There’s an overall feeling of angst about healthcare in America among both health care consumers and the people who provide care — physicians and administrators. On one thing most healthcare consumers and providers (can agree: that the U.S. health care system is on the wrong track.
Another area of commonality between consumers and providers regards privacy and security of health information: while healthcare providers will continue to increase investments in digital health tools and electronic health records systems, both providers and consumers are concerned about the security of personal health information.
In How We View Healthcare in America: Consumer and Provider Perspectives, 2015, Booz Allen Hamilton and Ipsos Public Affairs profile the perspectives of both users and suppliers of health care in the U.S., including the use of technology, access to care, and the role of prevention for individual and public health.
For the 2015 survey, Ipsos polled 1,003 U.S. adults online, and 401 providers (301 physicians including PCPs, specialists, and hospital-based; and 100 health and hospital administrators). While both consumers and providers were studied in this report, this post will focus mostly on the consumer lens.
Most Americans are satisfied with “their” health care overall, although some aspects of satisfaction have fallen since 2014:
- Peoples’ ability to see their personal doctor has fallen from 86% satisfied in 2014 to 81% in 2015
- Peoples’ wait time to get an appointment has fallen from 68% satisfied in 2014 to 63% in 201
- The amount of paperwork needed to be reimbursed for healthcare expenses fell from 61% satisfied in 2014 to 57% in 2015.
People most satisfied with their health care are covered by Medicare. Those with coverage least satisfied? People covered by health plans purchased in Health Insurance Marketplaces, and the uninsured.
When it comes to the expanding use of technology in health care — specifically EHRs — 53% of consumers trust that their personal health data are secure; 46% believe that data collected through doctor-recommended mobile or internet applications are secure. Younger people are more welcoming of new tech in health care than older people. The survey’s new question about doctors sharing personal health information to better coordinate and manage care found a majority of people welcoming that sharing for the benefit of care coordination.
Ironically, and concerning to Health Populi’s support for consumer-clinician shared decision-making, there was a drop in the proportion of consumers engaging in the process: 72% of consumers in 2014 said their providers works with them to choose a course of care that suits their personal needs; this dropped to 62% in 2015.
There’s also a generation gap when it comes to personal responsibility for consumer’s health: older people see greater value in health care providers’ approaches such as aggressive screening for disease and increased care coordination. Younger people value these approaches, but more also see the value in making personal choices for activities that contribute to health on a daily basis such as using mobile technology to monitor health.
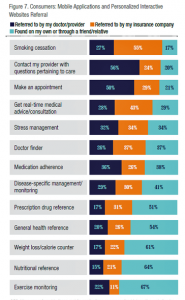 On the technology front, 79% of consumers polled have a smartphone, and 29% of these people use a mobile app or personalized website to monitor or manage health. Most of this activity is for exercise monitoring, health reference, and nutrition/weight loss tools. Older people use digital health technologies more often to access prescription drug references versus other age groups.
On the technology front, 79% of consumers polled have a smartphone, and 29% of these people use a mobile app or personalized website to monitor or manage health. Most of this activity is for exercise monitoring, health reference, and nutrition/weight loss tools. Older people use digital health technologies more often to access prescription drug references versus other age groups.
The second chart details self-directed use of mobile and personalized technologies (in the light blue bar segments) versus tools referred by clinicians (navy blue) and insurance companies (orange). The most common digital tools consumers self-adopt (by finding themselves or via peers) relate to exercise monitoring, nutrition, weight loss and calorie counting, general health reference, and prescription drug information. Most doctors refer patients to mobile apps for care questions and making appointments – call these personal health care administrative tasks like checking claims status, health savings account balances, and paying bills online. Insurance companies tend to refer consumers to tools for smoking cessation, real-time medical advice, doctor finders, and stress management.
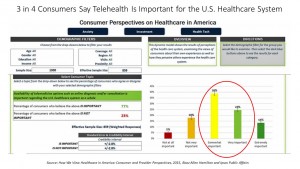 Health Populi’s Hot Points: Consumers continue to seek health care experiences rooted in their 21st century life-flows; that’s why Booz/Ipsos found that 3 in 4 consumers say telehealth is important for American health care, shown in the third chart which was screen-shot from the study’s interactive website.
Health Populi’s Hot Points: Consumers continue to seek health care experiences rooted in their 21st century life-flows; that’s why Booz/Ipsos found that 3 in 4 consumers say telehealth is important for American health care, shown in the third chart which was screen-shot from the study’s interactive website.
In addition, the cost of out-of-pocket medical expenses, coverage of medications, administrative paperwork, and the security of personal health information remain top priorities for health care consumers, as well.
Physicians continue to seek greater autonomy in the practice of medicine, and maintaining a sound business; administrators look to satisfying both providers and consumers, but also look for innovative ways to reduce costs so that they, too, can stay viable financially and relevant to these community-stakeholders.
Bolstering primary care will go a long way to accomplishing all 3 stakeholders’ goals. Every developed country with better public health outcomes than America’s have strong primary care backbones and universal consumer access to that PCP on-ramps. The good news for both consumers, providers and administrators alike is that those on-ramps can be mobile and virtual, and not wedded 24×7 to brick-and-mortar, face-to-face visits with clinicians. Consumers like the idea of telehealth platforms, which can be both synchronous and asynchronous, and cost the system and consumers out-of-pocket less money — as well as preserving precious PCP resources needed for in-person care when hands-on consultation is needed between patient and provider. See my joint research conducted with Accenture on the opportunity for virtual visits to extend the U.S. primary care infrastructure.




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a