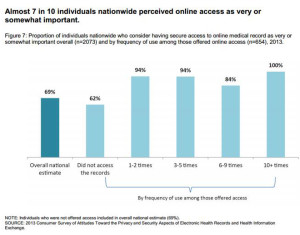
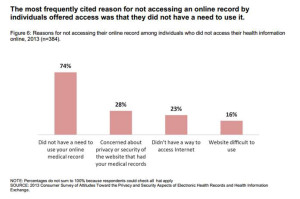
There’s a health information disconnect among U.S. adults: most people believe online access to their personal health information is important, but three-quarters of people who were offered access to their health data and didn’t do so didn’t perceive the need to. The first two graphs illustrate each of these points.
When people do access their online health records, they use their information for a variety of reasons, including monitoring their health (73%), sharing their information with family or care providers (44%), or downloading the data to a mobile device or computer (39%).
In this context, note that 1 in 3 people say they have experienced at least one gap in health information access, including repeating their medical history to a care provider who couldn’t access records from another clinician, hand-carrying a test result or digital image to an appointment, or waiting for test results longer than thought reasonable.
The Office of the National Coordinator for Health Information Technology (ONC) surveyed over 2,100 U.S. adults in 2013 to gauge consumers’ interests and needs for online health information. Dr. Karen DeSalvo, who leads ONC, discussed the results of this study this morning to kick off National Health IT Week and today’s Consumer Health IT Summit.
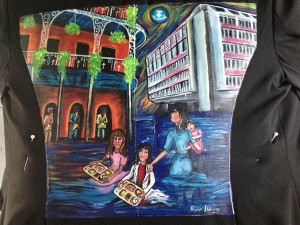 Dr. DeSalvo’s remarks were both professional and personal, concluding her introduction to #NHITWeek with a personal backstory graphically illustrated by Regina Holliday‘s jacket titled Legacy of a Free Lunch (image shown). Dr. DeSalvo joins the growing ranks of The Walking Gallery (of which I am a member, as well – with my “See Jane Think” jacket inspired by my father’s advance directives debacle).
Dr. DeSalvo’s remarks were both professional and personal, concluding her introduction to #NHITWeek with a personal backstory graphically illustrated by Regina Holliday‘s jacket titled Legacy of a Free Lunch (image shown). Dr. DeSalvo joins the growing ranks of The Walking Gallery (of which I am a member, as well – with my “See Jane Think” jacket inspired by my father’s advance directives debacle).
Dr. DeSalvo first talked about the importance of consumers’ accessing health information both from their electronic health records “inside” of health care, and also weaving in data from their own perspectives: from personally generated data, genomics, and “Fitbit data,” Dr. DeSalvo coined. (I assume here that “Fitbit” here is used as a shorthand proxy for digital activity tracking in general).
Dr. DeSalvo and her ONC team are working toward the goal that the Blue Button campaign will inspire people to demand their health data.
As important, Dr. DeSalvo shared her own story as a doctor who, “against many odds,” came out of poverty and benefited from, as Regina and Dr. DeSalvo themed, “free lunches” in terms of services that bolstered Dr. DeSalvo’s access to education, nutrition and health services. She spoke of people who can feel voiceless in society, recognizing that some of the people who need the most help sometimes are the least likely to be able to access that help.
Dr. DeSalvo sees that advancing the digitization of health and health care experience content can “empower and democratize” American health citizens in a way we’ve never been able to do before in the age of paper-based records, and as a result, advancing health equity.
Following Dr. DeSalvo, Emily Kramer-Golinkoff, Founder of Emily’s Entourage, spoke about her journey from patient to patient advocate. Kramer-Golinkoff manages Cystic Fibrosis (CF) along with CF-related diabetes. “The funny thing about patient advocacy, it wasn’t anything I ever aspired to,” Kramer-Golinkoff admitted. “Illness is powerful, all encompassing, and has a mind of its own.”
Kramer-Golinkoff spoke about the countless tasks she must do every single day to manage her conditions. On a good day, she says, she has 37% lung function, takes many injections, and is frequently admitted to hospital for long inpatient stays for courses of antibiotics. CF is intrinsically entwined through her life in every breath, she describes.
By most standards, Kramer-Golinkoff believes, she’s not an “average patient,” but not every patient wants or needs to play the kind of role she does.
“Patient empowerment is living breathing evolving thing,” she observes. The key is recognizing that the player with the most at-stake with the most responsibility for daily management of health are the patients, the hub of their own health care. They are the generators of data and trackers of trends. “We are the reporters on the front lines” for the rest of the care team, Kramer-Golinkoff asserts.
“IT people call it health tracking. We patients call it survival.”
Health Populi’s Hot Points: Kramer-Golinkoff detailed her personal health tracking data line items: these everyday details include the color of her sputum, frequency of coughing spasms, the nature of her breath when she reaches the top of a staircase, the quality of her sleep, her blood sugar readings and insulin use. Sometimes she tracks using digital means (like the aforementioned Fitbit), and sometimes, Kramer-Golinkoff admits, she just tracks in her head — a very common approach, according to the Pew Research Project’s survey on health self-tracking.
The key point made is that these observations of daily living, from sputum color to breaths-at-the-top-of-the-stairs, aren’t found in a patient’s electronic health record. These observations of daily living (ODLs) are person-generated every day in the course of living at home, at work, at school, on the playground. And these data points can add up to “remarkable insights” about when to sound an alarm, Kramer-Golinkoff advised.
These details are particularly important when the stakes are so high, as in her case with CF compromising lung function which is very sensitive to clinical nuances, Kramer-Golinkoff explained.
The vast majority of health care occurs outside of the hospital walls, not just in personally generated data via Fitbits and recorded in Excel spreadsheets, but in social media conversations on Twitter, Facebook, and in Google Hangouts, and Kramer-Golinkoff knows that “Most will never make their way into the EHR.”
She posed two crucial question concluding her insightful talk: how do we integrate all the health care conversations into a larger, richer constructive dialogue for all stakeholders? And, how do we learn from these conversations to advance medicine to make health care better for everyone? Considering these challenges will take us from “Meaningful Use” as a tick-box on the road of health providers receiving financial incentives for implementing digital health records to driving patient care, shared decision making, empowered people, and the democratization of health that Dr. DeSalvo envisions.
For more on Emily’s Entourage, see this video




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for