This blog appears today as part of a #HIMSS18 primer series for attendees, and the industry at large, to discuss major health IT issues that will help move health and healthcare delivery forward in 2018 – and beyond. I’m grateful to HIMSS to be one of 20 Social Media Ambassadors appointed for this year’s conference, which convenes in Las Vegas at the Sands Expo Center from March 5 to 9th, 2018.
Prioritizing the patient-as-consumer through my health economic lens, the biggest priorities will be:
- Engaging patients in self-care and driving health and health plan literacy to better manage constrained access and payments
- Dealing with healthcare provider burnout due to bureaucratic tasks and high-expectation patient demands
- Delivering right-sized care based on the most current clinical evidence to all patients, regardless of personal or financial factor
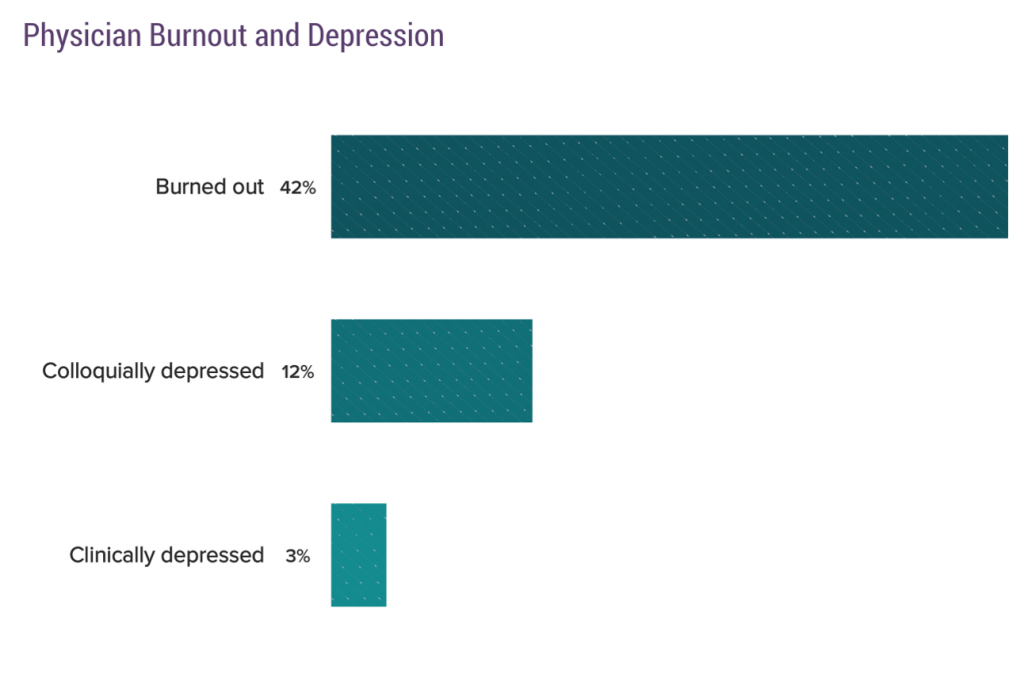 Healthcare providers are the front-line stakeholders who, increasingly, are taking on payment and incentives to help manage individual patient and communities’ health. More hospitals are physicians’ employers, and so bear the responsibility of supporting doctors and nurses in working to their highest and best use – especially empowering professionals in their patient care missions. The just-released Medscape National Physician Burnout and Depression report for 2018 reveals that 42 percent of doctors feel burned out – largely due to bureaucratic and administrative tasks.
Healthcare providers are the front-line stakeholders who, increasingly, are taking on payment and incentives to help manage individual patient and communities’ health. More hospitals are physicians’ employers, and so bear the responsibility of supporting doctors and nurses in working to their highest and best use – especially empowering professionals in their patient care missions. The just-released Medscape National Physician Burnout and Depression report for 2018 reveals that 42 percent of doctors feel burned out – largely due to bureaucratic and administrative tasks.
However, adopting and implementing poorly designed electronic health records (EHRs) has diminished the time available to clinicians to lay hands and eyes on patients – essentially, limiting their ability to do the jobs they were trained, hired and personally driven to do. This is a case of unintended consequences: the important research of Dr. Christine Sinsky and colleagues has shown that so much health IT has sub-optimized care processes, workflows and the important relationships between clinician and patient that both parties want to have.
Most physicians entered the profession, Medscape found, to form such relationships. The time tug of war between too many bureaucratic tasks coupled with lack of time to nurture patient relationships contributes to clinician stress and the added fourth leg of the Quadruple Aim – the Triple Aim with the addition of addressing provider burnout and drop-out.
