 In the past week, the Pharmaceutical Research and Manufacturers of America (PhRMA), the advocacy organization for the branded prescription drug industry, published Medicines: Costs in Context,” the group’s lens on the value of prescription drugs in the larger healthcare economy. Their view: that prescription drug costs comprise a relatively low share of health care spending in America, and a high-value one at that.
In the past week, the Pharmaceutical Research and Manufacturers of America (PhRMA), the advocacy organization for the branded prescription drug industry, published Medicines: Costs in Context,” the group’s lens on the value of prescription drugs in the larger healthcare economy. Their view: that prescription drug costs comprise a relatively low share of health care spending in America, and a high-value one at that.
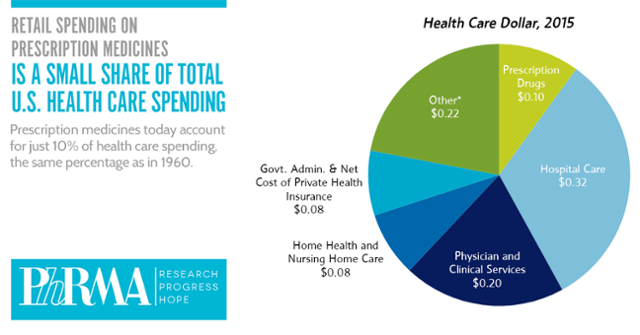
PhRMA contends that 10% of the health care dollar was allocated to prescription drugs in 2015, the same proportion as in 1960. “Even with new treatments for hepatitis C, high cholesterol and cancer, spending on retail prescription medicines is projected to remain approximately 10 percent of U.S. health care spending through 2025 – the same percentage as in 1960. This share of health care spending going toward medicines is providing tremendous value for patients and the health care system,” according to the PhRMA blog.
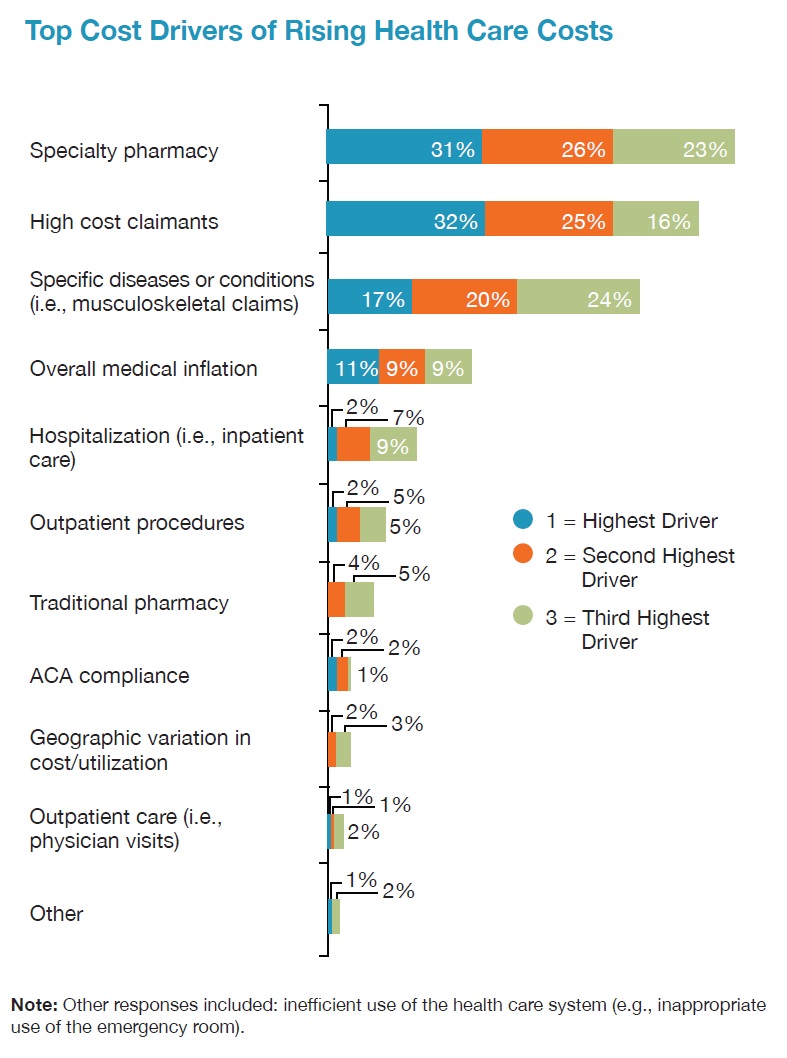
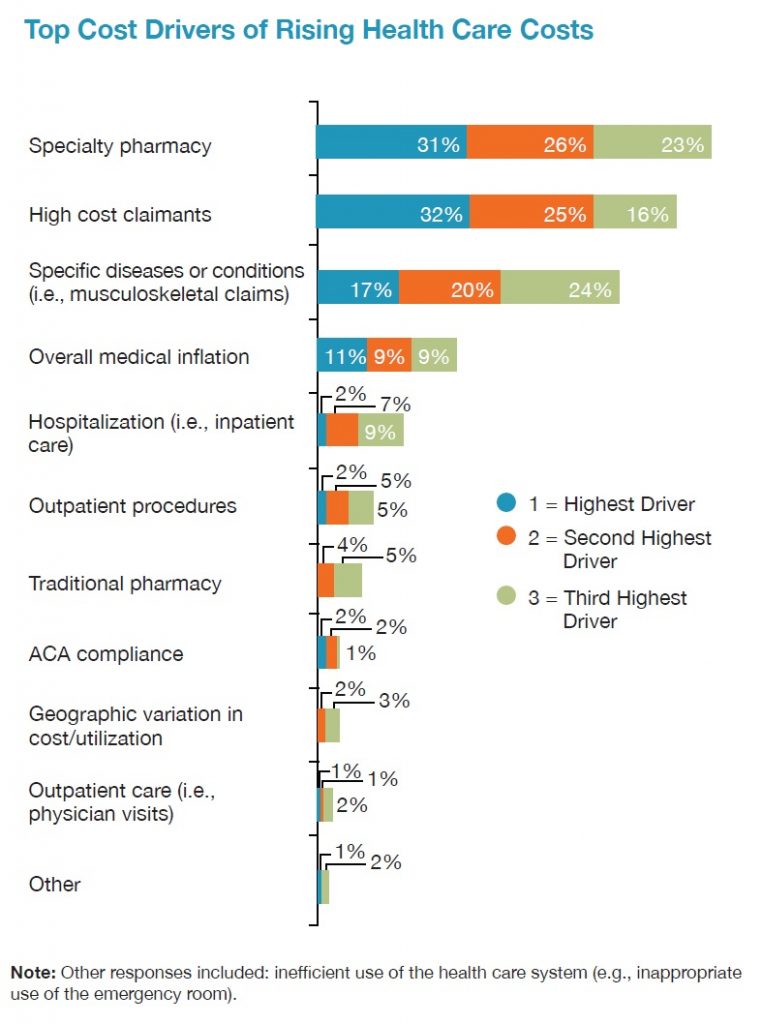 In contrast, yesterday, the National Business Group on Health published their latest read on healthcare costs, citing specialty drug costs as the top driver of rising health care costs. “Fueling the overall growth in the cost of health benefits is the surge in spending on pharmaceuticals, and specialty drugs, in particular. For the first time in the survey, most employers now consider specialty pharmacy the highest driver of health costs and are taking steps to curb them” among 80% of employers in the NBGH survey.
In contrast, yesterday, the National Business Group on Health published their latest read on healthcare costs, citing specialty drug costs as the top driver of rising health care costs. “Fueling the overall growth in the cost of health benefits is the surge in spending on pharmaceuticals, and specialty drugs, in particular. For the first time in the survey, most employers now consider specialty pharmacy the highest driver of health costs and are taking steps to curb them” among 80% of employers in the NBGH survey.
