 Reluctantly accepting the Affordable Care Act, health executives and their architects now see opportunities for re-imagining the hospital and health care services, according to Healthcare Industry Trends, a publication that’s part of the 2015 Building & Development Leadership Series provided by Mortenson, a construction services firm that’s active with healthcare organizations.
Reluctantly accepting the Affordable Care Act, health executives and their architects now see opportunities for re-imagining the hospital and health care services, according to Healthcare Industry Trends, a publication that’s part of the 2015 Building & Development Leadership Series provided by Mortenson, a construction services firm that’s active with healthcare organizations.
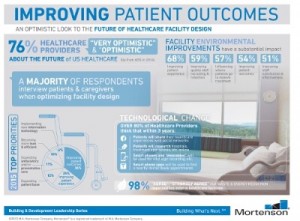
Mortenson conducted a survey at the 2015 ASHE Planning, Design, and Construction Summit, the results of which were published in this report. The over 300 respondents included healthcare executives, facilities managers, and healthcare architects. Thus the lens on the data in this survey is through the eyes of physical healthcare facilities and the people who manage them.
Their over-arching priority is the patient; look at the lower left corner of the infographic, which details the study data. 61% of this pie chart is devoted to (1) improving patient outcomes (36%) and improving the patient experience (25%). Another 12% looks to expanding the patient base, and 11% expanding ambulatory and/or preventive care.
Patients will play a growing role in “Yelping” health, with over 80% of the respondents saying that patients will share their healthcare experiences with social networks within 3 years, research hospitals and treatments online, use smartphones and wearable tech for vital sign tracking, and use apps to find doctors and book appointments. [Rock Health’s digital health consumer survey out last week found that 71% of consumers already seek health information online, consistent with Pew Research Group’s findings].
This is a healthcare-optimistic crowd, in that 76% of them are positive about the future of U.S. healthcare – up from 60% in 2014.
Given that the survey was done with an eye on facilities, it’s important to see that 68% of respondents said facility and environmental improvements have a substantial impact on improving the patient experience; 59% improving quality staff recruiting and retention; 57% influencing where patients go to receive treatment; and, 54% improving patient outcomes.
Another positive finding: most respondents interview patients and caregivers to optimize facility design.
Health Populi’s Hot Points: The survey also asked about the impact of the Affordable Care Act on facility issues. Some key comments illustrate the facility-opportunity of the ACA, like “We see potential in community-based population health initiatives,” and, “We have an opportunity to extend our services to community-type hospitals and to expand outpatient care.”
To that end, architects said, “Facilities should be more hospital-based and less institutional based….Spaces need to be on a more human scale….We need to make sure facilities are conveniently connected or located, easy to navigate, and put patients and visitors at ease.”
Improve facilities, improve outcomes, the Mortenson paper asserts.
Here’s another data point that gets to improving facilities: moving them into different locations via virtual doctor visits, which 63% believe will become “common” practice 3 years from now (call it 2018).
These survey respondents may well be forecasting, or at least intuiting, the impact of Medicare moving to value-based payments in 2018 to the tune of 50% shifting in that direction. That’s no so far away that physical facilities, and of course clinicians and staff, will need to wear value-based payment hats and cater more to patients as consumers who increasingly pay first-dollar coverage, and public payors shifting to paying for performance – outcomes and patient satisfaction.
“We’re finally getting our act together by integrating patients into their own healthcare by stressing health and wellness side-by-side with their very real responsibility in disease management,” one respondent said.
That means care – where we live, work, play, pray and learn. The architects and facilities planners have their work cut out for them – increasingly moving care outside of the institutional setting on Pill Hill or University City, and into communities and peoples’ homes.




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for