 “Having 20/20 vision does not necessarily mean you have perfect vision. 20/20 vision only indicates the sharpness or clarity of vision at a distance,” according to the American Optometric Association.
“Having 20/20 vision does not necessarily mean you have perfect vision. 20/20 vision only indicates the sharpness or clarity of vision at a distance,” according to the American Optometric Association.
An important vision skill, the AOA tells us, is “peripheral awareness or side vision” which contributes to overall visual acuity.
So it is with scenario planning in health care, a key work-flow this time of the year for me with my clients spanning the health/care ecosystem from providers to payors to Big Food, electronics and tech, and financial services. In the fourth quarter each year, I’m typically occupied with scenario planning, “thinking the unthinkable” as Herman Kahn of RAND, a godfather of the method (and no relation to me) described the process.
Here are the key factors we’re incorporating into health ecosystem plans, filtering their import and impact by industry segment. This is my gift to Health Populi readers, asking you to ponder how these driving forces shaping health consumers could shake up your businesses and work-worlds in the next year and beyond…
We’ll start with some knowns, first with Trust, Mis-Trust, and Big Tech Animus. The most important factor that underpins peoples’ engaging with their health and health care organizations is trust…and distrust in America is up, the Pew Research Group told us earlier this year in their report on Trust and Distrust in America.
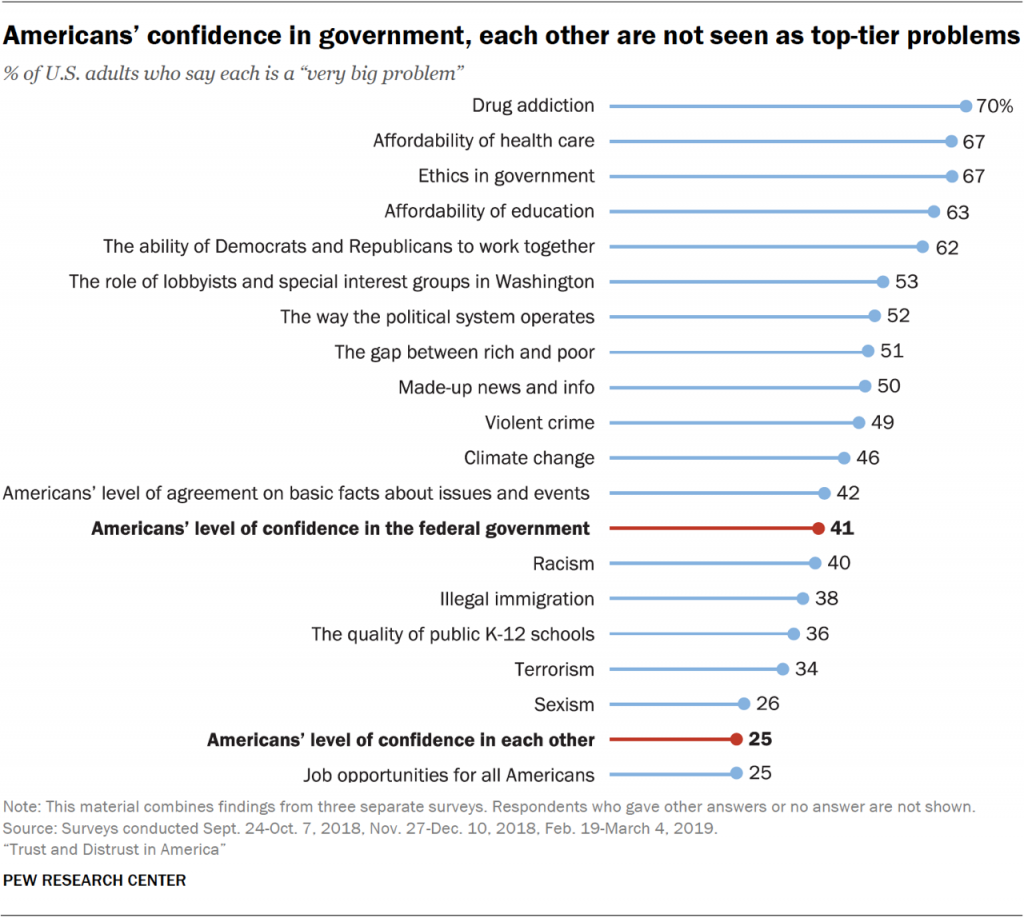 A tectonic force underneath growing distrust and mis-trust is a “techlash,” coined by the Information Technology and Innovation Foundation in this report, finding in their words, “growing animus toward Big Tech companies.” A growing cohort of people have begun to diss and cut off social network connections and take actions to better control their personal information where they can. And this has and will have an impact on the good actors in health/care who have been building patient social networks for good – for research, for peer-to-peer support, and for patients wanting to pay-it-forward for future peers who will share their conditions.
