As I wrote here in April 2017, telehealth and virtual healthcare are mainstreaming.
This week at the 2018 annual HIMSS conference, telehealth is playing a mainstream role in discussions about right-sizing and right-placing healthcare.
The evidence for telehealth’s tipping point is rooted in new research published today by Accenture on Patients + Doctors + Machines, Accentures’ 2018 Consumer Survey on Digital Health.
I sat down today with Dr. Kaveh Safavi who leads Accenture’s healthcare practice to discuss the results of this study into peoples’ atttudes toward healthcare technology and innovation.
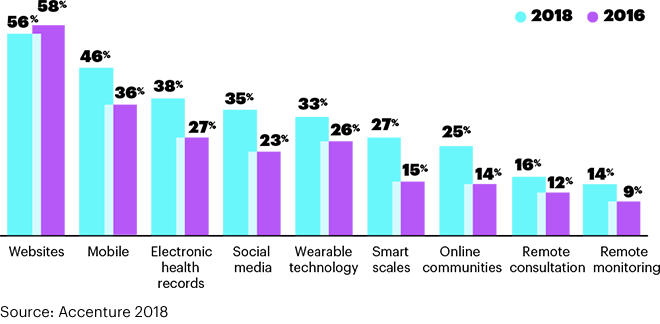
Three in four consumers in America say technology is important to managing their health. Consumers most commonly use the following technologies to help them manage health in 2018:
- 56% use websites
- 48% mobile app
- 38% electronic health records
- 35% social media
- 33% wearables
- 27% smart scales
- 25% online communities, and
- 14% remote monitoring.
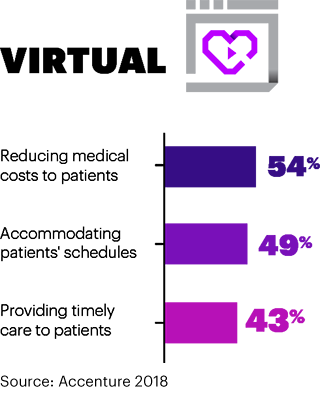
The most important advantages of virtual care have to do with cost and convenience, shown in the second chart. Half of Americans believe virtual care services can reduce medical costs to patients and accommodate patients’ schedules, and another 43% of consumers say that virtual care can provide timely services to patients. FYIm Accenture defines virtual services as video or voice transmitted by a provider either synchronously (in real-time) or asynchronously.
Patients’ views on the advantages of virtual are de-valued through consumers’ lenses on quality, engagement, and the speed of diagnoses.
There are two axes to consider when it comes to consumers’ current views on virtual healthcare options vs. in-person F2F with a clinician: those axes are trust and risk.
“When trust is high and risk is low,” Kaveh explained, “People can have asynchronous email” with their providers. “When trust is low and risk is high, we need to be in the same room. Health hasn’t offered us many options” before the emergence of the telehealth/virtual health continuum of choices, Kaveh pointed out.
We discussed other research demonstrating that the proportion of consumers who use alternatives to seeing “their” primary care provider, like telemedicine and retail clinics, is growing. A key reason these patients seek alternatives to F2F visits with their personal physicians is that they want to “get something done.” Convenience and the “Amazon Prime’ing” of consumers has come to health care underpinning consumerism.
Trust underpins health engagement, and that directly relates to the sharing of personal health information. Accenture found that 90% of consumers are willing to share health data from wearable devices with physicians and nurses, and 75% with their family. Surprisingly (to me), 72% of consumers said they’d share their health data with a health insurance plan. But only 38% would share wearable health data with an employer, and 41% with a government agency.
Here, instead of trust vs. risk, the factors to consider are trust vs. benefit, Kaveh counsels.
Accenture surveyed 2,301 U.S. adults 18 years of age and over between October 2017 and January 2018 for this survey.
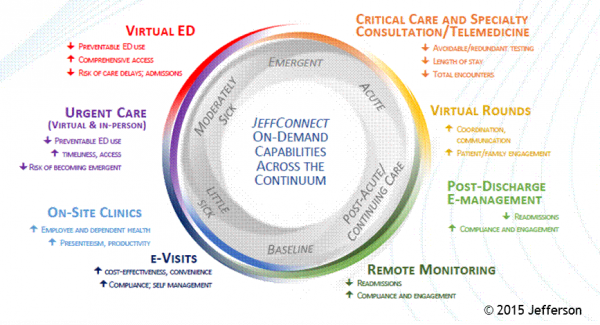
Health Populi’s Hot Points: This morning, I had the honor of participating as a judge in Microsoft’s annual Health Innovation Forum. Dr. Judd Hollander of Thomas Jefferson University Health System shared his experience launching JeffConnect, which is the organization’s telehealth platform. The program provides a full continuum of healthcare access to patients both within and outside of the TJU network. “A little sick” patients can access care at the 6 o’clock point of the diagram, all the way across the patient spectrum to post-discharge and remote monitoring at home.
Dr. Hollander provided hard evidence for consumers’ embrace of telehealth based on his experience with both clinicians and patients who are using JeffConnect. My favorite of his many quotable insights was the following:
“When a patient is doing a telemedicine call for 10 minutes with a patient, she’s not hell-bent to get antibiotics. But if she waits four hours in the ER and doesn’t get antibiotics, she’ll have something to say about it.”
Thus, virtual health can drive efficiency, right-sized healthcare, and greater patient satisfaction. These are key ingredients into migrating to the Quadruple Aim.




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for