved for publication, will help solve some of the regulatory vagueness that slowed developers in this space. Regarding the financial barrier, some enlightened Medicaid plans have provided smartphones to enrollees to encourage the use of health apps and streamlined communication with health providers.
Health Populi’s Hot Points: “Human-machine interactions may change so dramatically that people can no longer be neatly divided into categories such as patient, clinician, and support staff,” Weiner and team foresee.
The bottom line is that the consumer-patient will be playing an increasing self-service role in her health care. “Patient-centered provider teams will need to take advantage of data that are generated before, during and after a visit (whether face-to-face or remote) and that come from numerous nontraditional, community-based sources,” Weiner and his team write.
While the promise of self-service primary care, bolstered in these two publications, is positive, there are supply side and demand side issues to keep in mind. The Commonwealth Fund points out that apps can be targeted to lower-income people who bear a large burden of chronic disease. However, without adequate financial incentives to engage, and well designed programs that delight consumers. adoption and sustained use will be in peril. The Health Affairs article reminds us that provider workflow when it comes to full engagement of health IT is also more a cultural than technical challenge and while Meaningful Use incentives have inspired initial adoption, it remains to be seen how intimately doctors and providers will hug these tools.




 Thank you FeedSpot for
Thank you FeedSpot for