A tectonic force underneath growing distrust and mis-trust is a “techlash,” coined by the Information Technology and Innovation Foundation in this report, finding in their words, “growing animus toward Big Tech companies.” A growing cohort of people have begun to diss and cut off social network connections and take actions to better control their personal information where they can. And this has and will have an impact on the good actors in health/care who have been building patient social networks for good – for research, for peer-to-peer support, and for patients wanting to pay-it-forward for future peers who will share their conditions.
Self-Rationing Healthcare is a New Normal in America. At least one in two people living in the U.S. has avoided medical services for nearly a decade, based on annual surveys from the Kaiser Family Foundation and others. In 2020, avoiding care will be a new normal for even more people, a fact of American health life explained in a recent survey from NRC titled, The Decade of Deferment. Until health plans adopt more artful designs incorporating behavioral economic nudges that are meaningful and relevant to individual patient-members, self-rationing care in American will continue and, ironically, lead to greater spending in the long run with people putting off necessary tests, prescription drugs, and preventive care. With the emergence of six-to-seven figure specialty drugs coming out of the Rx pipeline into commerce, we can expect growing financial toxicity as a side effect of these therapies, and evolving financial services offered to patients to pay, say, on an installment plan as Bluebird Therapeutics has offered (specifically, $1.78 mm over five years). In 1971, Céline published his book, Death on the Installment Plan; one wonders what Louis-Ferdinand would have thought about this medical billing model.
 Tech Scaling a Big Embrace of Social Determinants. With greater recognition of the role of social determinants of health (SDoH), providers, payors and employers will scale solutions for nutrition and food security, transportation, and even loneliness using technology platforms and data mash-ups to determine who-needs-what, when. For example, Papa provides “Grandkids on Demand” matching college students for high-touch visits with older people in the community to address loneliness among people aging-in-place at home. For these folks, innovations in home sensor technology and Internet of Things for health and medicine will build their evidence case, with voice-tech fast-growing for these applications.
Tech Scaling a Big Embrace of Social Determinants. With greater recognition of the role of social determinants of health (SDoH), providers, payors and employers will scale solutions for nutrition and food security, transportation, and even loneliness using technology platforms and data mash-ups to determine who-needs-what, when. For example, Papa provides “Grandkids on Demand” matching college students for high-touch visits with older people in the community to address loneliness among people aging-in-place at home. For these folks, innovations in home sensor technology and Internet of Things for health and medicine will build their evidence case, with voice-tech fast-growing for these applications.
 The Retail Health Landscape Will Broaden and Deepen. With consumers as patient-payors, peoples’ preferences will largely be to stay-the-heck-away from healthcare’s Pill Hill, bricks-and-mortar places with expensive parking and long waits in ante-rooms. Telehealth is becoming just a normal part of medical service delivery, fast-growing for mental and behavioral health, DTC prescriptions for women’s and men’s health (looking at the trajectory of Ro, Hims and Hers), employers’ sponsorship of telehealth visits, and niched virtual health services. Retail health in the form of grocery stores and chain pharmacy had long defined this space. In 2020, with the likes of payors and health plans getting into the retail health segment, we’ll see CVS continue to integrate the acquisition of Aetna into the company’s product and service portfolio. In the new year, we’ll watch for Cigna, Humana and UnitedHealthcare to integrate vertically and/or horizontally to activate consumers in their health. Furthermore, we’ll see health care real estate deals using retail spaces in new ways for healthcare and self-service wellness close to people in their communities. And, I’m especially happy that the new YMCA in Louisville cut their ribbon on December 18th after more than a decade in the planning, bringing together the Y with an elementary school, a bank, a fresh food store, cardiac rehab, bolstering economic development in the Broadway section of town. This project is a model for physical, financial, and community health that will inspire other communities.
