 Virtually all employers who offer health coverage to workers extend health benefits to all full-time employees. 94% offer health care coverage to opposite-sex spouses, and 83% to same-sex spouses. One-half off health benefits to both opposite-sex and same-sex domestic partners (unmarried).
Virtually all employers who offer health coverage to workers extend health benefits to all full-time employees. 94% offer health care coverage to opposite-sex spouses, and 83% to same-sex spouses. One-half off health benefits to both opposite-sex and same-sex domestic partners (unmarried).
Dental insurance, prescription drug coverage, vision insurance, mail order prescription programs, and mental health coverage are also offered by a vast majority (85% and over) of employers.
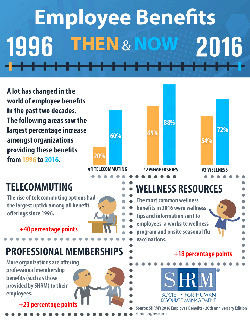
Welcome to the detailed profile of workplace benefits for the year, published in 2016 Employee Benefits, Looking Back at 20 Years of Employee Benefits Offerings in the U.S., from the Society for Human Resource Management.
The report is a hefty, data-dense 80+ pages long, 10 of which are totally devoted to health-related benefits. But in the Health Populi/THINK-Health view on health/care everywhere, other benefit segments bolster health and wellness, including those for employee programs, family-friendly services, financial benefits, flex working, housing, leave, and wellness.
Several emerging health benefits issues stand out for 2016:
- Telemedicine services such as diagnosis, treatment or prescriptions provided by phone or video are offered by 1 in 4 employers (23%)
- 20% of health plans levy a smoking surcharge on employees who smoke
- 17% of employers offer high-deductible health plans that are not linked to an HSA or a health reimbursement arrangement
- Genetic testing is covered in 2016 by 12% of employers (e.g., for assessing cancer risks, etc.)
- 72% of companies serve up wellness resources and information
- The most prevalent wellness offerings include worksite wellness programs and onsite seasonal flu vaccinations; however, SHRM found that certain wellness benefits, including onsite flu shots, 24-hour nurse hot lines, health coaching and insurance-premium discounts for weight loss declined between 2015 and 2016.
There has been some shifting regarding coverage for specific health procedures, treatments and drugs between 2015 and 2016. On the decline are:
- Contraceptive coverage slightly fell from 83% to 80% of employers offering
- Chiropractic coverage fell from 81% to 77%
- Acupressure/acupuncture medical coverage dropped slightly from 37% to 35%
- Bariatric coverage stayed fairly flat at around one-third of employers offering the procedure.
On the increase are:
- Wholesale generic drug programs for injectable drugs (24%)
- Alternative/complementary medical coverage (17%)
- Genetic testing (12%).
Some type of wellness program is offered by 92% of employers, including information (72%), programs in general (61%), and onsite flu vaccinations (54%). Note that some wellness programs are bundled into the healthcare benefit, so these numbers may be under-counted.
Obesity is on the minds of employers, with 37% of companies providing health coaching (declining from 46% in 2015), weight loss programs (31%). and subsidies for gyms (28%). Nutrition counseling is offered by 20% of employers.
41% of employers incorporate incentives for wellness programs, a growing percentage since 2012. 19% of organizations provide health care premium discounts for undergoing a health risk assessment, 17% discount for avoiding tobacco products, and 7% incentivize participating in a weight loss program.
What’s up in terms of wellness benefits are standing desks, provided by 33% of employers, and online fitness centers, among 26% of companies.
Health Populi reports here snippets from the health benefits and wellness sections of the report. But the paper is a treasure trove of benefit details, from “A” (adoption assistance, auto insurance, access to backup childcare service) to “W” (weight loss, wellness), and the benefit alphabet in-between.
SHRM’s report is based on a mail survey among the organization’s membership, with 3,490 HR professionals responding to the survey — a 15% response rate. The sample tends to have more HR professionals from smaller organizations, and private for-profit organizations.
Health Populi’s Hot Points: There was concern just prior to the launch of the Affordable Care Act that employers would collectively exit the role of providing health benefits at the workplace. That scenario has not played out. Instead, employers are taking critical looks at the entire benefit platform, scrutinizing return-on-investment across the many benefit segments and reallocating where payors find greater returns and synergies across the company’s culture of wellness. There’s a rise in financial wellness benefits, socially-oriented benefits, and work-life balance, away from specific wellness categories that have not yielded the desired ROI.
For companies that increased benefits, 58% increased health related ones, and 45% increased wellness programs. For companies that decreased benefits overall, 66% eroded health benefits, 19% wellness, 24% retirement savings and planning.
Based on this, there appears to be a chasm between companies that highly value the health and wellness benefit component, and employers eroding benefits overall including but not limited to health. This may reflect the bias in the study toward smaller, privately-held companies, with fewer larger firms represented in the sample.
It’s important to note the introduction and growth of non-traditional health-oriented benefits: acupressure/acupuncture, behavioral health, alternative and complementary medicine coverage, and the one-third of companies offering standing desks. We are in a morphing era of the health benefit, where companies are re-defining what health and wellness are in the workplace in a larger context of work-life balance and broader definition of whole health. This is in response to employees themselves re-defining their personal definitions of health, which incorporate physical, mental/emotional, appearance, and financial wellness.




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for