Who’s right? Health value is in the eye of the beholder according to where you play as an industry stakeholder.
The ExpressScripts forecast of specialty drug costs, covered here in Health Populi in March 2016, expected the medicines line item to reach 20% of health care spending in 2020.
Health Populi’s Hot Points: Here at Health Populi, we focus on health care consumers, patients, and caregivers — the end-users of prescription drugs and life sciences products and services. Value-based payment means valuing what matters to patients, a recent JAMA post explained.
Today’s Wall Street Journal features an article on taking in account patients’ perspectives before entering heart surgery, part of a growing program in Medicare to promote shared decision-making in health care. We have entered “a very different mindset than the era where the physician was the decision-maker,” Harlan Krumholz of Yale University is quoted. The article talks about a new cardiac device, the Watchman, designed to assist patients with atrial fibrillation (aFib, irregular heartbeat) to prevent strokes. Standard treatment for aFib is for patients to take blood thinners that preent clotting that can lead to strokes. But medications can have side effects like bruising and risks for excessive bleeding, which the Watchman avoids.
As patients pay growing proportions of health costs, they must play the role of consumer — albeit a difficult mantle to bear at this painful stage of pioneering health care consumerism. PhRMA, employers that sponsor health insurance programs, the insurance industry itself, hospitals and health care providers, and all industry stakeholders must play a part in surrounding their products and services with programs that bolster consumers’ health literacy, health plan literacy, and health financial literacy so people can play their part in making sound healthcare decisions based on their own values.
Too many health consumers don’t realize or have confidence that they actually can influence, and ultimately own, these decisions about their own health and the health of their loved ones.




 Thank you FeedSpot for
Thank you FeedSpot for