The median charge for hospitalizing a patient with COVID-19 ranged from $34,662 for people 23 to 30, and $45,683 for people between 51 and 60 years of age, according to FAIR Health’s research brief, Key Characteristics of COVID-19 Patients published July 14th, 2020.
FAIR Health based these numbers on private insurance claims associated with COVID-19 diagnoses, evaluating patient demographics (age, gender, geography), hospital charges and estimated allowed amounts, and patient comorbidities. They used two ICD-10-CM diagnostic codes for this research: U07.1, 2019-nCoV acute respiratory disease; and, B97.29, other coronavirus as the cause of disease classified elsewhere which was the original code used until March 18, 2020, when the specific coronavirus code was implemented.
Charges and estimated allowed amounts were calculated from private insurance claims filed in January through May 2020.
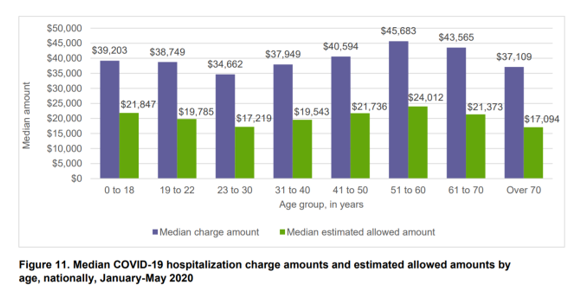 The charge estimates are shown in the first bar chart, published in the study. The blue bars are the median charges for each age cohort, billed by the patient’s hospital, Note that younger peoples’ charges from child to 18 years of age were roughly the same charges as for people in other age cohorts and, in fact, higher than those charged for people over 70 years of age. The highest charges came from patients age 51 to 60 years of age.
The charge estimates are shown in the first bar chart, published in the study. The blue bars are the median charges for each age cohort, billed by the patient’s hospital, Note that younger peoples’ charges from child to 18 years of age were roughly the same charges as for people in other age cohorts and, in fact, higher than those charged for people over 70 years of age. The highest charges came from patients age 51 to 60 years of age.
Estimated allowed charges by health plans were much lower than the original charge amounts, ranging from $17K at the low end to $24K for that 51 to 60 year old age group. The higher median charge amount was the amount charged to a patient who was uninsured or getting care out-of-network.
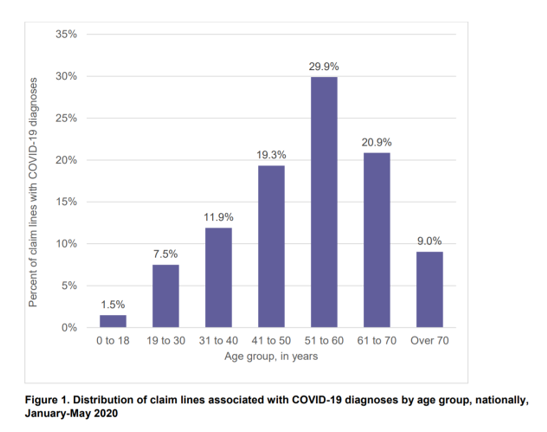
The second chart shows COVID-19 claim lines (that is, patient case claims in private plans) by age groups for the overall U.S. Note that the age group 51-60 saw the most cases, followed by 61-70 year olds.
The first chart exhibited that the highest charges for coronavirus hospital admissions were generated among those 51 to 60. Thus, this age group generated the greatest charges in aggregate compared with all others, given that this cohort is the largest group associated with the highest costs.
Remember that this study focused on commercially insured patients, so it makes sense that the claim percentage for patients over 70 years of age would be smaller — with peers in the age group likely covered by people covered by Medicare Parts A, B, and D, and those in Medicaid plans, CHIP, and state and local government programs.
In the third chart, see “where” the study’s COVID-19 patients were diagnosed for the disease by venue. One-third of patients of coronavirus patients were diagnosed in a physician’s office, 23% in the inpatient setting, 11% in an outpatient clinic, 7% in the emergency department, and 6% through telehealth. One in five were diagnosed somewhere else.
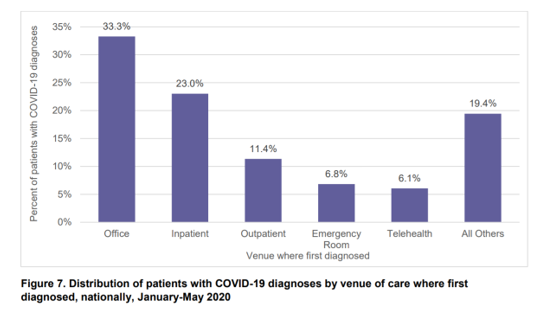 FAIR health concludes in the report that, “there is no one profile of COVID-19 patients.” COVID patients, as shown above, represent all ages, and live in rural and urban areas. They receive diagnoses across a range of care settings, and have diverse comorbidities, such as kidney disease, Type 2 diabetes, hypertension, heart failure, sleep disorders, COPD, among other conditions.
