What will telemedicine look like in 2030? imagined Kaveh Safavi, Accenture’s Senior Managing Director and Health of Global Healthcare Practice. Kaveh was brainstorming the future of telehealth a decade from “now,” with three innovators attending #ATA19: Deepthi Bathina of Humana, Matthew Holt of Catalyst Health (and Co-Founder of Health 2.0), and Kim Swafford of Providence St. Joseph. This week convened the ATA annual conference where healthcare industry stakeholders met up to deal with the current telehealth environment and imagine what the future prospects would/could be.

As Kaveh invoked the futuristic theme, I couldn’t help thinking about Elroy Jetson, pictured here in a kind of FaceTime/Skype-type visit with a clinician sometime in the future that Hanna-Barbera produced in my childhood.
”Telemedicine used to be about solving access to no care,” Kaveh introduced the conversation. “Now, it’s about serving people who already have care through different mechanisms.”
This quartet of innovative digital health thinkers discussed the pace of adoption for telehealth, moving from the current state to 2030 and working backward from there, asking what conditions would have to change to get us from “here” to telehealth as, well, a healthcare delivery channel norm.
Today, fewer than 1% of Medicare beneficiaries have had any telehealth encounter, Kaveh explained, and fewer than one in eight doctors are aware of offering telehealth in their practice.
Deepthi from Humana offered three considerations concerning how care will transform. First, connected care: one in five U.S. households have a smart device, Deepthi noted. In 2018, after Amazon acquired PillPack, the company filed a patent for Alexa that would observe a consumer’s cough or sneeze and predict the onset of depression or disease. By 2030, she imagined, Alexa would recognize this before we do and a drone might drop something off at our doorstep before we even know we have a problem.
Deepthi added two more elements: individualized care, personalized to each of us; and, standardized care, perhaps using a digital twin, in a system that cares for me employing established standards based on the latest knowledge culled through machine learning/AI.
 Kim Swafford of Providence St Joe’s knows a lot about telehealth “today” because her organization is on the forefront of leveraging digital and virtual health modes. Providence St. Joe’s deploys telehealth in eight states. She asserts that leveraging AI and machine learning for low acuity issues can automate as much as 80% of care, for both physical and behavioral/mental health.
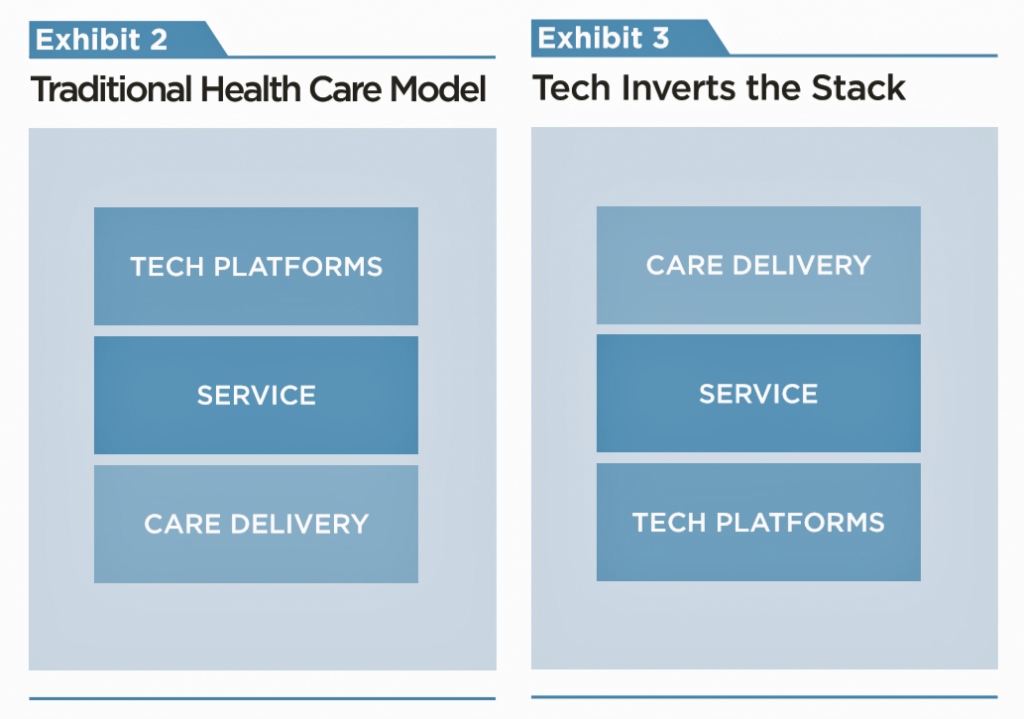
Kim Swafford of Providence St Joe’s knows a lot about telehealth “today” because her organization is on the forefront of leveraging digital and virtual health modes. Providence St. Joe’s deploys telehealth in eight states. She asserts that leveraging AI and machine learning for low acuity issues can automate as much as 80% of care, for both physical and behavioral/mental health.Matthew talked about the “Flip the Stack” concept that he and Indu Subaiya, his partner in Health 2.0, developed for the World Congress on Health and Medical Sociology in December 2018. They imagined a scenario where, say, Alexa version 5 was the home platform enabling daily living, including health care delivery at home. From their talk’s abstract: “Starting with technology, the sensors, trackers, AI systems and processes are soon going to be in place monitoring, measuring and suggesting next steps to both providers and patients.” That sounds very 2030, but also do-able with the eleven-year time horizon.