The Retail Health Landscape Will Broaden and Deepen. With consumers as patient-payors, peoples’ preferences will largely be to stay-the-heck-away from healthcare’s Pill Hill, bricks-and-mortar places with expensive parking and long waits in ante-rooms. Telehealth is becoming just a normal part of medical service delivery, fast-growing for mental and behavioral health, DTC prescriptions for women’s and men’s health (looking at the trajectory of Ro, Hims and Hers), employers’ sponsorship of telehealth visits, and niched virtual health services. Retail health in the form of grocery stores and chain pharmacy had long defined this space. In 2020, with the likes of payors and health plans getting into the retail health segment, we’ll see CVS continue to integrate the acquisition of Aetna into the company’s product and service portfolio. In the new year, we’ll watch for Cigna, Humana and UnitedHealthcare to integrate vertically and/or horizontally to activate consumers in their health. Furthermore, we’ll see health care real estate deals using retail spaces in new ways for healthcare and self-service wellness close to people in their communities. And, I’m especially happy that the new YMCA in Louisville cut their ribbon on December 18th after more than a decade in the planning, bringing together the Y with an elementary school, a bank, a fresh food store, cardiac rehab, bolstering economic development in the Broadway section of town. This project is a model for physical, financial, and community health that will inspire other communities.
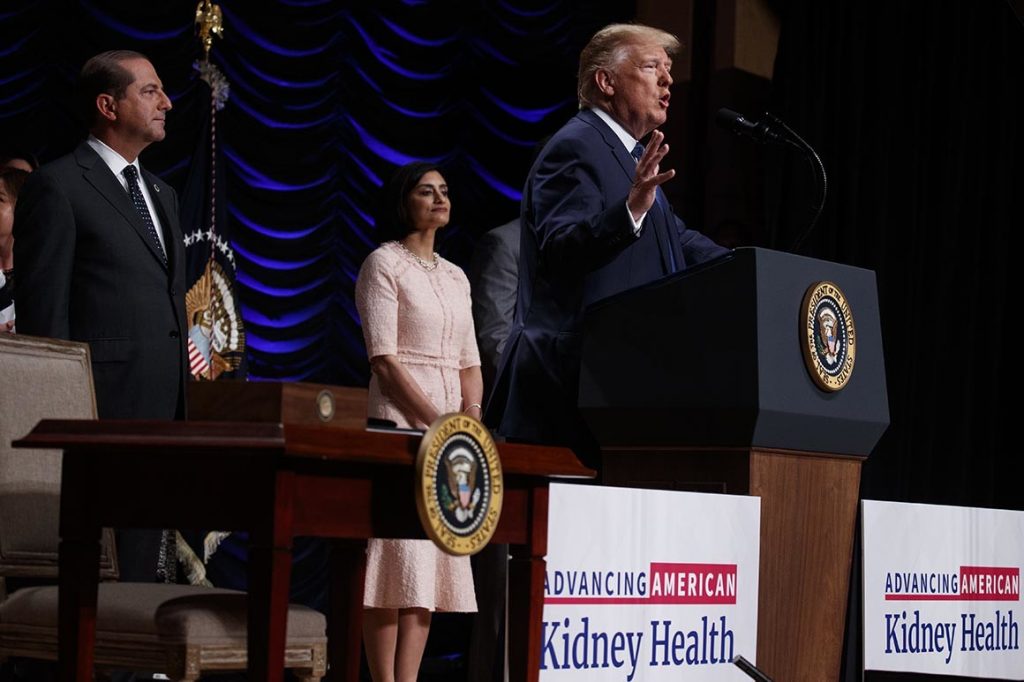 Health Politics, Policy and the President. The biggest known-unknown for 2020 is politics on the macro/national U.S. level, and then the tighter lens on health politics and health policy. We were fairly certain in last year’s Health Populi TrendCast that prescription drug pricing would get dealt with – after all, as Donald Trump was unpacking his Oval Office desktop bric-a-brac, TIME magazine’s Person of the Year told the magazine, ““I’m going to bring down drug prices,” further damning the industry by saying that, “pharma is getting away with murder” based on the pricing of medicines. The House passed its prescription drug bill earlier this month, named the Elijah E. Cummings Lower Drug Costs Now Act, including provisions for the Federal government to negotiate prices with Medicare, use reference pricing for drugs based on other nations, limit out-of-pocket costs for Medicare enrollees, and prevent dramatic drug price hikes. This legislation passed with universal votes from Democrats plus two Republicans. However, inside the White House, broader health policy harmony is compromised by a quite-public arm-wrestle between Alex Azar, the Secretary of Health and Human Services, vis-à-vis CMS Administrator Seema Verma.
