Everyday factors can make a big difference in a person’s current and future health risks and needs, we’re learning in the COVID-19 pandemic, detailed in 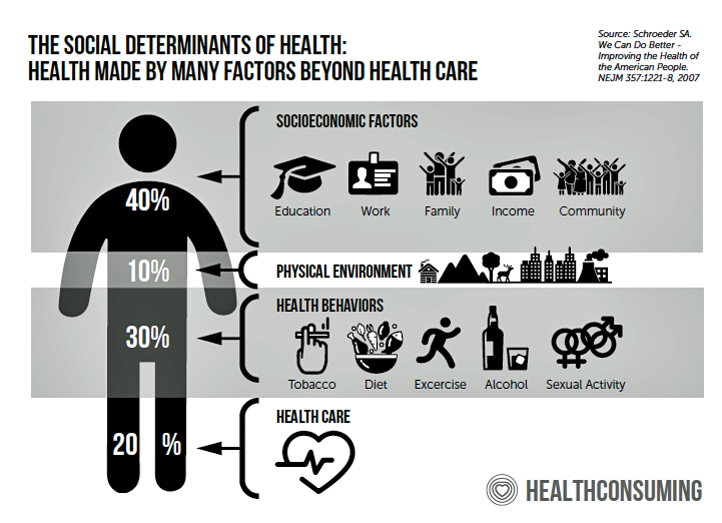 a new Welltok research report, Social Determinants of Health Matter: Voice of the Consumer.
a new Welltok research report, Social Determinants of Health Matter: Voice of the Consumer.
“The current public health crisis underscores the importance of leveraging SDOH as a way to effectively provide timely, relevant support that is truly going to make a difference for people’s total wellbeing,” Bob Fabbio, Welltok’s CEO, explained in a press release. “It’s not only about predicting high-risk individuals, but also those that may be feeling isolated, financially insecure or emotionally unstable that need help. People are lost and looking for personalized support and information from organizations they trust,” which provided context for company’s report.
For definition, the first graphic comes out of my book, HealthConsuming: From Health Consumer to Health Citizen, from chapter 7: “ZIP Codes, Genetic Codes, Food and Health.”
This part of HealthConsuming delves into the impacts of each of our every day lives, environments, personal choices and socioeconomic factors that shape our health and well-being even more than our genetic endowment at-birth does.
 Welltok explored U.S. adults’ perspectives on social determinants, first finding that most people under-estimate the impacts of SDoH factors on health status.
Welltok explored U.S. adults’ perspectives on social determinants, first finding that most people under-estimate the impacts of SDoH factors on health status.
Consumers estimated that lifestyle and environment contributed roughly one-half to health, versus the 80% shown in the foundational research — a large over-estimate on the power of medical care and our inherent genetic make-up.
