Three U.S. health plans cover about 100 million people. Today, those three market-dominant health plans — Aetna, Humana and UnitedHealthcare — announced that they will post health care prices on a website in early 2015. Could this be the tipping point for health care transparency so long overdue?
These 3 plans are ranked #1, #4 and #5 in terms of market shares in U.S. health insurance. Together, they will share price data with the Health Care Cost Institute (HCCI), a not-for-profit organization dedicated to research on U.S. health spending. An important part of the backstory is that the HCCI was launched by the three health plans participating in this project along with Kaiser Permanente in 2011.
According to some reports, WellPoint and CIGNA (#7 and #2 market-share wise) declined to participate in the project for at least this launch phase.For
Here’s the official press release about the project. For consumers, the statement says, “this will provide consistent and accurate transparency in the shopping experience with the most comprehensive cost data and quality information; uninsured individuals can access more reliable information about the relative prices of care, treatments and procedures.”
Health Populi’s Hot Points: The Healthcare Financial Management Association has said that “Health plans are in the best position to help their members find out the total estimated price of the service,” according to the Transparency Task Force’s report detailed in Part 1 of this topic here on Health Populi.
 Until quite recently, health insurance companies have considered price data to be a closely-held asset, proprietary information kept close-to-the-corporate vest. More health insurance companies have built cost-calculators for plan members, like Aetna’s Member Payment Estimator and CIGNA’s Cost of Care Estimator. The HCCI project promises to provide more data points in a more visible format from the 3 for-profit health plan founders who are, voluntarily, “going public” with a not-for-profit entity.
Until quite recently, health insurance companies have considered price data to be a closely-held asset, proprietary information kept close-to-the-corporate vest. More health insurance companies have built cost-calculators for plan members, like Aetna’s Member Payment Estimator and CIGNA’s Cost of Care Estimator. The HCCI project promises to provide more data points in a more visible format from the 3 for-profit health plan founders who are, voluntarily, “going public” with a not-for-profit entity.
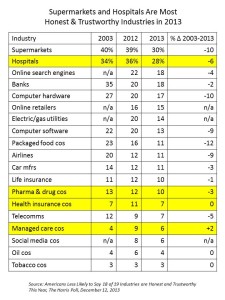
This point is very important: health plans aren’t universally trusted by health consumers – they’re on the lower end of the corporate trust roster, as the table illustrates, more closely aligned to Big Oil, Big Food and Big Tobacco than supermarkets and hospitals, according to a 2013 Harris Poll.
The Robert Wood Johnson Foundation observed in their 2012 report, Counting Change: Measuring Health Care Prices, Costs and Spending, that “insurance has a ‘distorting effect’ on measuring cost…because many health care prices are determined not by what it costs to produce them, but rather by what insurers will pay.”
Now that consumers with high-deductible health plans must cover health costs from the first dollar (until meeting that deductible), we can substitute “what consumers will pay” at the end of RWJF’s sentence from the report “Counting Change.” This is exactly what the newly-evolving health consumer has begun to do – count dollars and pennies toward meeting that deductible, whether enrolled in that health plan through his employer or her Health Insurance Exchange under the Affordable Care Act. Aetna, Humana and UHC are, finally, doing what’s been needed to be done since the advent of consumer-directed health plans in the late 1990s.
It’s a long time coming, and a welcome development.
Part 4 of Health Populi‘s week on the Season of Healthcare Transparency will look into consumer payments and useful tools that are arming people to evolve into health care consumerism.




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for