A study in JAMA published this week analyzed research reports that have measured waste in the U.S. health care system, calculating that 25% of medical spending in America is wasted. If spending is gauged at $3.8 trillion, waste amounts to nearly $1 trillion. If spending is 18% of the American gross domestic product (GDP), then some 4.5% of the U.S. economy is wasted spending by the health care system and its stakeholders.
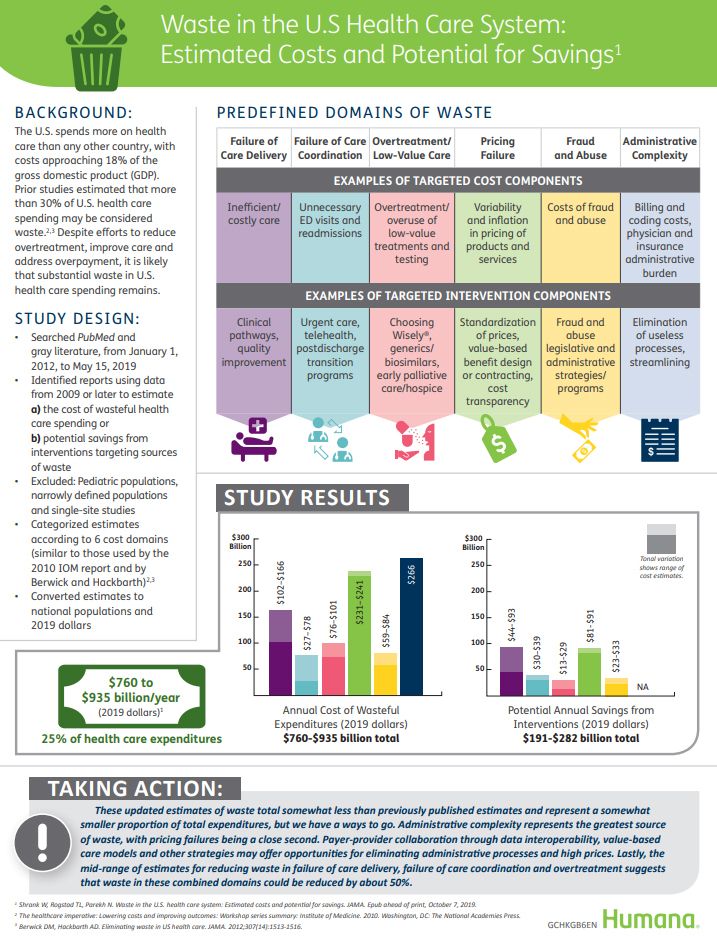
In “Waste in the US Health Care System,” a team from Humana and the Univrsity of Pittsburgh recalibrated the previous finding of 30% of wasted spending to the 25%, which equates to a waste-range of $760 bn to $935 bn.
The study reviewed reports and articles published between January 1, 2012 and May 15, 2019, dressing the topic of waste across six domains previously identified by the Institute of Medicine:
- Failure of care delivery, with waste ranging between $102 bn and $166 bn
- Failure of care coordination, with a waste-range of $27 bn – $78 bn
- Over-treatment or low-value care, waste between $76 bn – $101 bn
- Pricing failure, with waste ranging $231 bn – $241 bn
- Fraud and abuse, waste between $59 bn and $84 bn; and,
- Administrative complexity, wasting about $266 bn each year.
Thus, administrative complexity, which includes billing and coding waste, and physician time spent reporting on quality measures, accounted for the largest component of waste in American health care. This category comprised roughly one-third of the total waste in U.S. medical spending.
The second largest waste component was pricing failure, associated with medication pricing failure (the largest piece of three components), payer-based health services pricing failure, and lab and ambulatory pricing. Pricing failure as a waste-factor accounted for nearly another third of total waste in U.S. health care.
The third largest waste piece was failure of care delivery. This challenge covers hospital-acquired conditions and adverse events, clinician-related inefficiency, and lack of adoption of preventive care practices like administering vaccines and addressing obesity and hypertension.
The authors discuss the potential for savings — that is, how to bend the waste-curve of 25% down to some lower level. They first point to administrative complexity, the largest piece of the waste-pie. Fragmentation in payment and delivery costs the U.S. health care system mightily. Lack of interoperability of data systems is one area that’s improving, slowly. More savings would accrue through the quicker adoption of value-based payment models, the authors assert, where clinicians take on financial risk for managing population health.
Pricing failure, the second big waste factor, is predominantly challenged by pharmaceutical/prescription drug pricing based on this research. The Centers for Medicare and Medicaid Services (CMS) forecasts that prescription drug spending will be the fastest-growing cause of rising health spending by 2027.
Health Populi’s Hot Points: The arithmetic of this report suggests that two domains of the six waste categories contribute to about $2 in $3 of waste: administrative complexity and pricing failures, the latter largely due to prescription drug pricing.
Political debates in this 2020 U.S. election cycle have been addressing these two issues: first, in the continuum of policies for reforming the U.S. health care system from reinvigorating the ACA/Obamacare (the Joe Biden approach), with a call for a public option and/or “Medicare for those who want it” in Buttigieg-speak; with Medicare-For-All the other end of the policy spectrum, supported explicitly by Bernie Sanders and Elizabeth Warren.
On the more granular policy front is the regulation of prescription drug pricing, with policy prescriptions ranging from using reference pricing based on global rates calculated in other peer countries, to controlling prices for specific drugs (say, the most-used Rx’s among Medicare members or the top N number of drugs used by all U.S. patients).

As we continue to debate the merits of these approaches, one fact that distinguishes the U.S. health system apart from all other nations’ healthcare organizations has prevented systemic, foundational reform over the past twenty years: that is the Whac-A-Mole game that is health care spending in America. One stakeholder’s revenue is another’s cost when you press down on one segment in U.S. health care. American workers have traded off wages for growing health spending for twenty years based on this health spending supply side logic.
On the demand side — as the patient is becoming a growing force as Payor — will patients-as-consumer-payors articulate their demand to exorcise wasted spending, taking on their mantle as Health Citizens?
That’s the Holy Grail and vision in my book, HealthConsuming: From Health Consumer to Health Citizen. How that demand side will reconcile with the supply side of pharmaceutical and life science companies, health insurers, retail pharmacy, hospitals and physicians — all strong and assertive lobbies inside the Beltway — will become clearer over the next thirteen months. On the consumer and patient side, the AARP, patient advocacy groups, and increasingly visible and assertive patient social networks are more in the mix on Capitol Hill than they were a decade ago.
Standard operating procedure for my own advisory work looking at this health policy future state involves ongoing scenario planning with a long list of uncertainties and wild cards mashed into the mix depending what stakeholder you are.




 Thank you FeedSpot for
Thank you FeedSpot for