Welltok then found that people under-estimate specific daily life-flows that can negatively erode health and well-being, like the length of time one commutes to a job, or social connections that bolster feelings of belonging in a community. (FYI loneliness has been found to be at least as harmful to health as smoking a pack of cigarettes — discussed here in Health Populi, and in this terrific essay in Scientific American].
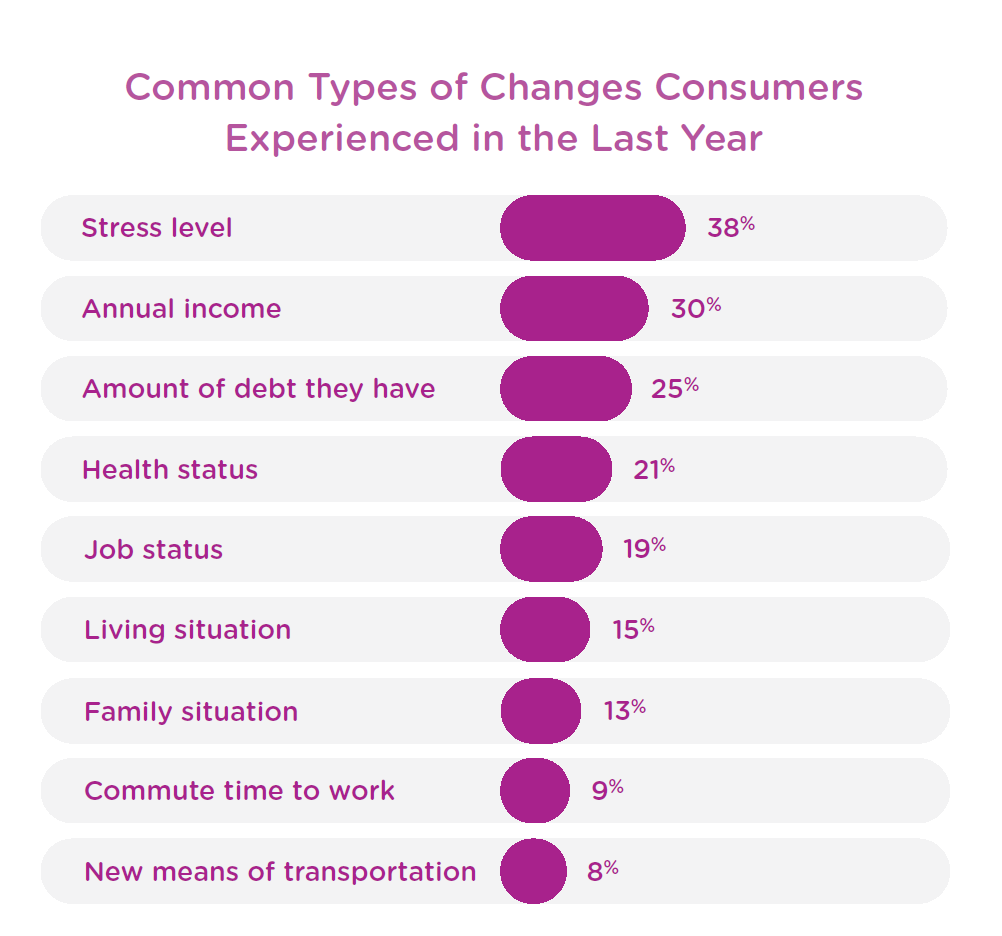
In the past year, Americans have felt increasing stress, financial concerns and growing debt, job changes, and other stressors that impact health.
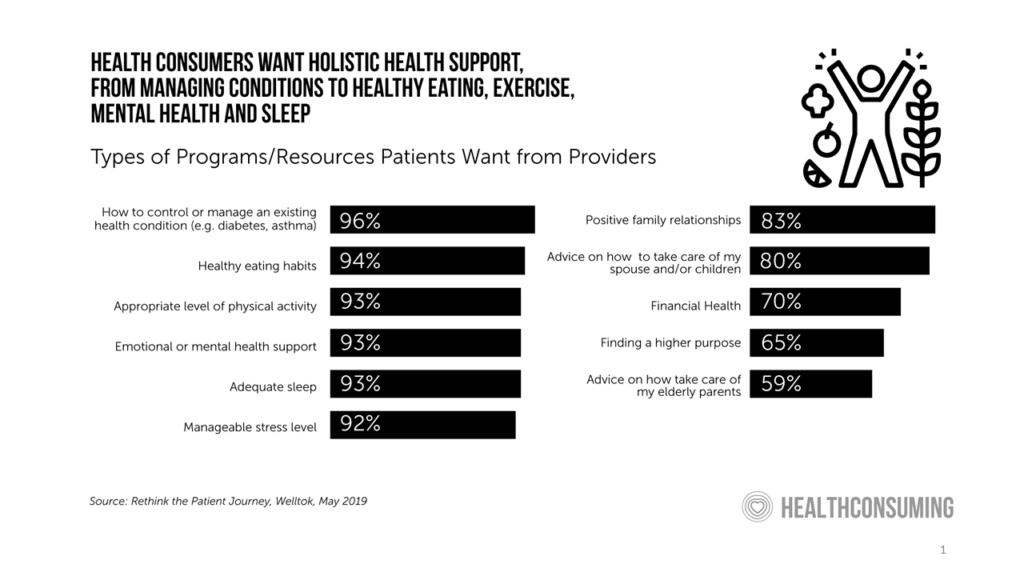 Welltok points out that patients-as-health consumers increasingly recognize the connections between financial, mental/emotional and social health on physical health, seeking support across all of these dimensions. This bar chart comes from a Welltok study published last year on the kind of support health consumers seek across their life-flows, from sleep and exercise to stress and financial management.
Welltok points out that patients-as-health consumers increasingly recognize the connections between financial, mental/emotional and social health on physical health, seeking support across all of these dimensions. This bar chart comes from a Welltok study published last year on the kind of support health consumers seek across their life-flows, from sleep and exercise to stress and financial management.
Interviews for the SDoH study were conducted among 2,000 U.S. adults in January 2020, just before the COVID-19 pandemic emerged in media reports.
 Health Populi’s Hot Points: We’re all now living in the current COVID-19 pandemic era, a great leveler across all socioeconomic strata. The pandemic has also made the world “flat,” spanning our fellow and sister health citizens across the globe, albeit in different time zones and seasons.
Health Populi’s Hot Points: We’re all now living in the current COVID-19 pandemic era, a great leveler across all socioeconomic strata. The pandemic has also made the world “flat,” spanning our fellow and sister health citizens across the globe, albeit in different time zones and seasons.
