COVID-19 is re-shaping all industries, especially health care. And the pharma industry is challenged along with other health care sectors.
 In fact, the coronavirus crisis impacts on pharma are especially accelerated based on how the pandemic has affected health care providers, as seen through research from Accenture published in Reinventing Relevance: New Models for Pharma Engagement with Healthcare Providers in a COVID-19 World.
In fact, the coronavirus crisis impacts on pharma are especially accelerated based on how the pandemic has affected health care providers, as seen through research from Accenture published in Reinventing Relevance: New Models for Pharma Engagement with Healthcare Providers in a COVID-19 World.
For the study, Accenture surveyed 720 health care providers in general practice, oncology, immunology, and cardiology working in China, France, Japan, the United Kingdom, and the U.S., in May and June 2020.
Top-line, Accenture points to four pillars on which the pharma industry can “reinvent its relevance,” as the report title suggests:
- To express greater empathy, understanding the patient experience of delaying treatment, financial impacts, and mental health challenges the pandemic has caused
- Expanding support services, especially as more care moves into patients’ hands as self-care in the home
- Rethinking messages, as adherence continues to be challenging as people don’t regularly see physicians face-to-face in brick-and-mortar exam rooms
- Creating partnerships that address the new realities of patients taking on care work flows and clinicians going virtual.
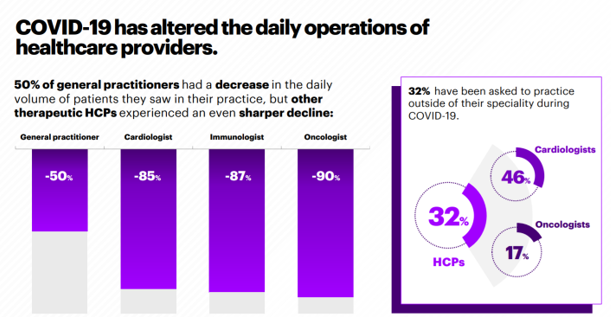 It all started with those health care providers changing work flows due to the emergence of the coronavirus: one-half of GPs saw declines in patient volumes, with specialists experiencing an even greater downturn of visits.
It all started with those health care providers changing work flows due to the emergence of the coronavirus: one-half of GPs saw declines in patient volumes, with specialists experiencing an even greater downturn of visits.
As the bar chart here illustrates, 9 in 10 cardiologists, immunologists, and oncologists saw sharply falling patient volumes.
This new work-flow for clinicians led to fast-adoption of virtual care platforms – telemedicine, tele-conferencing with patients via apps like Zoom and Skype along with commercially-built telehealth channels, and the prescription and use of remote health monitoring devices placed in patients’ homes.
Two-thirds of doctors said they valued tools for remote monitoring more since the pandemic hit than before. Two-thirds of clinicians also valued self-administration methods for patients, such as auto-injectors for therapies or on-body devices.
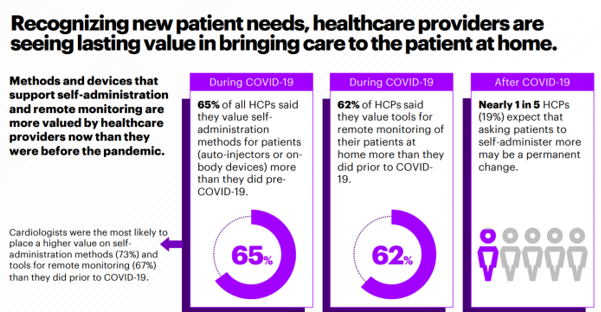 Doctors are embracing the value of bridging care to patients at home, with the home becoming the hub for living across peoples’ daily life-flows: for work, for school, for home-cooking, for religious services, and as a newfangled gym.
Doctors are embracing the value of bridging care to patients at home, with the home becoming the hub for living across peoples’ daily life-flows: for work, for school, for home-cooking, for religious services, and as a newfangled gym.
In addition to the home morphing into a site for patient care, Accenture points to care “more localized with delivery closer to home” as an outcome from the pandemic. Community centers, retail spaces, and other places “closer to home” will likely add to a more omni-channel approach to health care delivery I’ve been talking about in the pandemic era.
Finally, virtual doctors and visiting nurses will add to the portfolio of both delivery workflows and the diversifying patient care team envisioning safer and more convenient care direct-ot-patient.
 Health Populi’s Hot Points: Accenture’s general advice to the industry is that, “pharma companies need to move further, faster.” One aspect of this is going more virtual with sales teams, and creating content and engaging platforms that clinicians trust and find very relevant to their work and patient engagement.
Health Populi’s Hot Points: Accenture’s general advice to the industry is that, “pharma companies need to move further, faster.” One aspect of this is going more virtual with sales teams, and creating content and engaging platforms that clinicians trust and find very relevant to their work and patient engagement.
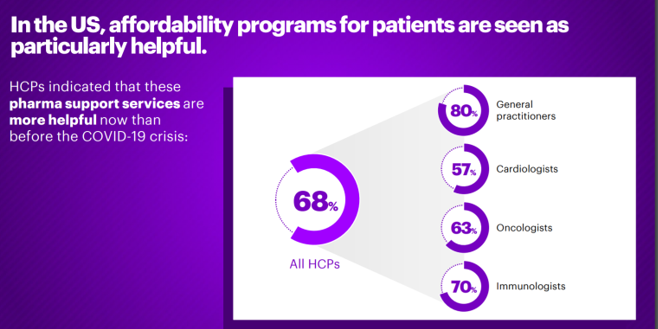
As patients-as-payors live through the COVID-19 pandemic, their financial well-being has also been impacted — and in the U.S., especially, as in other parts of the world governments have allocated more resources to keeping health citizens’ fiscal well-being more whole — by funding incomes and other safety net programs.
Thus, in the U.S., affordability programs for patients are particularly helpful, Accenture points out — as the last graphic attests.
Two-thirds of health care providers recognize that pharma support services are more helpful in the pandemic than before the crisis hit, especially keenly felt by general practitioners and immunologists. That six in ten oncologists perceived patient access programs are helpful in the pandemic is important because new oncologics launched in 2020 can be priced an average of $149,000 according to the 2019 forecast from IQVIA. Financial toxicity is a common side-effect for specialty drugs, and as U.S. consumers face higher out-of-pocket health costs, there is a greater risk for people to avoid filling prescriptions or delaying care. This is why artfully designing value-based health plans will be critical post-pandemic, to ensure that people have access to needed therapies and the services that surround them to bolster adherence and lower risks to lack of social determinants of health like nutritious food and broadband connections.
Accenture’s four-part prescription for pharma to emerge highly relevant in health care — for patients and physicians alike — are recommendations that were certainly useful pre-pandemic. Post-crisis, empathy, support, effective messaging for health literacy and trust-bolstering, and partnering in the community close-to and in peoples’ homes, are accelerated as strategic imperatives for healing health care in America.




 Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a