Health Politics, Policy and the President. The biggest known-unknown for 2020 is politics on the macro/national U.S. level, and then the tighter lens on health politics and health policy. We were fairly certain in last year’s Health Populi TrendCast that prescription drug pricing would get dealt with – after all, as Donald Trump was unpacking his Oval Office desktop bric-a-brac, TIME magazine’s Person of the Year told the magazine, ““I’m going to bring down drug prices,” further damning the industry by saying that, “pharma is getting away with murder” based on the pricing of medicines. The House passed its prescription drug bill earlier this month, named the Elijah E. Cummings Lower Drug Costs Now Act, including provisions for the Federal government to negotiate prices with Medicare, use reference pricing for drugs based on other nations, limit out-of-pocket costs for Medicare enrollees, and prevent dramatic drug price hikes. This legislation passed with universal votes from Democrats plus two Republicans. However, inside the White House, broader health policy harmony is compromised by a quite-public arm-wrestle between Alex Azar, the Secretary of Health and Human Services, vis-à-vis CMS Administrator Seema Verma.
So at a Federal level, the two most key leaders for health policy aren’t in harmony as we start the new year. This is why in PwC’s forecast for 2020, they expect that “regulation will trump policy.” I agree.
The biggest wild card for 2020 in health/care will be a privacy breach impacting one of the Big Tech companies. Will this result in a mass call for privacy regulation that goes beyond the fragmented approach we currently “enjoy” in the U.S. which prevents Americans from full-on health citizenship?
Will Big Tech get caught out on this? We’re monitoring EU regulators who have been pretty tough on Big Tech in Europe with respect to the GDPR and growing concern for tech companies’ access to data. The NHS in England has been criticized for its handling of patient data in concert with Google’s Deep Mind. California’s privacy legislation, the CCPA, goes live on 1 January 2020. Will this inspire other states to promulgate similar, tough privacy laws protecting their states’ residents?
On a personal note…I end 2019 with a lot of blessings in my life – love of family and friends, personal health, a job for which I’m so grateful and gratified, and the sale of our family home now living in a downsized, “Marie Kondo’d” streamlined lifestyle.
