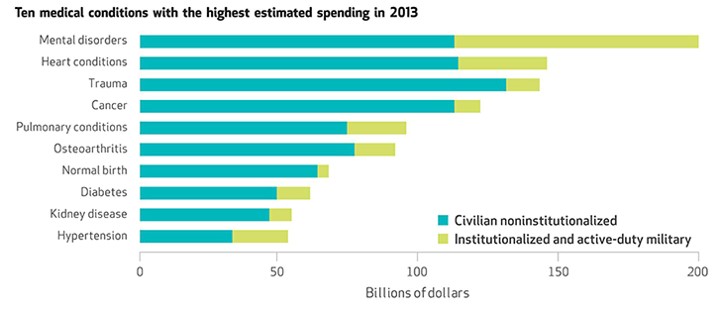
Heart disease and cancer may be the top killers of people who live in the U.S., but the top health spending line item was for mental disorders: $201 billion in 2013.
The chart explains a critical aspect of the spending in that top green portion of the bar: the turquoise segment was for spending on “civilian noninstitutionalized” people, and the green was for “institutionalized and active-duty military.” Mental health issues account, by far, for the largest medical spending in a single condition as shown by the top green bar segment in the chart.
These insights come from the Commerce Department’s Bureau of Economic Analysis’s new Health Care Satellite Account, published in a May 2016 Health Affairs Datawatch article, Mental Disorders Top The List Of The Most Costly Conditions In The United States: $201 Billion.
Spending on mental disorders had a 5.6% annual growth rate between 1996 and 2013, below other faster-growing spending on conditions such as gallbladder, pancreas, and liver, which increased by 10% annually. But since mental disorders command such a large share of spending, the segment topped the list of medical conditions by costs. Heart disease spending, another big category, grew only 2% year-on-year between 1996-2013. Spending on mental disorders displaced heart disease as the #1 cost category in 2013 – heart disease ranked first in 1996, when spending on it was $105 billion and mental diorders, $79 billion.
Health Populi’s Hot Points: The trend of slowed-down costs attributable to heart disease may lead to growing spending for mental disorders — specifically dementia, which increases in prevalence with advancing age. This is the good news/bad news outcome of people winning their personal health battles with heart disease, and aging well into 80s and 90s.
There is also the mental health disease burden of post-traumatic stress which has grown with the lengthening history of America’s participation in wars. The V.A. has been innovating digital health approaches to dealing with PTSD, depression and anxiety. But the burden of disease is substantial, impacting both returning soldiers and their families.
Furthermore, stressors in modern American living, in particular financial stress of managing flat wages and increasing costs of living (and ironically, growing personal health care cost burdens), are driving certain population segments to self-medicate through alcohol and drugs. Some of the opioid epidemic is attributable to this first world, modern-day challenge, with the increasing incidence of death among middle-aged white males.
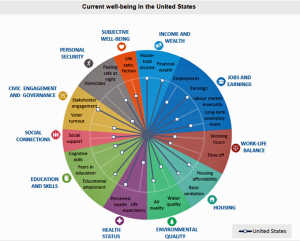 More health care spending may not alleviate this challenge. More social spending could help, in the forms of job creation and retraining support for the new/digital/knowledge economy, broadband to enable social connectivity, and more social safety net supports. The 2016 OECD Better Life Index was published today, illustrating the U.S.’s relatively low status for social support versus other developed (wealthy) nations. Some key findings which may contribute to mental unwellness in America are:
More health care spending may not alleviate this challenge. More social spending could help, in the forms of job creation and retraining support for the new/digital/knowledge economy, broadband to enable social connectivity, and more social safety net supports. The 2016 OECD Better Life Index was published today, illustrating the U.S.’s relatively low status for social support versus other developed (wealthy) nations. Some key findings which may contribute to mental unwellness in America are:
- A large gap between the richest and poorest – the top 20% of the population earn about eight times as much as the bottom 20%
- Lower reading literacy, and
- Lower work-life balance, among other factors.
 The OECD has developed best practices and policy recommendations in its recent report, Fit Mind, Fit Job, connecting the dots between mental health and meaningful employment. Job creation in the U.S., with good salaries, is not only an economic necessity: good jobs are crucial to move the nation’s needle on mental health.
The OECD has developed best practices and policy recommendations in its recent report, Fit Mind, Fit Job, connecting the dots between mental health and meaningful employment. Job creation in the U.S., with good salaries, is not only an economic necessity: good jobs are crucial to move the nation’s needle on mental health.




 Thank you FeedSpot for
Thank you FeedSpot for