 “Today’s primary care won’t work tomorrow,” given the shortage of primary care providers (PCPs) and the need to do more in healthcare with fewer resources in the emerging value-based economy. So let’s re-imagine primary care models, PwC asserts, and makes the case in their report, ROI for primary care: Building the dream team.
“Today’s primary care won’t work tomorrow,” given the shortage of primary care providers (PCPs) and the need to do more in healthcare with fewer resources in the emerging value-based economy. So let’s re-imagine primary care models, PwC asserts, and makes the case in their report, ROI for primary care: Building the dream team.
What’s the financial impact of this dream team on healthcare providers? It’s potentially $1.2 million in savings for every 10,000 patients served, PwC calculates.
Historically, physicians have been loath to share their work with non-physicians because of how doctors have been paid — on the basis of fee-for-service, being paid for volume of work (e.g., visits, tests, clinical imaging encounters, etc.). But as physicians are taking on more financial risk for patient outcomes, to deliver value, or work within payment “bundles” (say, for joint surgery under Medicare payment).
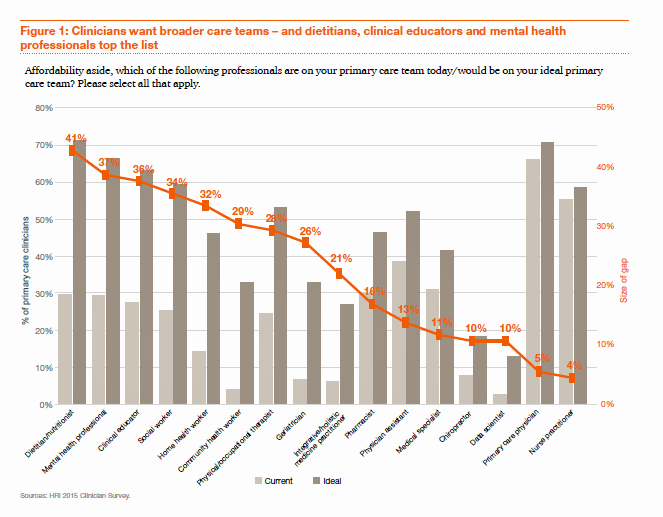
When faced with value-based pay models, doctors become keener on team-based care, more broadly defining the “team” to include dietitians, mental health providers, health educators, social workers, and home health workers. These and other potential members of the primary care dream team are shown in the bar chart, in terms of who’s working on the team currently (the light grey bars) and which roles are seen as ideal (the dark grey bars).
That’s the clinician side of the survey. Consumers’ interests in the dream team for primary care vary by a person’s medical and social needs, PwC found. People who are frail and aging more highly value a broad range of services, such as nutrition support, DIY diagnosis, telemedicine, home care, and prescription drug management. Healthier adults look to DIY diagnostics and home health. People managing chronic conditions are also interested in self-diagnostics, telemedicine, and home health.
Across-the-board, at least 21% of consumers have decided not to seek medical care due to cost at least once in the past year. Note that such self-rationing of care due to cost impacted 41-60% of consumers who were frail elderly, dealing with mental health issues, healthy families, and healthy adult skeptics (based on PwC’s consumer segmentation typology).
For this study, PwC surveyed 1,500 U.S. PCPs, specialists, nurse practitioners, physician assistants and pharmacists, along with 1,750 U.S. consumers, in the summer of 2016.
 Health Populi’s Hot Points: Around the world, developed nations with strong primary care backbones are those that are the highest performing healthcare systems. These countries also tend to spend more resources on “social care” than health care.
Health Populi’s Hot Points: Around the world, developed nations with strong primary care backbones are those that are the highest performing healthcare systems. These countries also tend to spend more resources on “social care” than health care.
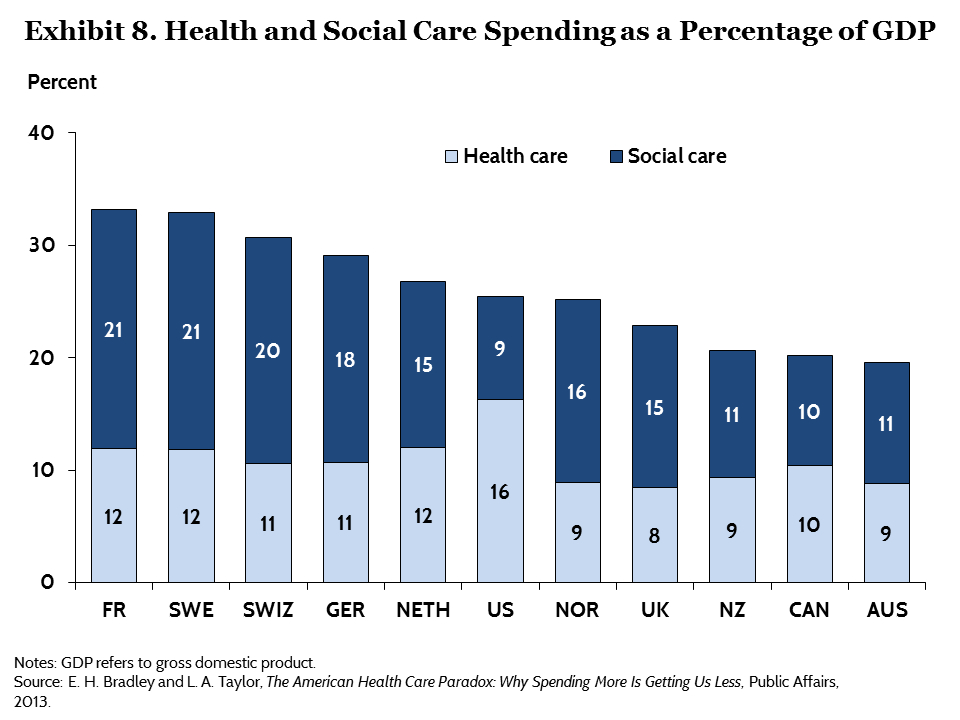
The second chart tells the story: the U.S. spends a much greater percent of national gross domestic product (GDP) on healthcare than other developed countries do. But peer nations spend greater proportions of their national GDP on social care than the U.S. does.
Health policy analysts and health care providers alike in America area growing to recognize the central importance of the social determinants of health on individuals’, and the public’s, health. New health/care delivery models are emerging in the U.S. to deal with this reality, building their own dream teams to bolster primary care and address people where they live (at home), work (at employers’ sites), play (at gyms and on playgrounds), pray (in faith-based institutions) and learn (at schools and university campuses). Look to Clover Health, Iora Health, Omada Health, and Purple Binder as examples of these new care approaches who are early adopters and solvers of the primary care dream team vision.




 Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a