FAIR health concludes in the report that, “there is no one profile of COVID-19 patients.” COVID patients, as shown above, represent all ages, and live in rural and urban areas. They receive diagnoses across a range of care settings, and have diverse comorbidities, such as kidney disease, Type 2 diabetes, hypertension, heart failure, sleep disorders, COPD, among other conditions.
Health Populi’s Hot Points: FAIR Health is a nonprofit organization whose mission is to support and drive transparency into healthcare for cost and health insurance information. This study was based on data shared by more than 60 payors and third-party administrators who insure, or process claims for private health plans covering over 150 million members — about 75% of U.S. privately-insured people.
This dataset showed that costs for hospital care for a COVID-19 patient can reach as high as $45,000 for someone in their 50s who may be uninsured or getting care out-of-network.
 Yesterday’s Health Populi featured a post speaking to what I termed, “the toxic side-effect of COVID-19: financial unwellness,” discussing the 2020 financial wellness “census” from Prudential.
Yesterday’s Health Populi featured a post speaking to what I termed, “the toxic side-effect of COVID-19: financial unwellness,” discussing the 2020 financial wellness “census” from Prudential.
In that study, Prudential focused more on the economic impacts on Americans due to the Great Lockdown and subsequent job losses, reduced hours on jobs, or furloughs from work — not so much on health care costs.
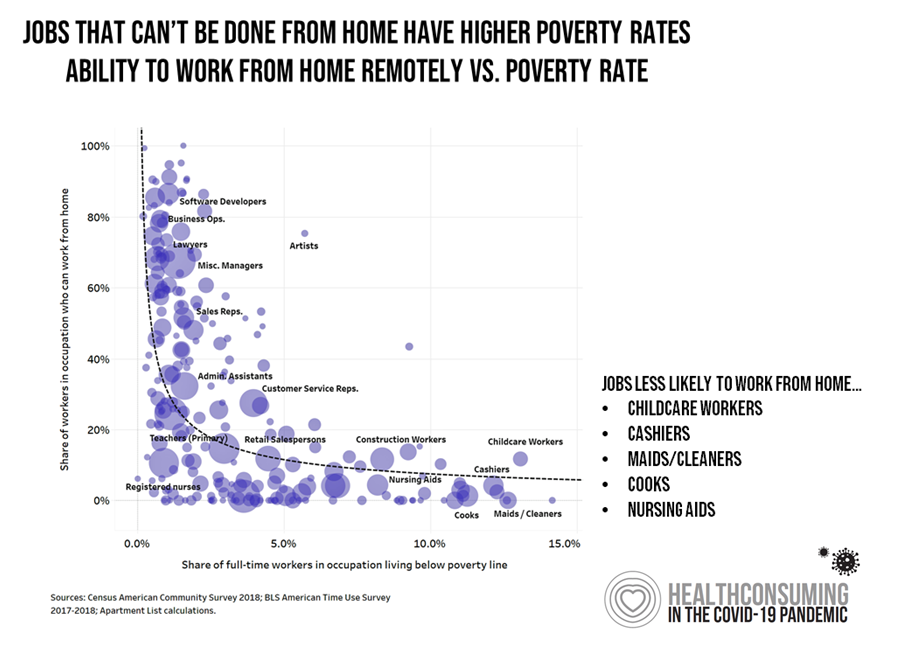
In the shelter-in-place phase of the pandemic, not every worker could work from home: in fact, jobs less likely to be able to work from home included some of the lowest-paid jobs in America, such as childcare workers, retail cashiers, maids and cleaners, cooks, and nursing aids, shown in the chart which demonstrates that jobs that can’t be done through home/telework have higher poverty rates.
This circular situation — that people who earn less money are less likely to be able to work from home, also combines with job loss and the loss of health insurance — that is, if these jobs’ employers had even offered health plans to workers, which is highly unlikely.
There is an obvious lesson here on the interplay between social determinants of health in the COVID-19 era — making lower-income people, largely people of color, more likely to die from the disease. But we must also connect the dots between the costs of coronavirus care and people who are uninsured who cannot afford to pay a hospital $45,000 at discharge.
Even if that patient did not survive her hospital stay.




 Thank you FeedSpot for
Thank you FeedSpot for