When it comes to patients, health care providers have been hit hard in two ways in the wake of the COVID-19 pandemic.
Hit #1 has been the direct negative impact of the coronavirus on health care volumes and patients not utilizing hospitals and doctors’ services, avoiding physical encounters in health care sites
Hit #2 has been the negative impact of patient experience for those health consumers who sought health care services during the pandemic — and had a negative response to the encounter.
 Accenture explored this phenomenon in their latest report, Elevating the Patient Experience to Fuel Growth.
Accenture explored this phenomenon in their latest report, Elevating the Patient Experience to Fuel Growth.
In the pandemic, consumers overall sought hygiene, safety, and comfort both within their homes and most assuredly when they left home to shop, go to school, or get health care.
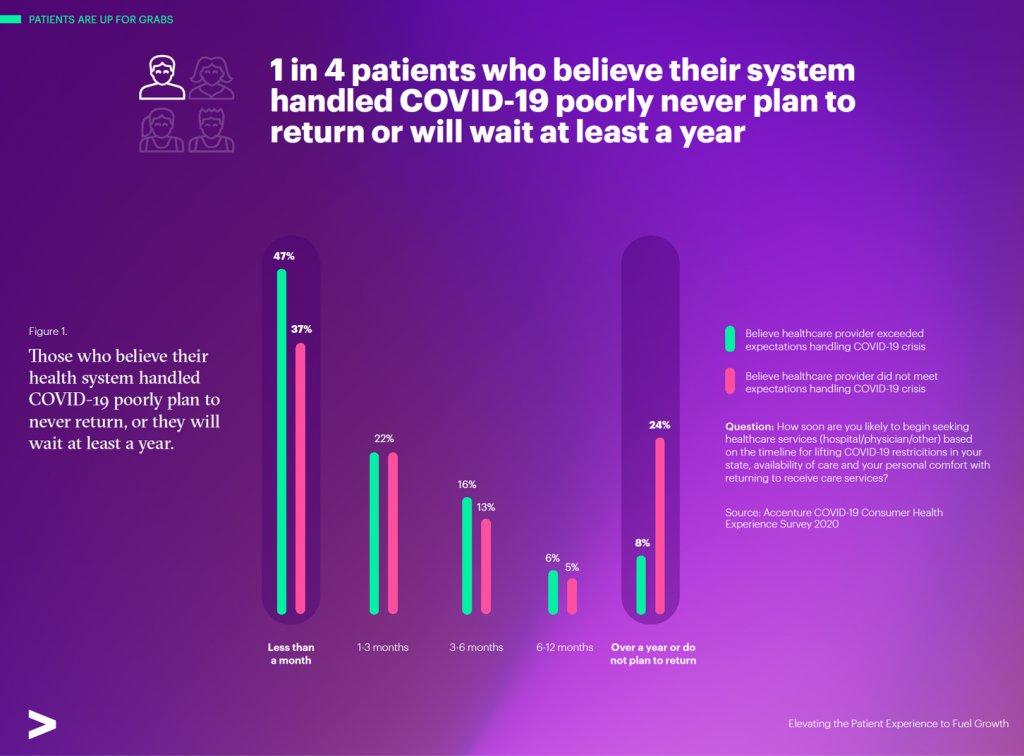
One in four patients who felt their health care system did not handle COVID-19 well
never plan to return to that provider, or they would wait at least one year to visit that health care site, the first chart from Accenture’s report illustrates on the right end of the graph.
To the left, we see that one-half of patients who believe their healthcare provider exceeded their expectations handling the coronavirus would return to the system within a month.
Let’s do some math that gives us pause in terms of patients’ willingness to return to health care — among those who felt their provider did a good job managing COVID-19. For those patients feeling positive about their provider’s handling of the virus, nearly 1 in three would not return to the health care provider for at least 3 months.
