Within days of the coronavirus pandemic emerging in the U.S., health care providers set up virtual care arrangements to convene with patients. Three months into the COVID-19 crisis, how have patients felt about these telehealth visits?
In Patient Perspectives on Virtual Care, Kyruus answers this question based on an online survey of 1,000 patients 18 years of age and older, conducted in May 2020. Each of these health consumers had at least one virtual care visit between February and May 2020.
The key findings were that:
- Engaging in a virtual visit was a new-new thing for 72% of people
- Patients’ experiences with virtual care were generally positive, with over 75% of consumers reporting being very or completely satisfied
- 3 in 4 consumers expect virtual care as an option for their own health care, believing that providers should scale telehealth as part of an overall portfolio of visit types in the future.
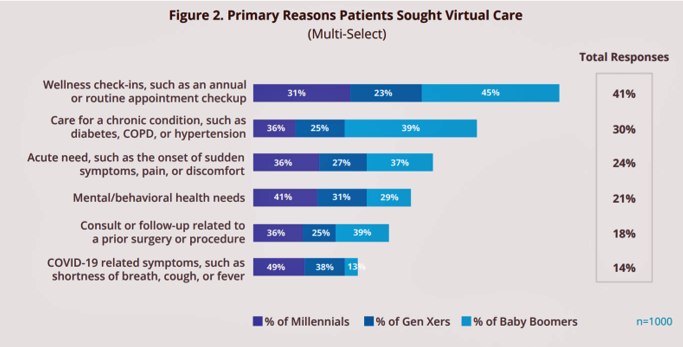 The top reasons health consumers sought virtual care were for wellness check-ins and routine check-ups, among 41% of virtual care consumers. This reason for seeking telehealth was particularly popular among Baby Boomers, 45% of whom south virtual care for a wellness visit or check-up. More Boomers were likely to seek virtual care across all categories surveyed except for mental/behavioral health, most commonly sought by Millennials at a rate of two-to-one compared with the general adult population (41% versus 21% overall).
The top reasons health consumers sought virtual care were for wellness check-ins and routine check-ups, among 41% of virtual care consumers. This reason for seeking telehealth was particularly popular among Baby Boomers, 45% of whom south virtual care for a wellness visit or check-up. More Boomers were likely to seek virtual care across all categories surveyed except for mental/behavioral health, most commonly sought by Millennials at a rate of two-to-one compared with the general adult population (41% versus 21% overall).
Thirty percent of people sough virtual care for dealing with a chronic condition (e.g., COPD, diabetes, hypertension), 24% for an acute need like pain, and 21% for mental/behavioral health needs.
14% of consumers sought virtual care to address COVID-19 symptoms such as cough, fever, or shortness of breath.
Over one-half of consumers learned about virtual care options through an online search like Google or Bing (“Calling Dr. Google!”), and another one-third through a patient portal, hospital system, or urgent care website. One-quarter of people found virtual care info via an insurance company site or third-party channel like ZocDoc.
To arrange care, most patients did so through their health care providers: 58% overall, and 73% Boomers. Younger people were more likely to use other sources to organize virtual care. Regardless of channel to organize care, the vast majority of people found doing so easy to organize. Only 4% four it “somewhat difficult.”
 Most consumers of virtual care also found their insurance covered or would cover all of the cost: 56% among commercial payors and 68% of public payors said their visit was totally covered. 32% of people covered by commercial insurance found the plan to cover “some” of the cost, compared with 18% of those on a public plan.
Most consumers of virtual care also found their insurance covered or would cover all of the cost: 56% among commercial payors and 68% of public payors said their visit was totally covered. 32% of people covered by commercial insurance found the plan to cover “some” of the cost, compared with 18% of those on a public plan.
Most consumers of virtual care in the first months of the pandemic were satisfied with their visits, including 77% of Boomers, 69% of Millennials, and 89% of Gen Xers. Key satisfaction drivers have been convenience, safety of having care at home, and speed of access. As a sign of satisfaction, 70% of consumers would be likely (very or extremely) to recommend virtual care to friends or colleagues.
 Among satisfaction deflectors were perceived quality of care, an impersonal experience, and technical issues.
Among satisfaction deflectors were perceived quality of care, an impersonal experience, and technical issues.
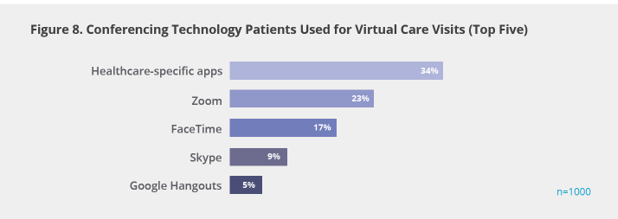
Regarding technology, it’s interesting to look at Figure 8 from the report, showing that only 34% of consumers in the study accessed healthcare specific apps for their virtual care visit such as Amwell and Teladoc, both of which fast-scaled by early March. Commercial conferencing platforms like Zoom (23%), Facetime (17%), and Skype (9%) were also stood up by clinicians touching base with patients for telehealth encounters.