The quartet discussed whether the demand (consumer/patient/caregiver) side would push telehealth adoption, or whether the supply side would. On the consumer side, younger people — namely, Millennials and Gen Z cohorts — are behaving today as if they do not value a primary care medical home, instead, favoring an on-demand, just-in-time-on-my-timeline mode. This would conform with other services in daily life flow, from shared rides to GrubHub food delivery, as health behavior morphs into more general consumer behavior patterns. Matthew pointed to latent demand for Lyft and Uber supplying that demand, which brought cheaper transport into peoples’ hands. “But how to get cheaper care into the hands of consumers?” he asked. We have this for some aspects of health and wellness services, choosing to deliver children in different settings, the supplement industry market, and chiropractic, Matthew commented.
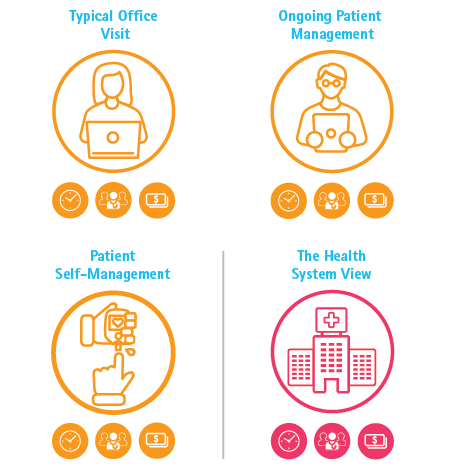 Health Populi’s Hot Points: In full disclosure, I worked with Kaveh and the Accenture team on a recent study modeling the economic value of shifting a portion of ambulatory care visits to virtual care settings. The report’s title summarized what we calculated: Virtual Health: The Untapped Opportunity to Get the Most out of Healthcare. We modeled three scenarios: a typical primary care office visit, ongoing patient management dealing with a chronic condition, and patient self-management at home. Our scenarios combined virtual health and traditional in-person patient care to reflect a hybrid model of care, reflecting how life really works in an omni-channel world for healthcare and other daily life-flows. By saving even five minutes’ time per patient, our model calculated that a health system could conserve 320 primary care providers (PCPs) and save about $63 million for these three use cases taken together.
Health Populi’s Hot Points: In full disclosure, I worked with Kaveh and the Accenture team on a recent study modeling the economic value of shifting a portion of ambulatory care visits to virtual care settings. The report’s title summarized what we calculated: Virtual Health: The Untapped Opportunity to Get the Most out of Healthcare. We modeled three scenarios: a typical primary care office visit, ongoing patient management dealing with a chronic condition, and patient self-management at home. Our scenarios combined virtual health and traditional in-person patient care to reflect a hybrid model of care, reflecting how life really works in an omni-channel world for healthcare and other daily life-flows. By saving even five minutes’ time per patient, our model calculated that a health system could conserve 320 primary care providers (PCPs) and save about $63 million for these three use cases taken together.This small study is but one data point and insight into how telehealth can help bend the cost curve to help remake a sustainable U.S. healthcare system. Any designs on healthcare reform, whether broad public/private universal healthcare or tightly defined Medicare4All, must move care outside of ultra-expensive care settings. Let’s be mindful that in espousing whatever flavor of healthcare reform we debate in the coming months, we ensure affordability, good design, and consumer engagement in places convenient to people — especially, in the home as Indu and Matthew imagine in their Flip the Stack future world.




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for