The CDC calculated that some 200,000 American lives would be lost to the coronavirus pandemic by Labor Day weekend 2020. Beyond the tragic mortality in the U.S. come morbidity impacts hitting mental health in America, hard.
 And some people are being hit-harder than others, a report from the Centers for Disease Control details.
And some people are being hit-harder than others, a report from the Centers for Disease Control details.
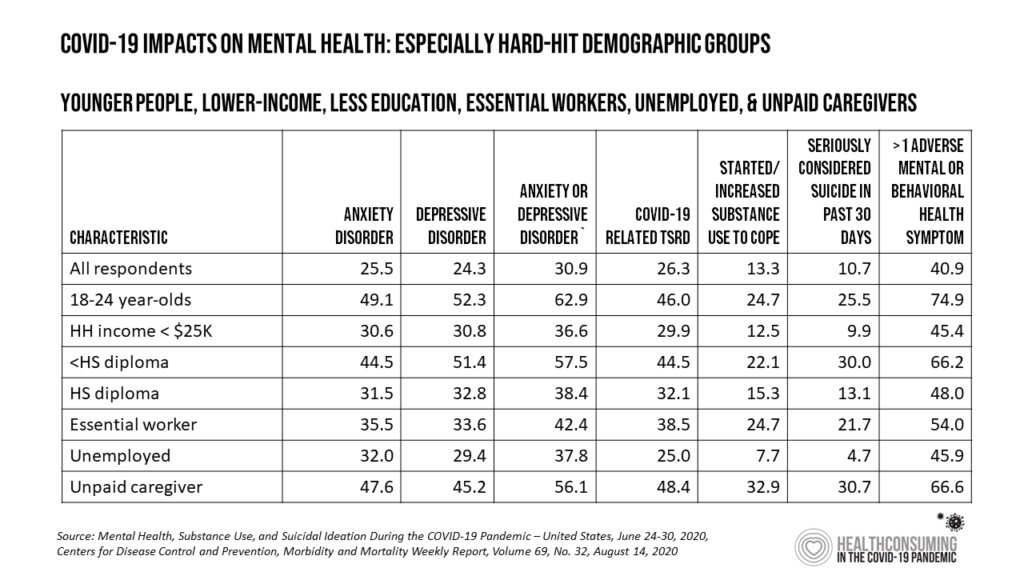
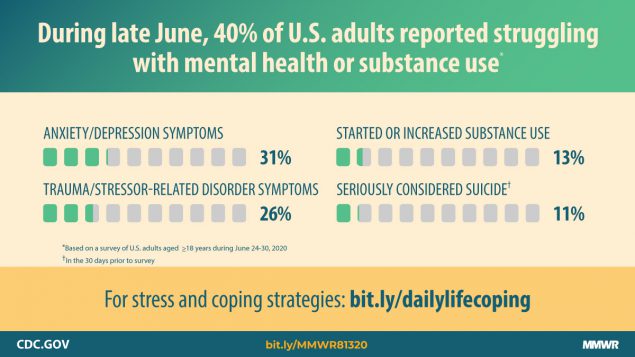
Overall, 4 in 10 people in the U.S. reported at least one adverse mental or behavioral health symptom in the last week of June 2020. These symptoms included anxiety disorder, depressive disorder, COVID-19 related trauma- or stress-related disorder (TSRD), substance use (either starting or increasing), and serious consideration of suicide in the past 30 days.
The table organizes data from the report’s Table 1, calling out those demographic characteristics where people had higher rates of mental/behavioral health impacts.
Those at greater risk for mental health impacts were younger people age 18 to 24 years. people earning lower income, those with less education (people without a high school diploma as well as those with a diploma), essential workers, unemployed people, and unpaid caregivers.
The youngest age cohort of Americans age 18 to 24, and unpaid caregivers, were most likely to have experienced at least one adverse mental or behavioral health symptom.
 THE CDC commissioned the web-based survey during the week of 24 to 30th June 2020, among 5,412 U.S. adults 18 and over. Across all respondents,
THE CDC commissioned the web-based survey during the week of 24 to 30th June 2020, among 5,412 U.S. adults 18 and over. Across all respondents,
- 25.5% reported anxiety
- 24.3% reported depression
- 26.3% reported COVID-19 related trauma- or stress-related disorder (TSRD)
- 13.3% started or increased substance use to cope with the pandemic
- 10.7% seriously considered committing suicide in the past 30 days, and
- 40.9% of people had at least one of these symptoms, shown here in the CDC’s chart.
Among the many demographic traits considered in this study, a unique feature was identifying unpaid caregivers. These people had 3.3 times greater risk for substance use than the overall population, and 3x greater risk of suicidal ideation.
For the entire population, suicidal ideation was twice as high in this study than in 2018 (10.7% versus 4.3%), based on CDC’s previous analysis of the question.
Health Populi’s Hot Points: The pandemic has expanded our vocabulary; now our lexicon must include the acronym “TSRD.” Trauma- and stress-related disorders are described in the Merck Manual as,
“Disorders [involving] exposure to a traumatic or stressful event. Two of the trauma-related disorders are acute stress disorder and post-traumatic stress disorder (PTSD). Acute stress disorder and PTSD are similar except that acute stress disorder typically begins immediately after the trauma and lasts from 3 days to 1 month, whereas PTSD lasts for > 1 month, either as a continuation of acute stress disorder or as a separate occurrence that begins up to 6 months after the trauma.
“Previously, trauma- and stressor-related disorders were considered anxiety disorders. However, they are now considered distinct because many patients do not have anxiety but instead have symptoms of anhedonia or dysphoria, anger, aggression, or dissociation.”
Unpaid caregivers had the greatest risk for COVID-19 related TSRD, with nearly one-half experiencing this adverse mental health symptom. The caregiver demographics come from a subset of data from Archangels’ Caregiver Intensity Index. Archangels, co-founded by Alexandra Drane, is focused on caregivers’ contributions to society and the economy-at-large.
“We believe that caregivers are the backbone of our country, that under-utilized resources exist to support them, and that humans are amazing…and we’re working to knit all that together in the form of impact on lives,” Drane explained the organization’s mission.
Kudos to the study team for incorporating the unpaid caregiver data into this analysis of the mental health pandemic-in-and-beyond-the coronavirus pandemic. These granular data will be hugely important to consider as part of our “post-COVID mental health census” as the U.S. seeks to address the whole-health needs of a nation in pain.




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for