 Older workers and retirees in the U.S. are most pleased with their healthcare experiences and have the fewest problems accessing services and benefits. But, “younger workers [are] least comfortable navigating U.S. healthcare system,” which is the title of a press release summarizing results of a survey conducted among 1,536 U.S. adults by the Harris Poll for Accolade in September 2015. Results of this Accolade Consumer Healthcare Experience Index poll were published on April 12, 2016.
Older workers and retirees in the U.S. are most pleased with their healthcare experiences and have the fewest problems accessing services and benefits. But, “younger workers [are] least comfortable navigating U.S. healthcare system,” which is the title of a press release summarizing results of a survey conducted among 1,536 U.S. adults by the Harris Poll for Accolade in September 2015. Results of this Accolade Consumer Healthcare Experience Index poll were published on April 12, 2016.
Accolade, a healthcare concierge company serving employers, insurers and health systems, studied the experiences of people covered by health insurance to learn about the differences across age cohorts.
Young Workers (defined as average age less than 30 years) have the most hassles “navigating” American healthcare, which includes many challenges: understanding cots, coordinating care, choosing and understanding the benefits, and finding a doctor “they can relate to,” in the words of the study. Young workers face financial challenges (THINK: student loans, new jobs, new homes) and lack general knowledge about healthcare.
The next age cohort up in the study are Working Families (defined with an average age of 39). This group spends more time dealing with healthcare than younger or older workers — generally as a result of their being in the center of The Sandwich Generation between aging parents and growing children. The cost of health care and medicines, and competing responsibilities (read: stress) are the two top challenges for this consumer segment covered by health insurance.
Older Workers, with an average age of 56, say they effectively manage health care issues — but only 45% give their healthcare a positive rating.
Retirees (average age of 69) have the highest degree of healthcare decision making confidence, and the best healthcare experiences. 59% of retirees positively rate their healthcare. There are many reasons for this which the study didn’t mine, but we know through other research: experience is a great teacher, older people have managed multiple chronic conditions over time, and Medicare is generally a beloved health plan valued by enrollees.
Based on these generation gaps and differences, Accolade recommends that health plan sponsors focus on multi-generational needs, recognizing both the kinds of services different groups need throughout the life journey as well as communicating to people to best connect, resonate and motivate for health engagement.
Health Populi’s Hot Points: While the Accolade/Harris study focused on insured, working health plan members and found generation gaps in healthcare confidence, people who have difficulty navigating the U.S. health system cross socioeconomic groups. In Digitizing the Safety Net, my paper for the California Healthcare Foundation published in February 2016, my own research found that a combination of digital + “in-personal” (the new analog) would be a critical success factor in enabling health plan members to become more effective users (I’ll say “consumers”) of their health plans and health care services.
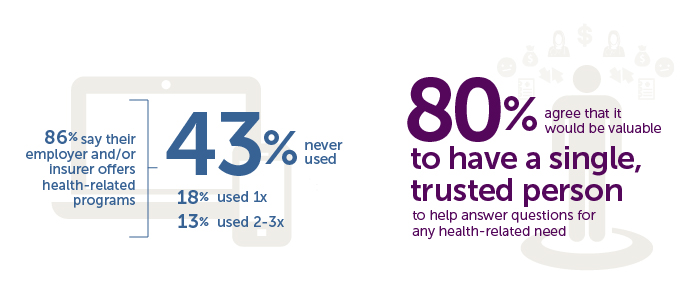
Health care coaches, concierges, patient navigators, and other advocates who partner with people to support personal healthcare journeys are now an important human capital addition to the American health care team. Employers and plan sponsors (especially government funders) spend dearly on health benefits; so do the enrollees, who are essentially the newest payor in U.S. healthcare. There is a significant healthcare literacy gap evident in the Accolade research which younger people openly admit they have.
The youngest workers in the Accolade study call out for the need for this sort of help. They’re not the only ones who need navigational assistance traversing that Rube Goldbergian machine that my friend J.D. Kleinke coined as the great oxymoron — the American healthcare “system.”




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a