 There’s a gap between the supply of digital health tools that hospitals and health systems offer patients, and what patients-as-consumers need for overall health and wellbeing. This chasm is illustrated in The future of the digital patient experience, the latest report from HIMSS and the Center for Connected Medicine (CCM).
There’s a gap between the supply of digital health tools that hospitals and health systems offer patients, and what patients-as-consumers need for overall health and wellbeing. This chasm is illustrated in The future of the digital patient experience, the latest report from HIMSS and the Center for Connected Medicine (CCM).
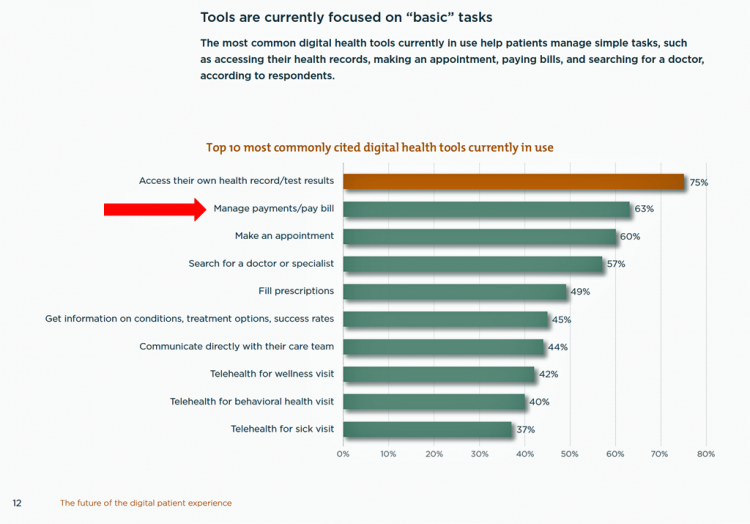
The big gap in supply to patients vs. demand by health consumers is highlighted by what the arrow in the chart below points to: managing payments and paying bills. Nowhere in the top 10 most commonly provided digital tools is one for price transparency, cost comparing or cost estimating.
In the top 10 most commonly cited digital health tools in use, this payment-bill pay tool ranks second on the supply side, following patient portals (described here as “access their own health record/test results), and ahead of making an appointment, searching for a physician, filling prescriptions, and getting information, among other “basic tasks,” as HIMSS/CCM classifies the list of 10.
 The key findings in the survey of 136 health care executives were that:
The key findings in the survey of 136 health care executives were that:
- Digital health tools are a priority for half of the health system leaders
- Only 1 in 3 felt their consumer digital experience was considered “the best possible”
- Patient-facing digital tools help patients with fairly basic tasks like making appointments, seeking doctors, and paying bills
- Motivations for expanding digital tools for patients are to enhance access to care, empowering patients to monitor and manage their health, and deliver greater patient satisfaction
- Key challenges to adopting digital health tools are first and foremost cost, following by interoperability and operational barriers.
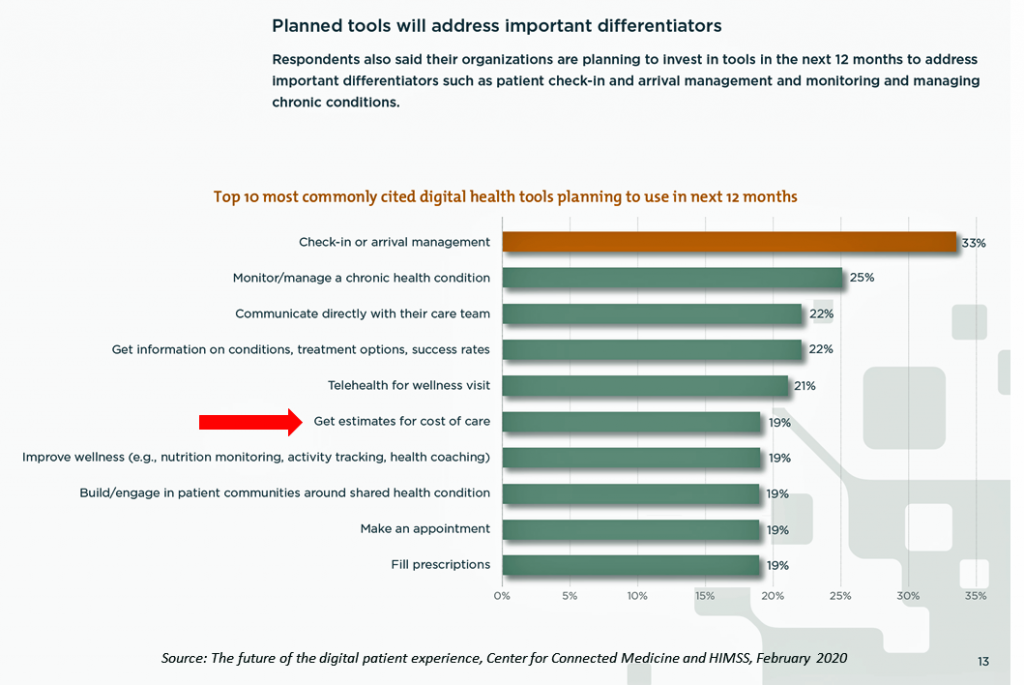
Check out the second bar chart which illustrates the top 10 tools planned by health systems to offer patients and consumers. Only 1 in 5 health systems plans to offer a tool to help patients-consumers “get estimates for costs of care.”