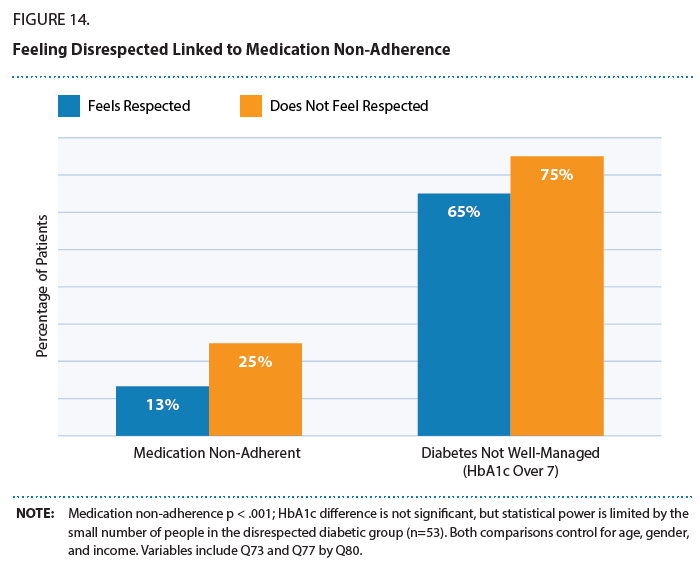 Still, clinicians need to hone their webside manner, listening and empathy skills. Patients are more adherent to medication regimens when people feel more respected in the clinical encounter and achieve better outcomes when managing chronic conditions like diabetes.
Still, clinicians need to hone their webside manner, listening and empathy skills. Patients are more adherent to medication regimens when people feel more respected in the clinical encounter and achieve better outcomes when managing chronic conditions like diabetes.
Payor, insurer and employer stakeholders can better align healthcare outcomes with health-making by more artfully designing health plans than nudge people to take better care of themselves, fund services that can address chronic healthcare conditions, and arm people with tools to share in decision- and health-making.
Patients/consumers also bear responsibility in helping make a better healthcare system. See that roughly equal proportions of patients themselves say they along with healthcare providers are responsible for improving health. The chasm between “say” they’re responsible and acting on that promise can be addressed through provider supports – both analog (read: empathy and humanity) and digital (via useful tools clinicians vet and curate for effectiveness and user-centered design).
Barriers and Opportunities for Progress
People have become Amazon-primed, benchmarking consumer expectations at a level beyond what the healthcare industry has typically delivered. Healthcare must adopt UX/UI that underpin technologies solving real patients’ and providers’ problems to streamline life- and work-flows.
There’s also a trust deficit between some patients and providers. But trust is a precursor to health engagement, so trust can be a barrier to patients and providers working together to improve healthcare. In addition to the EHR/screen-time challenge, there’s also a data/health information concern: patients expect health providers to be good data stewards, protecting personal health information.
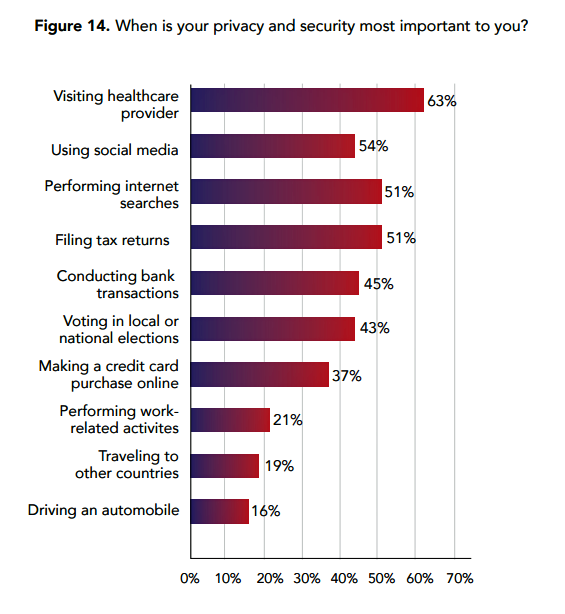 Most consumers say visiting healthcare providers is where privacy and security is most important, the Ponemon Institute found. The frequency of cybersecurity breaches in health systems is a risk factor eroding patient trust. To that end, it is interesting to note that Amazon is seeking a privacy professional experienced with HIPAA.
Most consumers say visiting healthcare providers is where privacy and security is most important, the Ponemon Institute found. The frequency of cybersecurity breaches in health systems is a risk factor eroding patient trust. To that end, it is interesting to note that Amazon is seeking a privacy professional experienced with HIPAA.
Finally, healthcare costs are top-of-mind for patients in the U.S. Financial toxicity is a growing concern among oncologists treating patients with cancer, for example. Doctors and patients want to discuss healthcare costs and have greater transparency available for healthcare products and services.
Technology solutions can be designed to address each of these three barriers (consumer service expectations, trust and data security, and financial transparency).
What to Look for at #HIMSS18
It is exciting to see so many panels and speakers addressing the patient and consumer as the “noun” in healthcare this year at HIMSS18. Here are some of the sessions I recommend that, together, will address many of the issues I’ve discussed in this post.
- Connected Patient Forum | #Engage4Health + #HIMSS18
- Innovation Symposium Closing Keynote – Health Happens Everywhere | #Aim2Innovate + #HIMSS18
- Patient Engagement – It Takes a Village | #Engage4Health + #HIMSS18
- Creating Delightful Consumer Experiences: What Can We Learn From Other Industries? | #Engage4Health + #HIMSS18
- Patients as Consumers: How Leading Providers are Digitally Transforming Patient Consults | #Engage4Health + #HIMSS18
- A New Era: The CMO’s Role at the Healthcare Consumerism Table | #Engage4Health + #HIMSS18
- Connected Care: VA, Virtual Health and the Patient Experience | #Engage4Health + #HIMSS18
- Tailored Conversations for Consumer Activation | #Engage4Health + #HIMSS18
Follow and continue this conversation via the following hashtags and communities: #HIMSS18, #Engage4Health, #Aim2Innovate




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for