 While the medical profession has reached a so-called state of crisis, there’s also a “changing of the guard” happening in the profession where doctors are re-imagining what it means to be physician in the era of value-based, technology-enabled health care.
While the medical profession has reached a so-called state of crisis, there’s also a “changing of the guard” happening in the profession where doctors are re-imagining what it means to be physician in the era of value-based, technology-enabled health care.
Such is the state of the union — or dis-union — of the U.S. medical profession.
The 2014 Survey of America’s Physicians from Physicians Foundation finds that 4 in 5 U.S. doctors are over-extended or reaching full capacity in their practices. This is up from 2012. Only 19% of doctors say they have time to see more patients.
That may be because a plurality of doctors (44%) are planning to retire, go part-time, or migrate to non-clinical jobs, which will further reduce patients’ access to physician visits. Such reductions have already begun, with fewer doctors accepting Medicare and Medicaid assignment.
Only 1 in 3 physicians consider themselves independent practice providers, down from 49% in 2012 and 62% in 2008. This signifies that 2 in 3 doctors are employed or members of a corporate practice entity. 53% of physicians call themselves hospital or medical group employees.
2 in 3 physicians see their clinical autonomy is limited and their personal clinical decisions are compromised. At the same time, physicians spend 20% of their time on non-clinical paperwork. 72% of doctors say more physicians should be trained to extend physician supply due to a perceived shortage.
The Foundation emailed a 36-question survey to about 650,000 physician addresses, yielding 20,088 responses (= 3.1% response rate), in March-June 2014. This represents one of the largest physician surveys ever done in the U.S. 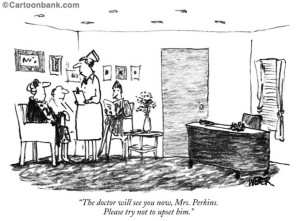
Health Populi’s Hot Points: The Physicians Foundation uses the tagline, “Empowering Physicians. Improving Healthcare.” It is crystal clear based on the results of the 2014 survey that physicians feel far from empowered.
So how does the U.S. “improve healthcare” under these circumstances, with a stressed-out, stretched-out, dis-empowered front line of care providers?
Underneath these numbers, there are stark differences: younger doctors, female doctors, employed physicians, and primary care physicians are relatively more positive about “where” the medical profession is compared with older, male, specialty, and practice owning physicians. This implies that expectations for younger physicians (which includes a greater proportion of female doctors than the older cohort has) are changing.
These younger practitioners already work with information technology and have a different perspective on engaging patients with the technology — which has been more frequently adopted by younger physicians 45 years of age and younger vs those over 45 (92% vs. 81%). Furthermore, more younger physicians say an EMR has improved quality of care than older physician say – at a rate of 42% vs. 26%. Fewer younger physicians are concerned about the privacy implications of EMRs than older physicians at a rate of 36% vs. 58%.
The data point most fascinating to me in this era of growing consumer expectations of a retail experience from health care is that 79% of physicians, overall, say that patient relationships are the most satisfying factor of practicing medicine. This was ranked above financial rewards, noted by only 15% of doctors. “Perhaps the primary reason why many physicians continue to exhibit low morale is the erosion of the physician/patient relationship,” the Foundation observes in its report.
It is time to hug our doctors. Better yet, let’s promote and support meaningful conversations between patients and physicians, which should be a success ingredient in the emerging value-based and high-deductible health care environment. Patients need to better understand effective self-care strategies along with the cost/quality/value aspects of their care. Physicians need to ensure patients engage in effective self-care and pay their share of health charges so practices can remain financial viable.
Hugging goes both ways…




 Thank you FeedSpot for
Thank you FeedSpot for