 Yet it’s health care costs that rank top in U.S. health citizens’ minds in 2020 leading up to the election.
Yet it’s health care costs that rank top in U.S. health citizens’ minds in 2020 leading up to the election.
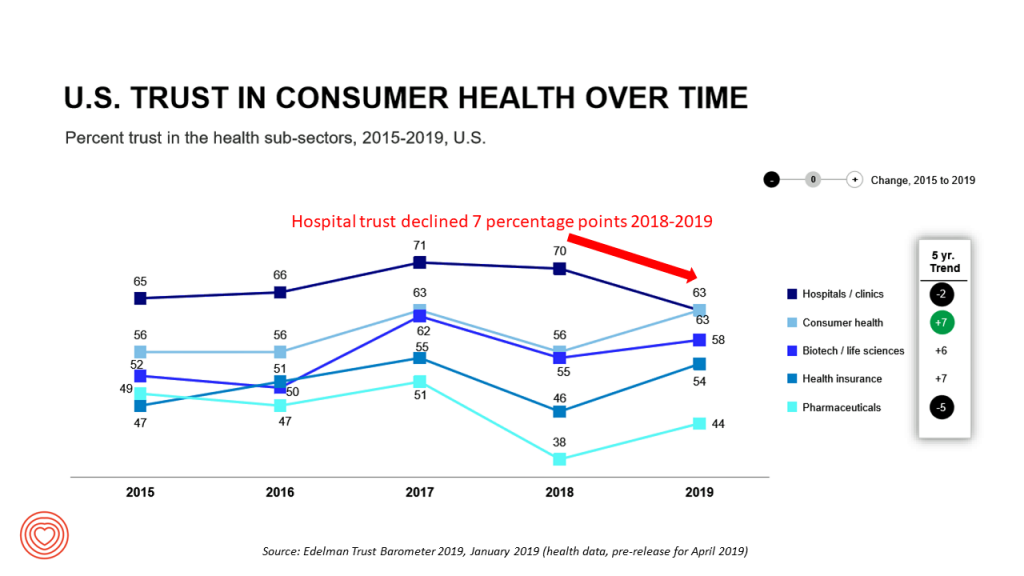
And note how Americans’ trust in hospitals — historically the top-trusted health care segment in the nation — eroded from 2018, tying with consumer health companies, and just north of biotech and life science organizations.
Even trust with pharmaceutical companies increased that year.
Health Populi’s Hot Points: The HIMSS-CCM research focused on “digital patient experience.”
 The financial experience is part of, integrated into, the patient-as-consumer’s health care experience today. The patient has morphed into the payor, as the first chapter of my book, HealthConsuming, attests. As such, financial wellness is bound up in overall health and wellness.
The financial experience is part of, integrated into, the patient-as-consumer’s health care experience today. The patient has morphed into the payor, as the first chapter of my book, HealthConsuming, attests. As such, financial wellness is bound up in overall health and wellness.
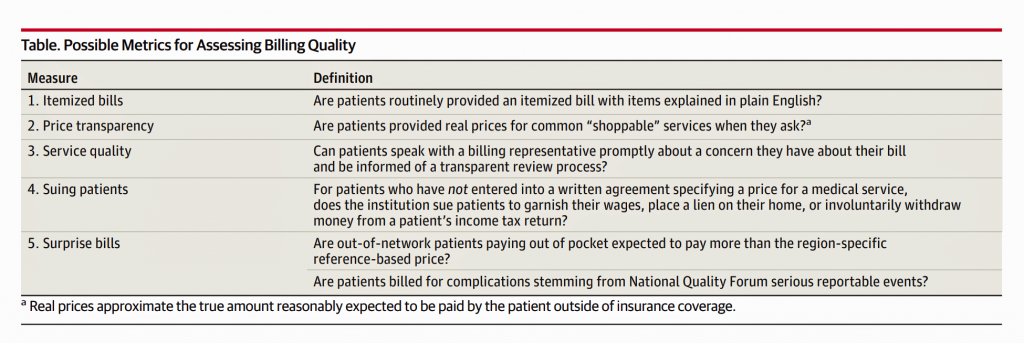
An essay in the 4th February 2020 JAMA, Billing Quality is Medical Quality, attests that, “the financial harm of medical care should not be separated from the clinical consequences of care, because both outcomes can have a major influence on the health and well-being of patients.” This sage insight was written by Dr. Martin Makary and Dr. Simon Mathews of Johns Hopkins; Dr. Makary’s book, The Price We Pay, speaks to the relatively low ROI Americans get for their health care spending and how to fix the system. The fourth table comes from the JAMA viewpoint, serving up measurements that address “billing quality.”
All five of these issues have contributed to patients-as-consumers beginning to diss hospitals and the entire inpatient sector — lawsuits against patients and their families, surprise bills, lack of pricing transparency, et. al.
Hospitals are already losing patients to alternative sites when there are choices to be had in a local market. Prioritizing the digital health experience, with financial health baked into the front-end and not just the back-end bill payment and ex post facto EOB from the health plan will help reverse this era of eroding trust between patient and hospital.




 Thank you FeedSpot for
Thank you FeedSpot for