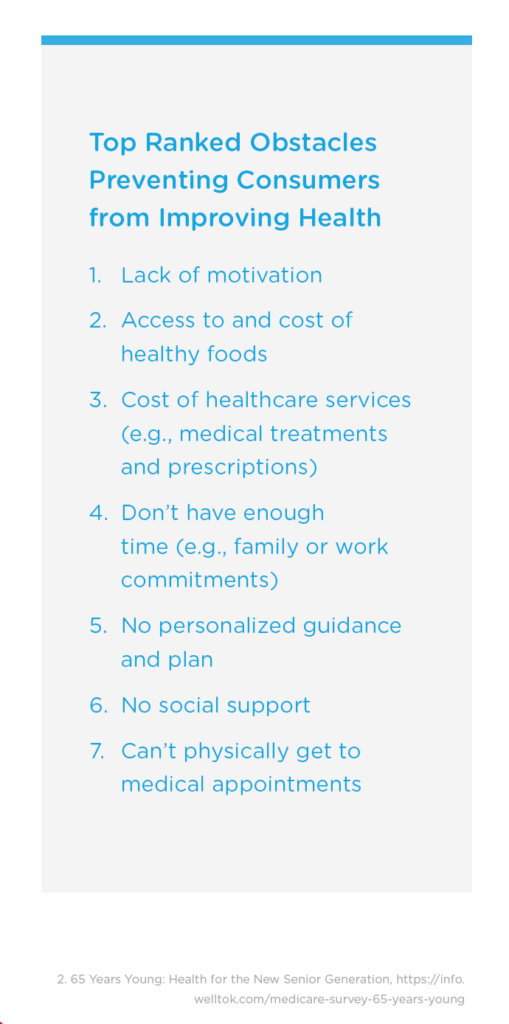
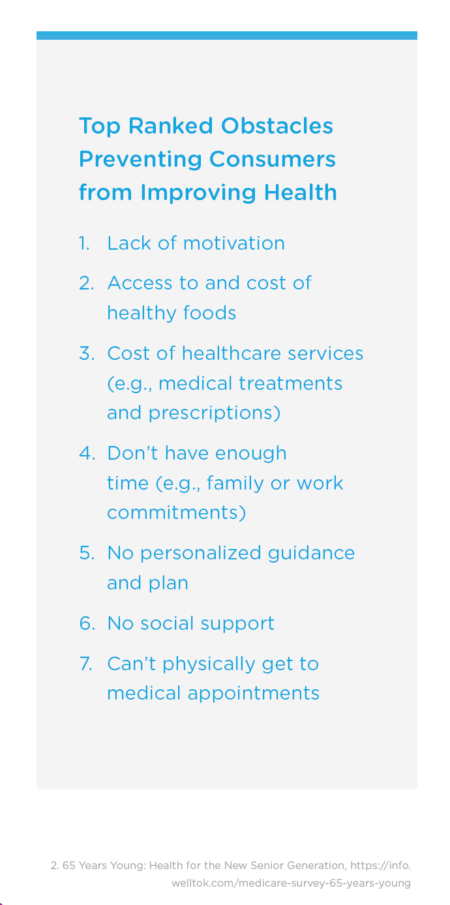
In the U.S., Welltok identified some big obstacles keeping us from improving our health, shown in the blue list. Lack of motivation, access to and cost of healthy foods, and the cost of healthcare services ranked in the top 3 barriers to making our health.
In the COVID-19 pandemic, these 3 barriers are even more challenging as millions of people have lost jobs (and as a result, many losing health insurance), feeling discombobulated in the #StayHome era (whether working at home or not), and of course, challenged to eat healthily without open access to grocery stores. Furthermore, the rate of exercise is down, exacerbating healthy lifestyles we might have lived out before the coronavirus disrupted our normal daily flows.
Welltok recommends that health care ecosystem leaders — health plans, providers, pharma and other organizations — collaborate and leverage SDoH data to identify people at-risk for factors that erode health and, in the COVID-19 pandemic, place patients in harm’s way of the virus.
Technology platforms can help communicate and “meet” with patients where they live — via phones (whether smartphones or texting ones) and broadband networks, connecting people with local community resources and care.
The COVID-19 pandemic reminds us the power of connectivity, data, and empathy. While it’s painful in real-time in so many ways, we have the opportunity to come out of the pandemic with the learnings that inform and motivate us to make health care delivery, financing and engagement so much more human, humane, effective and collaborative.




 Jane will deliver the keynote address at the upcoming
Jane will deliver the keynote address at the upcoming  Thank you, Jared Johnson, for including me on the list of the
Thank you, Jared Johnson, for including me on the list of the  I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,