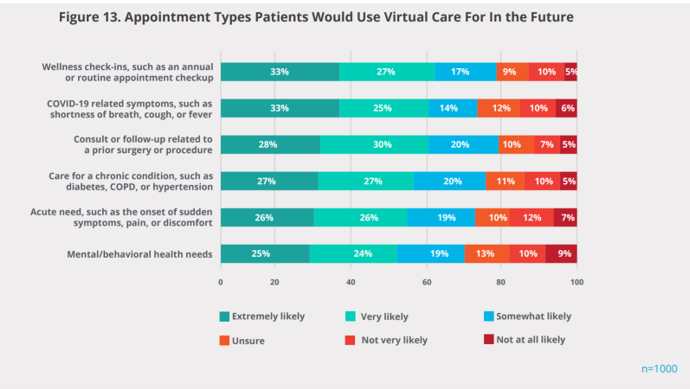 Going forward, based on overall satisfaction with their virtual visit during the pandemic, most consumers expect virtual care in their personal portfolio of health care service options.
Going forward, based on overall satisfaction with their virtual visit during the pandemic, most consumers expect virtual care in their personal portfolio of health care service options.
Most people who had had a virtual visit during the early pandemic era would welcome telehealth across a range of medical needs, from wellness and routine check-ups to caring for a chronic condition and following up a surgical procedure.
One-half of consumers would also be very or extremely likely to use mental and behavioral health services via virtual platforms in the future.
Kyruus concludes the survey report noting the opportunity to improve care coordination and drive patient retention by “closing the loop” through building processes that keep patients in the medical family — that is, the health system’s provider network.
 Health Populi’s Hot Points: The Kyruus study spoke to the “demand side” of telehealth — the patient’s point of view. What about physicians? Are they as enthusiastic about supplying virtual care to their patients once COVID cools and physicians get back to some sort of “normal?”
Health Populi’s Hot Points: The Kyruus study spoke to the “demand side” of telehealth — the patient’s point of view. What about physicians? Are they as enthusiastic about supplying virtual care to their patients once COVID cools and physicians get back to some sort of “normal?”
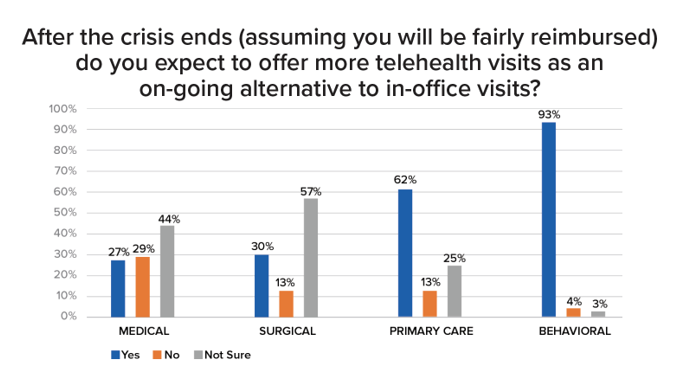
A new study from Sage Growth Partners and Black Book Research demonstrates some ambivalence among physicians — especially among medical and surgical doctors. The most bullish clinicians about providing telehealth visits as an on-going alternative to in-office visits are behavioral/mental health providers and primary care physicians, 93% and 62% of whom expect to provide more telehealth to patients. Note that the survey question SGP asked assumed physicians would be ‘fairly reimbursed,’ so payment was taken out of this question as a potential barrier to providing virtual care.
Earlier in the SGP report, physicians listed key problems with telehealth, which included privacy (explaining policies to patients), cybersecurity risks, lack of data for care continuity, patient literacy with digital technology, and to be sure, reimbursement and payment parity, among other challenges.
The bullish forecasts we now read in analysts’ reports must be tempered with the doctors’ and other providers’ points-of-view. Virtual care has indeed been a boon and gift in the COVID-19 pandemic to scale care and provide access to patients in their quarantine and risk-management journeys. Physicians, too, benefited from some work-flow and encounters to help financial buoy medical practices and serve up care to their patients. But privacy, security, pricing, and regulatory challenges must be ironed out if telehealth is to scale everywhere it needs to be to benefit U.S. health citizens and their providers.




 Thank you FeedSpot for
Thank you FeedSpot for