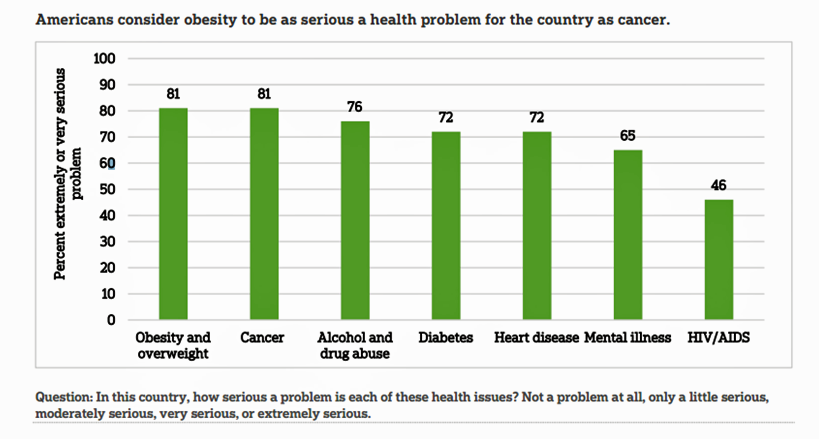
 60% of Americans are currently trying to lose weight. So it shouldn’t be a surprise that when asked, “what’s the most serious health problem in the United States?” Americans say it’s obesity, tied with cancer, and ahead of heart disease and diabetes. Overweight and obesity are top-of-mind for most Americans, according to research conducted by the American Society for Metabolic and Bariatric Surgery (ASMBS) and NORC at the University of Chicago. This research has created two reports which can be accessed at the link.
60% of Americans are currently trying to lose weight. So it shouldn’t be a surprise that when asked, “what’s the most serious health problem in the United States?” Americans say it’s obesity, tied with cancer, and ahead of heart disease and diabetes. Overweight and obesity are top-of-mind for most Americans, according to research conducted by the American Society for Metabolic and Bariatric Surgery (ASMBS) and NORC at the University of Chicago. This research has created two reports which can be accessed at the link.
The survey, conducted among 1,509 consumers in August and September 2016, found that Americans’ understanding of obesity’s risks for chronic disease (namely diabetes, heart disease, high blood pressure, and cancer) has improved since a similar study was done in 2013. However, there remain misconceptions on how to effectively address the obesity epidemic, posing opportunities to better educate the public on obesity’s role in health and available treatments beyond the peoples’ favorite: diet and exercise.
While most consumers agree on the health risks of obesity, many people who are obese do not seek help from the health care system to help them deal with the issue. ASMBS perceives that consumers and the medical profession are on different pages about the condition: that clinicians have reached a consensus that obesity is a disease (cited as such by the AMA in 2013), only one-third of Americans call obesity a disease. Instead, most consumers say obesity is a risk factor for other diseases. Furthermore, people who believe obesity is a lifestyle issue are less likely to talk to a doctor about their weight.
Medical consensus among clinicians is that obesity is caused by several factors: behavioral, emotional, environmental, and genetic. But most Americans with obesity tend to believe that obesity is based totally on lifestyle choices, with the main barrier being lack of willpower (perceived by more men than women).
One in 3 Americans know someone who died or developed a disease because of obesity. People with such a connection are more likely to call out the severity of obesity and its link to other conditions. These people are more likely to “take weight seriously in their own lives,” the report notes, “more often report talking to a doctor about their own weight” and thinking through the role of weight in other parts of their lives.
There’s a Mars/Venus difference in how men see themselves as overweight vs. obese compared with women. About two-thirds of men who are overweight or obese underestimate their weight. Men are less likely to recognize obesity in themselves compared to women: less than half of women who are overweight or obese underestimate their weight, the survey found.
In this political season, it’s also interesting to note a party difference on the role of prevention in public policy: while 95% of Democrats and Independents believe something should be done to prevent obesity, only 78% of Republicans support such a prevention policy.
 Health Populi’s Hot Points: Most people say “willpower” is the key barrier to dealing with obesity, followed by fair-priced, accessible healthy foods.
Health Populi’s Hot Points: Most people say “willpower” is the key barrier to dealing with obesity, followed by fair-priced, accessible healthy foods.
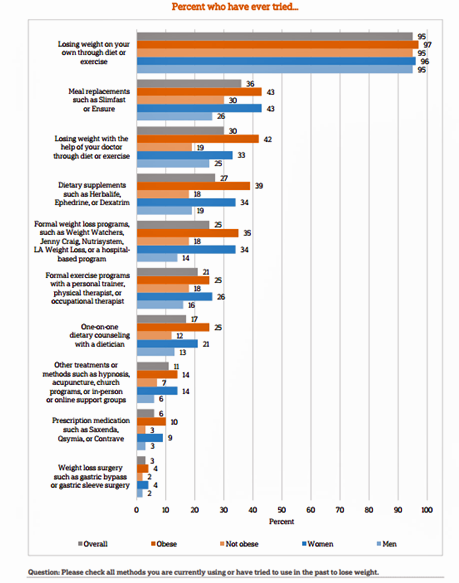
Nearly 100% of people have tried to lose weight through diet and exercise (on their own): the go-to tactic for weight loss. 78% of people believing diet and exercise are most effective for weight loss. However, this has not been borne out by both individuals’ experience on sustained weight loss as well as an evidence base of clinical research.
Most Americans (78%) believe that health insurance should cover losing weight with the help of a doctor through diet or exercise. weight loss surgery (75%), one-on-one dietary counseling (73%), prescription medications (61%), and formal exercise programs (60%).
But most people who are obese haven’t yet approached their physicians to discuss these options — whether insurance currently would pay for the various approaches or not.
Due to the multi-factor nature of obesity that goes well beyond the norm of diet-and-exercise, closing the chasm between consumers who are obese and their health care providers would be one important strategy to help deal with America’s overweight epidemic. There is compelling research, too, that supports a social role, peer-to-peer support, in weight loss beyond “going it alone” for diet and exercise, detailed in Christakis and Fowler’s work, Connected. In addition, Michele Segar’s research published in her book No Sweat provides compelling research into how people can look at exercise as a gift and not a chore, taking into account the a key barrier to sustaining behavior change.
What we know we know through ASMBS and NORC’s two reports is that overweight and obesity are issues that the bulk of Americans, Democrats and Republicans, men and women, think about a lot. The issue is deeply embedded into our popular culture. As the medical system takes on more value-oriented payment, health care providers must bundle into care the social determinants of obesity and overweight — access to nutritious food and places to move around safely and accessibly, insurance coverage for treatment, social care for conversations and counseling, and broadband connectivity to be able to access social networks for peer-to-peer social health.




 Thank you FeedSpot for
Thank you FeedSpot for