 This is my second post for the #HIMSS14 Blog Carnival, written to coincide with the annual 2014 HIMSS Conference convening health IT leaders in Orlando, FL, 23-28 February 2014. I am gratified to be one of a dozen+ Social Media Ambassadors to the Conference. The first post, on why health IT ‘should’ matter to consumers, can be found here.
This is my second post for the #HIMSS14 Blog Carnival, written to coincide with the annual 2014 HIMSS Conference convening health IT leaders in Orlando, FL, 23-28 February 2014. I am gratified to be one of a dozen+ Social Media Ambassadors to the Conference. The first post, on why health IT ‘should’ matter to consumers, can be found here.
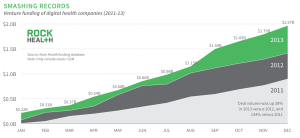
Investments in the digital health space reached nearly $2 billion in 2013, based on Rock Health’s look back at venture funding in the market. These financings covered $245 mm that went toward electronic health records and clinical workflow; $161 toward analytics and Big Data in health care’ $146 mm for digital medical devices; $136 mm for wearables and biosensing; $126 mm to population health management; and, $119 mm for health care consumer engagement. This venture funding is over-and-above the investments that incumbent companies already involved in health IT are making for new product development and innovations.
At the same time, more people, patients and caregivers are spending disposable income on self-tracking devices, health information access, digital medical devices such as USB-enabled blood pressure monitors and glucometers for managing health and conditions outside of the health system, at home.
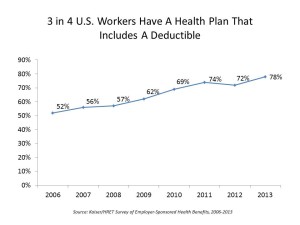 Employers, increasingly moving toward consumer-directed health plans — largely, high-deductible health plans — are bundling wellness programs into health insurance programs, many of which are nudging consumers via carrots (and more and more, sticks) to adopt healthy lifestyles to move personal needles on health metrics like BMI, blood pressure, and physical activity.
Employers, increasingly moving toward consumer-directed health plans — largely, high-deductible health plans — are bundling wellness programs into health insurance programs, many of which are nudging consumers via carrots (and more and more, sticks) to adopt healthy lifestyles to move personal needles on health metrics like BMI, blood pressure, and physical activity.
Prescription drug companies, long in the bulls-eye of health system critics, are getting closer to patients surrounding their products with services to help people stay on-track with adhering to therapeutic regimens (dosing regularly and on-time).
Hospitals, facing dis-incentives for re-admitting patients into hospitals for AMI, CHF and pneumonia, are getting better at predicting which discharged patients are at-risk for returning to the ER and inpatient bed, by linking with people through remote health monitoring and proactively calling patients to help them keep well and safe at home.
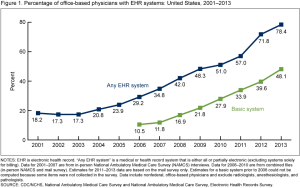 And physicians continue to deepen their adoption of electronic health records, moving toward meaningful use (and the eventual garnering of hard-dollar incentives).
And physicians continue to deepen their adoption of electronic health records, moving toward meaningful use (and the eventual garnering of hard-dollar incentives).
Health care delivery and financing in the U.S. is, slowly, slowly, morphing toward a more harmonious ecosystem as payment, incentives, and access designs reduce friction across silos. Health IT and communications technologies support this migration by promoting data standards, interoperability, and ultimately, data liquidity.
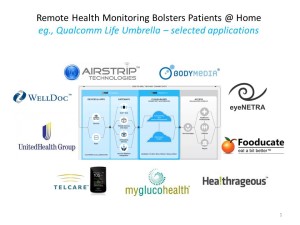 An example of how this has begun to happen is via Qualcomm Life’s 2net platform, an example of which is shown in the fourth exhibit. Imagine the complex workflow for a person managing diabetes on a daily basis: checking and tracking blood glucose, creating healthy grocery shopping lists, monitoring heart function, tracking physical activity, ensuring eye health, adjusting medications and timing of doses, and other tasks.
An example of how this has begun to happen is via Qualcomm Life’s 2net platform, an example of which is shown in the fourth exhibit. Imagine the complex workflow for a person managing diabetes on a daily basis: checking and tracking blood glucose, creating healthy grocery shopping lists, monitoring heart function, tracking physical activity, ensuring eye health, adjusting medications and timing of doses, and other tasks.
The Qualcomm 2net platform enables the bits of personal health data to move and populate peoples’ personal health records. The last mile will be ensuring that peoples’ Observations of Daily Living can inter-operate with more traditional forms of health data – the physician’s (or more likely physicians’) EHRs, hospital systems, and ultimately with peoples’ smart front-end systems that help them “read” themselves and make good health and life decisions when they want and need to. This enables people to become their own and best primary care providers.
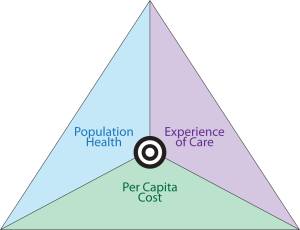 This takes a village — of providers, payers, plan sponsors (employers, unions, governments), pharma, device companies, pharmacy, and people. The full value of health IT is realized when all parties come to the table to ensure data liquidity and ultimately, information and support flowing to people and patients. More value can be derived when technologies don’t add costs, but conserve costs and resources. This will mean replacing those mature technologies that don’t deliver on the present-day value proposition — but continuing to use mature tools that do deliver. The goal: driving The Triple Aim of reducing costs, expanding access, and enhancing the patient experience.
This takes a village — of providers, payers, plan sponsors (employers, unions, governments), pharma, device companies, pharmacy, and people. The full value of health IT is realized when all parties come to the table to ensure data liquidity and ultimately, information and support flowing to people and patients. More value can be derived when technologies don’t add costs, but conserve costs and resources. This will mean replacing those mature technologies that don’t deliver on the present-day value proposition — but continuing to use mature tools that do deliver. The goal: driving The Triple Aim of reducing costs, expanding access, and enhancing the patient experience.




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for