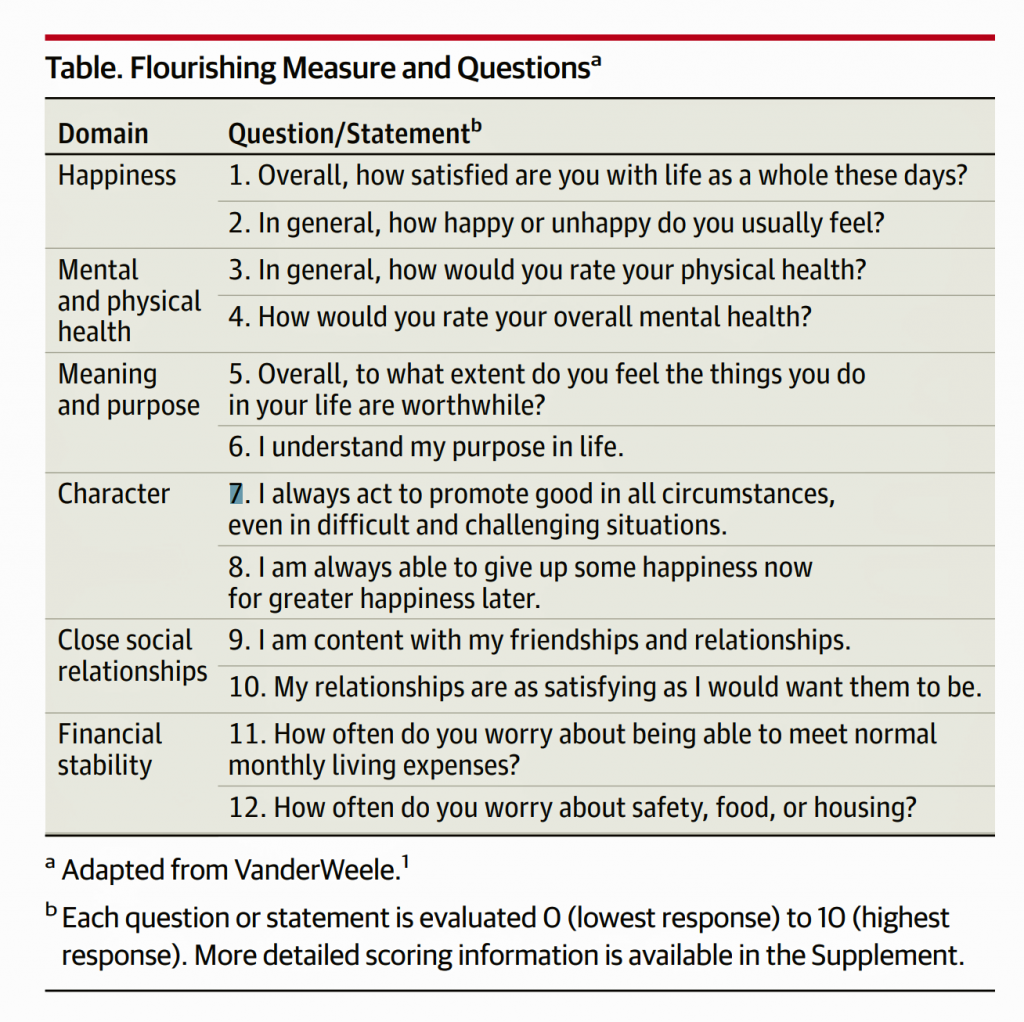 I am currently inspired for 2020 pondering two recent JAMA essays, “Health: Flourishing” and “Health as a way of doing business.”
I am currently inspired for 2020 pondering two recent JAMA essays, “Health: Flourishing” and “Health as a way of doing business.”
In the former, I quote: A patient care not only about physical health and test results “within normal limits” but also more broadly about being happy, having meaning and purpose, being “a good person,” and having fulfilling relationships.
From the latter, note that, “In short, global dynamics such as market forces, rising societal expectations, and innovative long-term strategies are pushing companies to consider social effects, including health, as a way of doing business. Such efforts are in their early stages, however, and many remain skeptical that business, historically blamed for a range of health problems, can ever contribute to solutions. Only further global debate, innovation, and evaluation can determine how the private sector can best improve public well-being and offer new directions for the future of population health.”
In 2020, I expect a trend we saw emerge in 2019 continue in this new year: that “public health” functions will grow in the private sector as the public sector continues to be challenged by political divisions, divisiveness, and incivility.
I wish you all a joyous and blessed holiday season, and healthy, peaceful and inspired 2020…with clear vision, loving hearts, and plenty of laughter-for-health.




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for