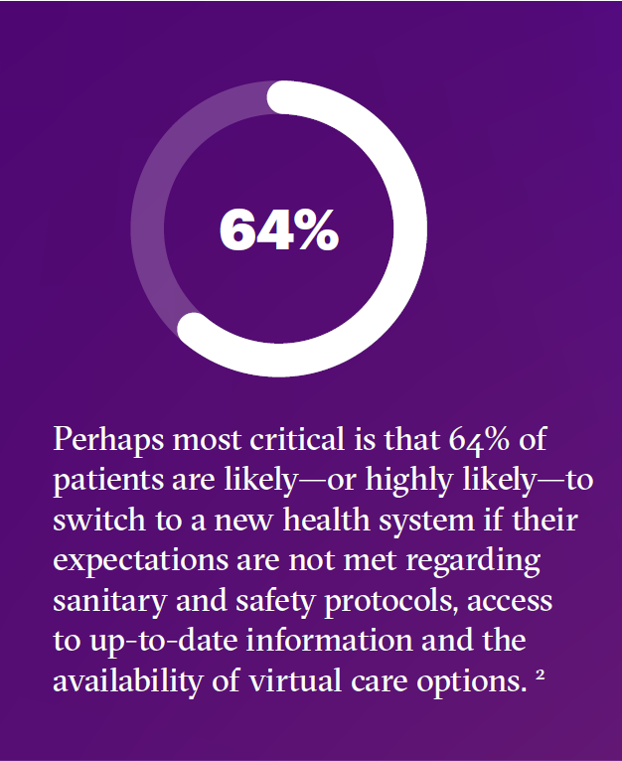
 “Poor customer experiences are costly,” Accenture warns. Quantifying that cost, Accenture modeled the negative patient experience cost to a $5 billion health system, calculating the difference between a poor and strong performing institution could be $900 million in net patient revenues over the coming year.
“Poor customer experiences are costly,” Accenture warns. Quantifying that cost, Accenture modeled the negative patient experience cost to a $5 billion health system, calculating the difference between a poor and strong performing institution could be $900 million in net patient revenues over the coming year.
“COVID-19 has increased the stakes and heightened urgency surrounding” consumer expectations, Accenture emphasized.
The pandemic has inspired and revealed new consumer needs that will persist “after” the pandemic wanes.
Accenture offers four recommendations to address the risks of negative patient experience in the evolving mindset of the post-COVID health consumer:
- Alleviate patient concerns with personalized messages. Patients prefer to receive those messages directly from their physicians than from health systems due to greater levels of trust in “my doctor.”
- Meet health consumers “at the front door.” This means designing and implementing digital front doors, such as appointment schedule, virtual waiting rooms, and form completion before walking through the literal entrance of the system.
- Enhance virtual care options. The public health crisis certainly launched a new era for telehealth and virtual care. Health systems must become omni-channel in terms of virtual care options, from text messaging and encrypted email systems to synchronous face-to-face telehealth visits with clinicians and other health professionals.
- Listen through social channels. Here, Accenture recommends that health care providers should do “social listening” to learn how patients feel (and what they’re saying in public social networks) about the pandemic, health information (like vaccine hesitancy and evidence-based medicine), and about the health system itself. By listening, the system can continuously learn about consumers’ pain-points and tweak services and the patient experience to improve it.
The bottom-line of this study is that two in three patients would switch out of the health system if their expectations weren’t being met — including hygiene and safety, information access, and virtual care options.
 Health Populi’s Hot Points: When I wrote HealthConsuming: From Health Consumer to Health Citizen last year, my thesis was that the patient had evolved into the payor, covering more out-of-pocket costs, high-deductibles, and greater financial exposure to medical costs.
Health Populi’s Hot Points: When I wrote HealthConsuming: From Health Consumer to Health Citizen last year, my thesis was that the patient had evolved into the payor, covering more out-of-pocket costs, high-deductibles, and greater financial exposure to medical costs.
This year, my book Health Citizenship: How a virus opened hearts and minds, explores the prospects for U.S. patients-as-health consumers to claim their health citizenship. The Accenture study on patient experience emphasizes the growing power of peoples’ self-agency in health care that patients feel in the wake of their pandemic experience. People-as-patients have been re-shaped into self-care health care consumers, with homes evolving as personal health hubs. And virtual platforms as digital front-doors have made care more convenient, safe, and in many ways, empowering.
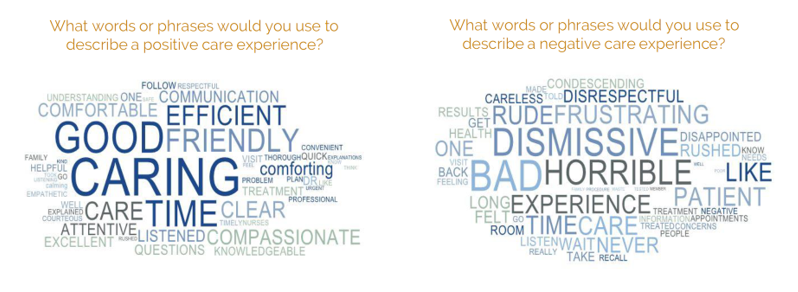
This builds on peoples’ growing muscles as health consumers seeking transparency and the right to safety, hygiene, and respect from their health systems.
Baking empathy and respect into health encounters will help health providers avoid the risk of health consumer-switch….which these organizations won’t be able to weather in the long-run.
For more on embedding empathy into health care processes, check out my post on the Beryl Institute-Ipsos research on the importance of designing respect into patient care.




 Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a